Abstract
Depression during adolescence is critical to the individual's own development. Hence, identifying individuals with high-risk depression at an early stage is necessary. This study aimed to identify childhood emotional and behavioral risk factors related to depressive symptoms in Korean adolescents through a longitudinal study. The first survey took place from 1998 to 2000, and a follow-up assessment conducted in 2006, as the original participants reached 13-15 yr of age. The first assessment used the Korean version of Child Behavior Checklist and a general questionnaire on family structure, parental education, and economic status to evaluate the participants. The follow-up assessment administered the Korean Children's Depression Inventory. Multiple regression analysis revealed that childhood attention problems predicted depressive symptoms during adolescence for both boys and girls. For boys, family structure also predicted adolescent depressive symptoms. This study suggests that adolescents with attention problems during childhood are more likely to experience depressive symptoms.
Depression, as one of the most common psychiatric problems in adolescence, has a lifetime prevalence rate of around 15%-20% (1). The prevalence rate of depression jumps from less than 3% to 9%, aging from prepubertal childhood (aged 6-11 yr) to ages 12-16 yr (2, 3). According to various studies, by ages 15-18 yr, the rate sharply increases (4): an implication that adolescence is a vulnerable stage correlated to depression. Many studies have shown that adolescents with depression have co-occurring anxiety disorders, conduct disorders, and eating disorders (5-6). Several studies show that depression during adolescence is a risk factor of academic failures, marriage struggles, suicide attempts, interpersonal conflicts, unemployment, drug abuse, and delinquency; it is also a strong predictor of adulthood depression (1, 5, 7). Subdiagnostic depression during adolescence also has been linked to an onset of psychiatric disorders, drug abuse, academic problems, social skills, and suicide attempts (8). Adolescent depression and depressive symptoms can interfere with shaping individual's developments.
Research on risk factors presents an effective standard for identifying individuals at high-risk of depression. It is further studied due to its potent prevention of depression through an early-stage intervention. Gender, stressful life events (9, 10), negative affectivity (11), deficits in social support (9, 10), and externalizing behaviors (12) are risk factors usually presented in studies regarding adolescent depression. Gender, in particular, is a crucial factor to consider as the prevalence of depression in adolescent girls is 1.5-3 times higher than that of adolescent boys (13).
Although researchers have conducted a number of studies of risk factors for adolescent depression, the findings are quite inconsistent and the prospective association between psychological problems in childhood and depression is still under debate. Moreover, most studies of adolescent depression use Caucasian samples (14); therefore, data regarding risk factors of depression among adolescents in Asia are notably scarce. However, several studies on the depression of Asian adolescents suggested the existence of cultural differences on adolescent depression. Some studies represented that Asians demonstrated more persistent symptoms of depression compared to European Americans (15), whereas others found lower depression rates in Asian adolescents (16). Some researchers suggested that low rates of depression among Asian adolescents may be related to the somatization tendency of emotional problems (17, 18). A recent cross-sectional study showed that Asian adolescents had higher prevalence of depressed symptoms, yet, similar risk factors as Caucasians; i.e., female gender, perceived low parental interest in feelings, failing grades, worry about failing grades, and cigarette smoking (19). As few have carried out longitudinal studies on the developmental associations between emotional, behavioral, and environmental problems in early childhood and adolescent delinquency in Asia, recognizing the risk factors associated with depressive symptoms in Asian youth is necessary to provide a culture-specific mental health service.
In this study, we used data from a longitudinal sample, followed from childhood (age 7) to adolescence (ages 13-15), in order to identify early childhood risk factors correlated with adolescent depressive symptoms. We investigated in detail whether there were any significant gender differences among such adolescents.
This study was based on the data derived from a longitudinal study on child psychiatric disorders in Osan, a small city located 50 kilometers (about 30 miles) southeast of Seoul, and having similar socioeconomic profile to the national average. During a periodic health examination, a survey was performed by the Child Mental Health Care Center. The data were collected in two separate instances (1998-2000 and 2006). The first assessment was conducted with teachers' and parents' approval from the years 1998 to 2000. All of the first grade children at eight primary schools were recruited for the study, resulting in a study group of 3,808 pupils. A follow-up assessment was performed in 2006 when the original subjects became middle school students. The center performed the follow-up assessment, comprising of two stages. In the first stage, all 14- to 16-yr old adolescents who were living in Osan city were requested to complete the questionnaire with parental consent. The total number of subjects was 5,670. After the adolescents completed the questionnaire, their personal information was compared to the data obtained in 1998-2000. Among the students, 1,821 had participated in the first assessment. The retention rate was 47.8%, and the mean age of the children at the first assessment was 6.85 yr (SD=0.41); at the second assessment, the mean age was 13.75 yr (SD=1.0). Omitted answers were excluded from analyses, and thus, a total of 1,659 data were used for the analyses of the study. The dropout analyses showed no significant differences with gender
At baseline, the children's parents completed questionnaires, including the Korean version of the Child Behavior Checklist (K-CBCL) (20), regarding their own children and demographic information: age, gender, family structure, and economic status. The K-CBCL is a parent-report questionnaire consisting of 119 items with the total problem scale divided into eight syndrome scales: withdrawn, somatic complaints, anxious/depressed, social problems, thought problems, attention problems, delinquent behavior, and aggressive behavior. This instrument has been frequently used to evaluate social adjustment and emotional and behavioral problems of children. Each child was sent home with a K-CBCL to be completed by the parents and was collected after 3 to 5 days.
At the 6- to 8-yr follow-up, researchers requested participants to complete the Korean version of Children's Depression Inventory (K-CDI), which is a 27-item self-rated depression symptom oriented scale. This instrument was developed based on the Beck Depression Inventory (BDI) in order to identify adolescents with diagnoses of major depressive or dysthymic disorder (21).
First, we used the chi-square test to examine differences in the economic status by gender; while the non-parametric Fisher's exact test was used to analyze the family structure and K-CDI score by gender. Second, we selected independent variables for multiple regression from the correlations of K-CDI score and K-CBCL's syndrome scale (less than P values<0.2 chosen as the independent variables) (22). Lastly, we measured the childhood risk factor, an effective predictor of adolescent depressive symptoms, through multiple regression analysis. All statistical tests were two-sided. Statistical analysis PASW statistics software version 18.0 (SPSS Inc., Chicago, IL, USA) was used for data entry and statistical analyses.
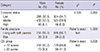
Of the 1,659 participants, 782 were boys (47.1%), and 877 were girls (52.9%). Comparisons revealed that family economic status (χ2=2.535, df=2, P=0.282), family structure (P=1.000), and frequency, which scored K-CDI above the cut-off (P=0.226), showed no statistically significant differences between genders (Table 1).
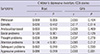
Following the correlation analysis, the variables among the K-CBCL syndrome scale, which showed correlation with K-CDI at the P<0.2 level, were chosen as the independent variables of the multiple regression (Table 2). Withdrawn (r=0.069, P=0.055), anxious/depressed (r=0.093, P=0.010), social problems (r=0.120, P=0.001), attention problems (r=0.136, P< 0.001), delinquent problems (r=0.092, P=0.010), and aggressive problems syndrome scale (r=0.086, P=0.019) were included as the independent variables for boys, whereas withdrawn (r=0.055, P=0.104), social problems (r=0.052, P=0.126), and attention problems syndrome scale (r=0.085, P=0.012) were chosen for girls. Additionally, family structure and family economic status were selected as the predicting factors of the multiple regression analysis.
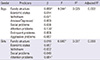
We investigated childhood factors associated with adolescent depressive symptoms. Analysis showed that attention problems (β=0.130, P<0.001) and family structure (β=0.080, P=0.030) at age 7 yr predicted depressive symptoms of boys 6-8 yr later. The regression model, factoring in attention problems and family structure, showed a 2.5% explanatory power regarding the K-CDI scores in boys (R2=0.025, P<0.001). For girls, only attention problems (β=0.084, P=0.014) at age 7 yr predicted the depressive symptoms of girls with a 0.7% explanatory power (Table 3).
This study attempted to examine childhood emotional and behavior factor related to adolescents' depressive symptoms by gender via a longitudinal study. The summary is as follows. First, applying the CDI cut off score of 22, 10.3% of all subjects scored above the cut off, displaying possibilities of depression. This result complies with the previous studies' outcome of 9% in adolescents between the ages of 12-16 (2, 3). On the other hand, there was no difference in K-CDI scores by gender. In adults, one of the most common and reliable findings in psychiatric epidemiology is that depression is twice more likely and severe in females than in males. These findings did not apply until mid-adolescence; moreover, the period when gender difference begins to emerge was not definite (23). Several studies have investigated about the gender gap of adolescent depression. Angold and Rutter (24) represented that depression rate was similar between genders under age 11 yr; however, between ages 14 to 16, girls were twice as likely to have symptoms of depression as boys. Likewise, a study in New Zealand found that the small gender gap in the rates of depressive disorders became evident between the ages of 13 to 15, and the greatest differences emerged between ages 15 and 18 (4). Previous studies in Korea also showed that the gender difference of depression began to emerge in middle school ages with continuity into high school ages (25, 26). On the other hand, some studies in Korea represented that gender differences in depression started to appear in grades 7 and 8; however, gender gaps were not statistically significant in high school students (27, 28). The participants' ages of this study ranged from ages 12 to 15 with an average age of 13.75: this age group is within the spectrum of emergence in gender difference in previous studies. Our study also did not reveal any gender difference in the K-CDI score, indicating that the gender difference of depressive symptoms in Korean adolescents may be dissimilar to that of other regions and cultures.
Second, attention problem at age 7 predicted the depressive symptoms 6-8 yr later regardless of gender. A total of 16%-37% of adults with attention deficit/hyperactivity disorders (ADHD), who are referred to a clinical setting, experience major depressive disorder or dysthymia (29). Many studies, investigating the association between depression and ADHD history, have been undertaken, yet, there are inconsistent findings. Several longitudinal studies showed that childhood ADHD had no observable influence on the onset of major depressive disorder in adolescence or early-adulthood (30, 31). Nonetheless, few studies stated differently. Hinshaw et al. (32) reported that girls with ADHD more often displayed depressive symptoms. A 13-yr longitudinal study showed that children with ADHD were more likely to meet the criteria for major depressive disorder during adolescence or early adulthood (33). Similarly, a recent study showed that more children with ADHD reported suicidal ideation and attempts during high school than controls (34). As diagnostic criteria for depressive episode include 'diminished ability to think or concentrate', attention problem could be regarded as one of depressive symptoms. However, we controlled anxious/depressed symptoms using K-CBCL, a tool assess comprehensively child's psychological problems. In this study, among various emotional and behavioral problems during childhood, only the attention problems significantly predicted depressive symptoms in adolescence. Children who have trouble paying attention and controlling impulsive behaviors are often hyperactive. This can cause poor performance in school, negative feedback from teacher or parents, difficulties in peer relationship, and low self-esteem. This result suggests that children with attention problems need close attention to their experience and its consequences to prevent possible long-term problems.
Third, depressive symptoms in male adolescents were affected not only by attention problems, but also by the family structure during childhood. Notably, juvenile depressive symptoms risk factors in girls contained only the individual factors. Socio-demographic factors, including family structure and economic status, did not significantly predict depression in girls. On the other hand, boys were more sensitive to environmental factors than girls were. The fact that boys who did not live with both parents were likely to show depressive symptoms 6-8 yr later, implying that boys respond more to the environmental support than girls do. This result is not consistent with that of previous reports in which the environment has a higher influence on girls than on boys (35). However, considering a study regarding social phobia in girls, such phobia was affected by struggles with parents during the developmental phase while for boys, the absence of a close relationship with a parent or other adult figure during childhood was correlated with social phobia (36). Family structure shaping psychiatric disorder development depends on both quantitative and qualitative characteristics as well as gender. Another possible explanation is that for boys, emotional distress was manifested as an attention problem. As depressed children display irritability and inattention rather than sadness, accurately identifying childhood attention problems and emotional problems is difficult (37). Therefore, depression of children may be misdiagnosed as ADHD, which corresponds with the study that depressed children are more likely to be diagnosed with ADHD than non-depressed children (38). Moreover, considering that boys with ADHD have higher comorbidity with depression than do girls (39), emotional distress arising from an unstable family structure might be expressed as an attention problem.
Although attention problem and family structure during childhood were predicted as the depressive symptoms in adolescence, their explanatory powers are quite low (girls, 0.7%; boys, 2.5%). The implication of this result is that other traditional factors, such as stressful life events, deficits in social support, and attribution style, must be considered along with childhood emotional and behavioral factors in order to predict depressive symptoms during adolescence (9, 10).
The present study has several limitations. First, only 47.8% of the original subjects participated in the follow-up assessment. Second, the intervals between the first assessment and the follow-up assessments were not consistent: 6 to 8 yr. Third, the findings regarding depressive symptoms, socio-demographic factors, and childhood behavioral and emotional problems relied on self-reported information. In addition, the information source differed between assessments: parents completed the first survey, while participants completed the follow-up survey themselves. Thus, person-to-person interviews with structured formats should be featured in a future study in order to insure objective and consistent data.
Despite these limitations, the strength of this study is that it is a community-based longitudinal study with a large sample size for investigating the risk factors of depressive symptoms of adolescents in Korea. In addition, the comprehensive measure, including various emotional and behavioral factors in childhood, was used to identify factors that were related to depressive symptoms of adolescents. In conclusion, this study suggests that attention problem is the most important risk factor among various emotional and behavioral problems during childhood, predicting depressive symptoms among adolescents regardless of gender.
Figures and Tables
References
1. Birmaher B, Ryan ND, Williamson DE, Brent DA, Kaufman J, Dahl RE, Perel J, Nelson B. Childhood and adolescent depression: a review of the past 10 years: part I. J Am Acad Child Adolesc Psychiatry. 1996; 35:1427–1439.
2. Fleming JE, Offord DR. Epidemiology of childhood depressive disorders: a critical review. J Am Acad Child Adolesc Psychiatry. 1990; 29:571–580.
3. Kaltiala-Heino R, Rimpelä M, Rantanen P, Laippala P. Adolescent depression: the role of discontinuities in life course and social support. J Affect Disord. 2001; 64:155–166.
4. Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: emerging gender differences in a 10-year longitudinal study. J Abnorm Psychol. 1998; 107:128–140.
5. Fergusson DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Arch Gen Psychiatry. 2002; 59:225–231.
6. Lewinsohn PM, Rohde P, Klein DN, Seeley JR. Natural course of adolescent major depressive disorder: I. continuity into young adulthood. J Am Acad Child Adolesc Psychiatry. 1999; 38:56–63.
7. Ge X, Conger RD, Elder GH Jr. Pubertal transition, stressful life events, and the emergence of gender differences in adolescent depressive symptoms. Dev Psychol. 2001; 37:404–417.
8. Capaldi DM, Stoolmiller M. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: III. prediction to young-adult adjustment. Dev Psychopathol. 1999; 11:59–84.
9. Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. prevalence and incidence of depression and other DSM-III-R disorders in high school students. J Abnorm Psychol. 1993; 102:133–144.
10. Windle M. A longitudinal study of stress buffering for adolescent problem behaviors. Dev Psychol. 1992; 28:522–530.
11. Gjone H, Stevenson J. A longitudinal twin study of temperament and behavior problems: common genetic or environmental influences? J Am Acad Child Adolesc Psychiatry. 1997; 36:1448–1456.
12. Fergusson DM, Wanner B, Vitaro F, Horwood LJ, Swain-Campbell N. Deviant peer affiliations and depression: confounding or causation? J Abnorm Child Psychol. 2003; 31:605–618.
13. Ge X, Lorenz FO, Conger RD, Elder GH, Simons RL. Trajectories of stressful life events and depressive symptoms during adolescence. Dev Psychol. 1994; 30:467–483.
14. Stewart SM. Methods in cross-cultural psychopathology. In : McKay D, editor. Handbook of research methods in abnormal and clinical psychology. New York: SAGE;2008. p. 447–467.
15. Brown JS, Meadows SO, Elder GH Jr. Race-ethnic inequality and psychological distress: depressive symptoms from adolescence to young adulthood. Dev Psychol. 2007; 43:1295–1311.
16. Saluja G, Iachan R, Scheidt PC, Overpeck MD, Sun W, Giedd JN. Prevalence of and risk factors for depressive symptoms among young adolescents. Arch Pediatr Adolesc Med. 2004; 158:760–765.
17. Anderson ER, Mayes LC. Race/ethnicity and internalizing disorders in youth: a review. Clin Psychol Rev. 2010; 30:338–348.
18. Karasz A. Cultural differences in conceptual models of depression. Soc Sci Med. 2005; 60:1625–1635.
19. Song SJ, Ziegler R, Arsenault L, Fried LE, Hacker K. Asian student depression in American high schools: differences in risk factors. J Sch Nurs. 2011; 27:455–462.
20. Oh K, Lee H, Hong K, Ha E. Korean version of the Child behavior Checklist (K-CBCL). Seoul: Chung Ang Aptitude Publishing Co.;1997.
21. Kovacs M. The Children's Depression Inventory (CDI). New York: Multi-Health Systems;1992.
22. Katz MH. Multivariable analysis: a practical guide for clinicians. Cambridge: Cambridge University Press;1999.
23. Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression during adolescence. Psychol Bull. 1994; 115:424–443.
24. Angold A, Rutter M. Effects of age and pubertal status on depression in a large clinical sample. Dev Psychopathol. 1992; 4:5–28.
25. Choi IJ. The effects of parent-adolescent communication on adolescent's self-differentiation, depression and anxiety. Korean J Clin Psychol. 2007; 26:611–628.
26. Ha EH, Oh KJ, Song DH. Psychosocial risk factors for comorbid adolescents with depression and anxiety. Korean J Psychol Gen. 2003; 22:127–144.
27. Kim MY, Kang YJ. Depression and related factors for adolescents. J Korean Soc Sch Health. 2000; 13:261–270.
28. Shin M, Chung KM, Kim ES. Gender differences in depression and anxiety among Korean adolescents: onset and developmental change. Korean J Clin Psychol. 2012; 31:93–114.
29. Murphy KR, Barkley RA, Bush T. Young adults with attention deficit hyperactivity disorder: subtype differences in comorbidity, educational, and clinical history. J Nerv Ment Dis. 2002; 190:147–157.
30. Bagwell CL, Molina BSG, Kashdan TB, Pelham WE, Hoza B. Anxiety and mood disorders in adolescents with childhood attention-deficit hyperactivity disorder. J Emot Behav Disord. 2006; 14:178–187.
31. Claude D, Firestone P. The development of ADHD boys: a 12-year follow-up. Can J Behav Sci. 1995; 27:226–249.
32. Hinshaw SP, Owens EB, Sami N, Fargeon S. Prospective follow-up of girls with attention-deficit/hyperactivity disorder into adolescence: evidence for continuing cross-domain impairment. J Consult Clin Psychol. 2006; 74:489–499.
33. Fischer M, Barkley RA, Smallish L, Fletcher K. Young adult follow-up of hyperactive children: self-reported psychiatric disorders, comorbidity, and the role of childhood conduct problems and teen CD. J Abnorm Child Psychol. 2002; 30:463–475.
34. Chronis-Tuscano A, Molina BS, Pelham WE, Applegate B, Dahlke A, Overmyer M, Lahey BB. Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2010; 67:1044–1051.
35. Cyranowski JM, Frank E, Young E, Shear MK. Adolescent onset of the gender difference in lifetime rates of major depression: a theoretical model. Arch Gen Psychiatry. 2000; 57:21–27.
36. DeWit DJ, Chandler-Coutts M, Offord DR, King G, McDougall J, Specht J, Stewart S. Gender differences in the effects of family adversity on the risk of onset of DSM-III-R social phobia. J Anxiety Disord. 2005; 19:479–502.
37. De Mesquita PB, Gilliam WS. Differential diagnosis of childhood depression: using comorbidity and symptom overlap to generate multiple hypotheses. Child Psychiatry Hum Dev. 1994; 24:157–172.
38. McClellan JM, Rupert MP, Reichler RJ, Sylvester CE. Attention deficit disorder in children at risk for anxiety and depression. J Am Acad Child Adolesc Psychiatry. 1990; 29:534–539.
39. Biederman J, Mick E, Faraone SV, Braaten E, Doyle A, Spencer T, Wilens TE, Frazier E, Johnson MA. Influence of gender on attention deficit hyperactivity disorder in children referred to a psychiatric clinic. Am J Psychiatry. 2002; 159:36–42.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download