1. Jo I, Ahn Y, Lee J, Shin KR, Lee HK, Shin C. Prevalence, awareness, treatment, control and risk factors of hypertension in Korea: the Ansan study. J Hypertens. 2001; 19:1523–1532.
2. Bakris G, Sarafidis P, Agarwal R, Ruilope L. Review of blood pressure control rates and outcomes. J Am Soc Hypertens. 2014; 8:127–141.
3. Faria C, Wenzel M, Lee KW, Coderre K, Nichols J, Belletti DA. A narrative review of clinical inertia: focus on hypertension. J Am Soc Hypertens. 2009; 3:267–276.
4. Lemstra M, Alsabbagh MW. Proportion and risk indicators of nonadherence to antihypertensive therapy: a meta-analysis. Patient Prefer Adherence. 2014; 8:211–218.
5. Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA, Wong PK. Medication compliance and persistence: terminology and definitions. Value Health. 2008; 11:44–47.
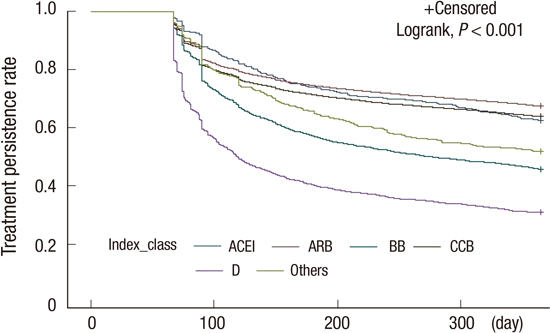
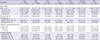
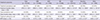
6. Hasford J, Schröder-Bernhardi D, Rottenkolber M, Kostev K, Dietlein G. Persistence with antihypertensive treatments: results of a 3-year follow-up cohort study. Eur J Clin Pharmacol. 2007; 63:1055–1061.
7. Jones JK, Gorkin L, Lian JF, Staffa JA, Fletcher AP. Discontinuation of and changes in treatment after start of new courses of antihypertensive drugs: a study of a United Kingdom population. BMJ. 1995; 311:293–295.
8. Tu K, Anderson LN, Butt DA, Quan H, Hemmelgarn BR, Campbell NR, McAlister FA. Hypertension Outcome and Surveillance Team. Antihypertensive drug prescribing and persistence among new elderly users: implications for persistence improvement interventions. Can J Cardiol. 2014; 30:647–652.
9. Mancia G, Zambon A, Soranna D, Merlino L, Corrao G. Factors involved in the discontinuation of antihypertensive drug therapy: an analysis from real life data. J Hypertens. 2014; 32:1708–1715.
10. Grimmsmann T, Himmel W. Persistence of antihypertensive drug use in German primary care: a follow-up study based on pharmacy claims data. Eur J Clin Pharmacol. 2014; 70:295–301.
11. Trimarco V, de Simone G, Izzo R, De Luca N, Giudice R, Marino M, Damiano S, Rozza F, Trimarco B, Di Renzo G. Persistence and adherence to antihypertensive treatment in relation to initial prescription: diuretics versus other classes of antihypertensive drugs. J Hypertens. 2012; 30:1225–1232.
12. Patel BV, Remigio-Baker RA, Mehta D, Thiebaud P, Frech-Tamas F, Preblick R. Effects of initial antihypertensive drug class on patient persistence and compliance in a usual-care setting in the United States. J Clin Hypertens (Greenwich). 2007; 9:692–700.
13. Sung SK, Lee SG, Lee KS, Kim DS, Kim KH, Kim KY. First-year treatment adherence among outpatients initiating antihypertensive medication in Korea: results of a retrospective claims review. Clin Ther. 2009; 31:1309–1320.
14. Han E, Suh DC, Lee SM, Jang S. The impact of medication adherence on health outcomes for chronic metabolic diseases: a retrospective cohort study. Res Social Adm Pharm. 2014; 10:e87–e98.
15. Mathes J, Kostev K, Gabriel A, Pirk O, Schmieder RE. Relation of the first hypertension-associated event with medication, compliance and persistence in naive hypertensive patients after initiating monotherapy. Int J Clin Pharmacol Ther. 2010; 48:173–183.
16. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–383.
17. Law M, Wald N, Morris J. Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy. Health Technol Assess. 2003; 7:1–94.
18. Mazzaglia G, Mantovani LG, Sturkenboom MC, Filippi A, Trifirò G, Cricelli C, Brignoli O, Caputi AP. Patterns of persistence with antihypertensive medications in newly diagnosed hypertensive patients in Italy: a retrospective cohort study in primary care. J Hypertens. 2005; 23:2093–2100.
19. Matchar DB, McCrory DC, Orlando LA, Patel MR, Patel UD, Patwardhan MB, Powers B, Samsa GP, Gray RN. Systematic review: comparative effectiveness of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers for treating essential hypertension. Ann Intern Med. 2008; 148:16–29.
20. Elliott WJ, Plauschinat CA, Skrepnek GH, Gause D. Persistence, adherence, and risk of discontinuation associated with commonly prescribed antihypertensive drug monotherapies. J Am Board Fam Med. 2007; 20:72–80.
21. Friedman O, McAlister FA, Yun L, Campbell NR, Tu K. Canadian Hypertension Education Program Outcomes Research Taskforce. Antihypertensive drug persistence and compliance among newly treated elderly hypertensives in ontario. Am J Med. 2010; 123:173–181.
22. van Wijk BL, Shrank WH, Klungel OH, Schneeweiss S, Brookhart MA, Avorn J. A cross-national study of the persistence of antihypertensive medication use in the elderly. J Hypertens. 2008; 26:145–153.
23. Hill MN, Miller NH, Degeest S, Materson BJ, Black HR, Izzo JL Jr, Oparil S, Weber MA. American Society of Hypertension Writing Group. Adherence and persistence with taking medication to control high blood pressure. J Am Soc Hypertens. 2011; 5:56–63.
24. Klootwyk J, Sanoski C. Medication adherence and persistence in hypertension management. J Clin Outcomes Manage. 2011; 18:351–358.
25. Elliott WJ. Improving outcomes in hypertensive patients: focus on adherence and persistence with antihypertensive therapy. J Clin Hypertens (Greenwich). 2009; 11:376–382.
26. Mazzaglia G, Ambrosioni E, Alacqua M, Filippi A, Sessa E, Immordino V, Borghi C, Brignoli O, Caputi AP, Cricelli C, et al. Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation. 2009; 120:1598–1605.
27. Kim HK, Park JH, Park JH, Kim JH. Differences in adherence to antihypertensive medication regimens according to psychiatric diagnosis: results of a Korean population-based study. Psychosom Med. 2010; 72:80–87.
28. Liu PH, Wang JD. Antihypertensive medication prescription patterns and time trends for newly-diagnosed uncomplicated hypertension patients in Taiwan. BMC Health Serv Res. 2008; 8:133.
29. McDowell SE, Coleman JJ, Ferner RE. Systematic review and meta-analysis of ethnic differences in risks of adverse reactions to drugs used in cardiovascular medicine. BMJ. 2006; 332:1177–1181.
30. Guertin JR, Jackevicius CA, Cox JL, Humphries K, Pilote L, So DY, Tu JV, Wijeysundera H, Rinfret S. Canadian Cardiovascular Outcomes Research Team. The potential economic impact of restricted access to angiotensin-receptor blockers. CMAJ. 2011; 183:E180–E186.
31. Selmer R, Blix HS, Landmark K, Reikvam A. Choice of initial antihypertensive drugs and persistence of drug use--a 4-year follow-up of 78,453 incident users. Eur J Clin Pharmacol. 2012; 68:1435–1442.
32. Larochelle P, Tobe SW, Lacourcière Y. β-Blockers in hypertension: studies and meta-analyses over the years. Can J Cardiol. 2014; 30:S16–S22.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download