Abstract
The aim of this study was to review the literature of latent papillary thyroid carcinomas (PTCs) discovered at autopsy and describe the available pathologic and demographic differences from a group of papillary thyroid microcarcinomas (PTMCs) the reported in a previous publication. We searched the PubMed for published articles describing latent thyroid carcinomas detected at autopsy. Meta-analysis was performed to identify differences between the clinicopathologic features of PTMCs analyzed previously in our institution (Group I) and those of latent PTCs described in autopsy studies (Group II). We identified 1,355 patients with PTMC (Group I) and 989 with latent PTCs (Group II). Mean patient age was 47.3 yr in Group I and 64.5 yr in Group II. The male:female ratio was 1:10.9 in Group I and 1:1 in Group II. Most PTMCs (67.6%) were larger than 0.5 cm in size, whereas most latent PTCs were <1-3 mm in diameter. The rates of multifocality were 24.7% in Group I and 30.5% in Group II, and the rates of cervical lymph node metastasis were 33.4% in Group I and 10.0% in Group II. Currently available data indicated that clinically evident PTMCs differ from latent PTCs detected at autopsy. Therefore, these two entities should be regarded as different.
Latent carcinomas are carcinomas found in autopsy specimens, and latent thyroid carcinomas are defined as tumors 1.5 cm or less in diameter and not suspected clinically (1). Although no autopsy studies of the Korean population have been published, a PubMed search of autopsy reports from the 1960s onwards revealed that small foci of thyroid carcinoma were often present in the thyroid glands of individuals who died of unrelated illness (2). However, few comparative studies have been performed, because of differences in definitions, the pathological sectioning techniques used, and the pathological criteria used to diagnose thyroid cancer (2).
The prevalence of latent thyroid carcinomas, which are frequently minute and occult, has been reported to range from 1.0% to 35.6% in different systematic autopsy series, this incidence is much higher than that of clinically evident carcinomas of the thyroid (1, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16). Papillary thyroid carcinoma (PTC) is a common thyroid malignancy, accounting for 86%-90% of thyroid cancer, and has indolent clinical characteristics. Papillary thyroid microcarcinomas (PTMCs), defined by the World Health Organization (WHO) as papillary thyroid carcinomas of maximum diameter of ≤1.0 cm (17), account for 30%-40% of PTCs, although recently their incidence is increasing rapidly (18). Most PTMCs are found incidentally, with some changing in clinical behavior to become clinical cancers (19).
At present, the relationship between latent PTCs and PTMCs is unclear, as in the treatment of patients with latent PTCs. There are two important questions with regard to latent PTCs. First, what is the relationship between latent papillary thyroid carcinomas and PTMC? Second, what should the therapeutic attitude be toward a patient in whom PTMC is discovered?
Because of the indolent behavior of PTMCs and the good prognosis of patients with these tumors, treatment of PTMCs is sometimes confused with that for latent PTCs. However, there is no evidence of similarity between PTMCs and latent PTCs. Despite this, autopsy studies have had a negative influence on the choice of therapy in patients with PTMC (20).
This study aimed to review the literature of latent PTCs discovered at autopsy and describe the available pathologic and demographic differences from a group of PTMCs the reported in a previous publication.
The clinicopathologic features of PTMCs have been described previously in the Korean Journal of Head & Neck Oncology in 2008 (18). Between January 2000 and December 2005, 1,355 patients with PTMC treated at the Thyroid Cancer Center, Yonsei University College of Medicine, Seoul, Korea were evaluated (Group I).
To identify patients with latent PTCs, the MEDLINE database was searched via the PubMed (http://www.ncbi.nih.gov/sites/entrez/) on 24 February 2011 for the MeSH headings "occult", "latent", and "thyroid cancer". We carefully reviewed all potentially relevant articles, and studies were included in the analysis if they met all of the following criteria: 1) including papillary thyroid carcinoma, 2) performing autopsy, 3) providing available clinicopathologic characteristics, 4) where participants always included general population of both sexes without age restriction, and 5) written in English.
Of the identified articles, 15 were included in this study (Table 1). These 15 papers described 8,619 autopsy specimens, 989 of which (11.5%) had latent PTCs (1, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16).
A meta-analysis was performed to identify differences between the clinicopathologic features of PTMCs evaluated in our institution (Group I) and those of latent PTCs evaluated in autopsy studies (Group II).
Categorical variables were summarized as counts and percentages, and continuous variables as means. Comparisons between PTMCs and latent PTCs were performed using the one sample t-test, assuming a mean age of 47.3 in patients with PTMCs, whereas Pearson's chi-square test was used to compare gender, tumor size (with cut-offs of 0.5 cm for PTMCs versus 1-3 mm cut-off value for latent PTCs), mutifocality, and cervical lymph node metastasis. All statistical analyses were performed using SAS 9.2 software (SAS Institute Inc., Cary, NC, USA). A P value less than 0.05 was considered statistically significant in all tests.
This study included 1,355 cases of PTMC (Group I) and 989 cases of latent PTCs from 15 autopsy reports (Group II). The clinicopathologic results of PTMCs reported in the Korean Journal of Head & Neck Oncology are listed in Table 2.
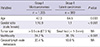
We compared the following variables between two groups; patient age, sex distribution, multifocality, and cervical lymph node metastasis. These variables and results of statistical analyses are listed in Table 3.
Mean patient age was 47.3 yr in Group I and 65.4 yr in Group II (P=0.003), and sex distribution (male:female) was 1:10.9 in Group I and 1:1 in Group II (P<0.001) with statistical significance.
Tumor diameter was not comparable between the two groups: the majority (67.3%) of patients in Group I had tumors larger than 0.5 cm in diameter, and whereas tumors with tiny diameters that were described as small foci (<1-3 mm) were common in Group II.
Multifocality was significantly less frequent in Group I than in Group II (24.7% vs 30.5%, P<0.001). The rates of cervical lymph node metastasis rate were higher in Group I than in Group II (33.4% vs 10.0%) but the difference was not statistically significant.
Of the 8,619 thyroid glands obtained in 15 autopsy studies, 989 (11.5%) were positive for latent PTC (Table 1). However, the prevalence of latent PTC has been found to vary considerably, from 1.0% to 35.6%. Comparing this prevalence among autopsy studies is complicated by differences in methods of examination, section intervals (ranging from 4 µm to 4 mm), diagnostic criteria, and sample selection. In particular, different methods of examination can have a profound effect on the observed prevalence of carcinoma (1).
One factor that may cause a spurious increase in the rate of latent PTC at autopsy is bias of the entire series in favor of thyroid carcinoma or a related disease (1). We, however, did not directly select for PTC at autopsy, because almost all of the latent carcinomas were small and clinically occult. There also was no evidence of indirect selection for patients with thyroid carcinoma. Another factor related to an increased prevalence rate is that the incidence of thyroid carcinoma is fundamentally very high.
This can be explained by the two-stage theory. A thyroid carcinoma may arise in response to various factors, including environmental and genetic factors, but its growth may be deficient and it may lack clinical characteristics. Subsequently, other factors may promote the development of clinical thyroid carcinoma (21, 22). This two-stage theory explains the small size, described as foci, and the sclerotic characteristics of the latent PTCs.
The latent PTC group contained a high proportion of very small tumors. Most (67.3%) patients with PTMC had tumors larger than 0.5 cm in diameter, whereas most latent PTCs were small foci (<1-3 mm in size). Moreover, most of the latent PTCs showed sclerotic patterns, indicating that these tumors had arisen a long time prior to autopsy.
Papillary carcinomas arise as non-sclerosing tumors; during further growth, stromal fibrosis (non-encapsulated sclerosing tumors) occurs or a fibrous capsule (encapsulated tumors) forms with various degrees of cellular infiltration, with the latter likely associated with a host reaction (10).
In contrast to the marked female predominance of clinical thyroid carcinoma, the prevalence of latent carcinomas did not differ significantly between men and women. Also, whereas most hospital-based series have found a slight male predominance, we observed a 1:1 ratio of latent PTCs in males and females. Moreover, patients with latent PTC were older than those with PTMC. Older age and male predominance, however, may be caused by a selection bias in patients with latent PTCs, since these studies were based on autopsy data.
Multifocality was significantly more prevalent in patients with latent PTC than in those with PTMC (30.5% vs 24.7%, P<0.001). In contrast, cervical lymph node metastasis was more prevalent in patients with PTMC than in those with latent PTC (33.4% vs 10.0%), probably because lymph node status was not fully examined in autopsy studies.
In conclusion, despite the limited ability to compare variables between patient with PTMC and those with latent PTC, and despite selection bias, there are differences between these groups, indicating that latent PTCs and PTMCs should be considered distinct entities. The choice of therapy in patients with PTMC should not be influenced by the concept of latent PTCs. Future autopsy studies should include molecular and metabolic markers.
Notes
References
1. Sampson RJ, Key CR, Buncher CR, Iijima S. Thyroid carcinoma in Hiroshima and Nagasaki: I. prevalence of thyroid carcinoma at autopsy. JAMA. 1969; 209:65–70.
2. Bramley MD, Harrison BJ. Papillary microcarcinoma of the thyroid gland. Br J Surg. 1996; 83:1674–1683.
3. Fukunaga FH, Yatani R. Geographic pathology of occult thyroid carcinomas. Cancer. 1975; 36:1095–1099.
4. Sampson RJ, Woolner LB, Bahn RC, Kurland LT. Occult thyroid carcinoma in Olmsted County, Minnesota: prevalence at autopsy compared with that in Hiroshima and Nagasaki, Japan. Cancer. 1974; 34:2072–2076.
5. Sobrinho-Simôes MA, Sambade MC, Gonçalves V. Latent thyroid carcinoma at autopsy: a study from Oporto, Portugal. Cancer. 1979; 43:1702–1706.
6. Bondeson L, Ljungberg O. Occult thyroid carcinoma at autopsy in Malmö, Sweden. Cancer. 1981; 47:319–323.
7. Arellano L, Ibarra A. Occult carcinoma of the thyroid gland. Pathol Res Pract. 1984; 179:88–91.
8. Harach HR, Franssila KO, Wasenius VM. Occult papillary carcinoma of the thyroid: a "normal" finding in Finland: a systematic autopsy study. Cancer. 1985; 56:531–538.
9. Ottino A, Pianzola HM, Castelletto RH. Occult papillary thyroid carcinoma at autopsy in La Plata, Argentina. Cancer. 1989; 64:547–551.
10. Yamamoto Y, Maeda T, Izumi K, Otsuka H. Occult papillary carcinoma of the thyroid: a study of 408 autopsy cases. Cancer. 1990; 65:1173–1179.
11. Bisi H, Fernandes VS, de Camargo RY, Koch L, Abdo AH, de Brito T. The prevalence of unsuspected thyroid pathology in 300 sequential autopsies, with special reference to the incidental carcinoma. Cancer. 1989; 64:1888–1893.
12. Martinez-Tello FJ, Martinez-Cabruja R, Fernandez-Martin J, Lasso-Oria C, Ballestin-Carcavilla C. Occult carcinoma of the thyroid: a systematic autopsy study from Spain of two series performed with two different methods. Cancer. 1993; 71:4022–4029.
13. Furmanchuk AW, Roussak N, Ruchti C. Occult thyroid carcinomas in the region of Minsk, Belarus: an autopsy study of 215 patients. Histopathology. 1993; 23:319–325.
14. Kovács GL, Gonda G, Vadász G, Ludmány E, Uhrin K, Görömbey Z, Kovács L, Hubina E, Bodó M, Góth MI, et al. Epidemiology of thyroid microcarcinoma found in autopsy series conducted in areas of different iodine intake. Thyroid. 2005; 15:152–157.
15. Neuhold N, Kaiser H, Kaserer K. Latent carcinoma of the thyroid in Austria: a systematic autopsy study. Endocr Pathol. 2001; 12:23–31.
16. Chong PY. Thyroid carcinomas in Singapore autopsies. Pathology. 1994; 26:20–22.
17. Hedinger C, Williams ED, Sobin LH. The WHO histological classification of thyroid tumors: a commentary on the second edition. Cancer. 1989; 63:908–911.
18. Lee JD, Oh DK, Lim SS, Nam KH, Chung WY, Soh EY, Park CS. Clinical behaviors and treatment outcomes of papillary thyroid microcarcinomas: tumor size-based therapeutic concept. Korean J Head Neck Oncol. 2008; 24:47–52.
19. Lee J, Yun JS, Nam KH, Chung WY, Soh EY, Park CS. Papillary thyroid microcarcinoma: clinicopathologic characteristics and treatment strategy. J Korean Surg Soc. 2007; 72:276–282.
20. Mazzaferri EL. Managing thyroid microcarcinomas. Yonsei Med J. 2012; 53:1–14.
21. Hall WH. The role of initiating and promoting factors in the pathogenesis of tumors of the thyroid. Br J Cancer. 1948; 2:273–280.
22. Sampson RJ, Key CR, Buncher CR, Iijima S. Smallest forms of papillary carcinoma of the thyroid: a study of 141 microcarcinomas less than 0.1 cm in greatest dimension. Arch Pathol. 1971; 91:334–339.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download