Abstract
Subclinical hypothyroidism (SCH) is a common clinical condition, whereas it's natural course has not been identified distinctly. We evaluated the natural history of 169 SCH patients over 5-yr and the prognostic factors including thyroid autoantibodies and thyroid ultrasonographic (USG) findings related to develop overt hypothyroidism. After 5 yr, 47.3% of patients showed normalization of TSH, while 36.7% of patients remained persistence of high level of TSH, and overt hypothyroidism developed in 11.2% of patients. There were painless thyroiditis (2.9%) and hyperthyroidism (1.7%) during 5 yr follow-up. The thyroid nodule was seen in 48.6% of patients. Most of patients had 1 to 2 nodules whereas only 3% of patients with thyroid nodule had more than 6 nodules. Overt hypothyroidism patients had more heterogenous echogenecity in USG compared to patients with normalization or persistent SCH (76.5% vs 50.0% vs 35.0%, P = 0.048) and higher prevalence positive anti-thyroid peroxidase (anti-TPO Ab) and anti-thyroglobulin antibody (anti-Tg Ab) and titer of anti-TPO Ab than other two groups. The cut off values for prediction of overt hypothyroidism were TSH > 7.45 µIU/mL, free T4 < 1.09 ng/dL and Anti-TPO Ab > 560 IU/mL. SCH has various courses and initial TSH, free T4, presence of thyroid autoantibody, titer of thyroid autoantibody; and thyroid USG findings can serve as a prognostic factor for progression of overt hypothyroidism. These parameters suggest consideration to initiate thyroid hormone treatment in SCH.
Subclinical hypothyroidism (SCH) is defined as the clinical state with higher serum thyroid stimulation hormone (TSH) concentration than the statistically defined upper limit of the reference value when serum free T4 concentration is within its reference range (1). The prevalence of SCH is continuously increasing; it might be related with the development of TSH assay and frequent routine checking of TSH in regular health surveillance for general population. The prevalence of SCH is between 4% to 10% in general population and it is more common in woman with their older than 60s (2, 3). Although SCH have been shown clinical association with several health problems such as, hyperlipidemia, cardiac dysfunction, mood disorder and overt hypothyroidism, research findings have not consistently supported these concerns (4-8). Several studies show the different results of treating subclinical hypothyroidism, and it leads to no establishment of standard consensus to treat subclinical hypothyroidism (9-14). There are some clinical follow-up observations for SCH, but they have important limitation to generalize of their data in the aspects of short duration of follow-up and very limited number of patients (15, 16). Heterogenous echo pattern or decreased echogenicity on thyroid ultrasonography (USG) are indicative of several forms of autoimmune thyroiditis and are associated with thyroid dysfunction including overt hypothyroidism and SCH (17, 18). The usefulness of performing routine thyroid USG in patients with SCH continues to be debated.
In this study, we prospectively investigated the natural course of SCH in Korean population during a follow-up period of 5 yr and the prognostic factors including thyroid autoantibodies and thyroid ultrasonographic findings related to develop overt hypothyroidism.
The study enrolled 197 patients who were diagnosed SCH at the endocrinology department in Chungbuk National University from 2005 to 2006. Twenty patients were excluded due to pregnancy and follow-up loss. Thyroid cancer was diagnosed in 8 patients of 177 patients (4.5%) at the beginning of the study. Ultimately, a total of 169 patients with SCH was subjected to this study.
The diagnostic criteria of SCH was defined as patients having free T4 between 0.89-1.79 ng/dL with TSH > 4.05 µIU/mL (reference range: 0.17-4.05 µIU/mL). Overt hypothyroidism was defined as patients having low free T4 below 0.89 ng/dL and elevated TSH above 4.05 µIU/mL. Serum TSH, free T4 and T3 were repeated at an interval of 2 weeks before enrolling the study to minimize assay variation or fluctuation. The exclusion criteria were defined as patients conditions or taking medications, which affect thyroid functions, including pregnancy, female hormone therapy, thyroid hormone therapy, methimazole, carbimazole, prophylthiouracil, amiodarone, lithium and dopamine antagonist. Also patients with normal free T4 and TSH over 10 µIU/mL who complained of fatigue or weakness and took thyroid hormone were excluded.
History of thyroid surgery, I131 treatment for Graves' disease or toxic multinodular goiter was also excluded. We implemented biochemical study, anti-thyroid peroxide enzyme antibody (Anti-TPO Ab), anti-thyroglobulin antibody (Anti-Tg Ab) at the study enrolling points. All patients underwent thyroid USG to evaluate echogenecity pattern and thyroid nodule.
Follow up studies was performed at the first 6-month and annually over a period of 5 yr. After 5 yr follow up, we classified them into 3 subgroups based on the end study of the thyroid function test (Normal thyroid function group, Persistent SCH group, and Overt hypothyroidism group).
Thyroid function test was measured using venous blood samples. Serum TSH (reference range: 0.17-4.05 µIU/mL, Beckman Coulter, Fullerton, CA, USA), free T4 (reference range: 0.89-1.79 ng/dL, Beckman Coulter) and T3 (reference range: 78-182 ng/dL, Beckman Coulter) levels were measured by radioimmunoassay (RIA).
Anti-TPO Ab and Anti-Tg Ab were measured by RIA (Beckman Coulter), with a reference value of up to 40 IU/L.
Thyroid USG was performed initially with a IU22 (Philips Medical System, Bothell, WA, USA) for evaluation echogenicity and thyroid nodule by designated one radiologist. The echogenicity was assessed by a standardized comparison of the echogenicity of the thyroid gland with the echogenicity of the sternohyoideus muscle. The radiologist followed the standard USG procedure to check thyroid illness.
We used PASW 18.00 (Version 12.0: SPSS Korea Date solution Inc., Seoul, Korea) as a statistical analysis method for this study. The variation was expressed as mean ± standard deviation. We used one-way ANOVA, chi-square test and logistic regression test as statistical analysis method and accepted that study was statistically significant if P value was less than 0.05.
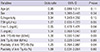
The clinical and biochemical parameters of all patients were summarized in Table 1. Study population was 169, their mean age was 51.5 ± 12.9 yr, and females were 124 (73.4%). The mean TSH, free T4 and T3 value was 7.16 ± 2.40 µIU/mL, 1.12 ± 0.18 ng/dL and 100.01 ± 19.39 ng/dL, respectively at the baseline study. As mentioned above, we repeated thyroid function test due to minimize assay variation or fluctuation. Free T4, T3 and TSH values were calculated the average levels of repeated thyroid function test.
The mean total cholesterol, HDL-C, LDL-C and triglyceride was 209.19 ± 73.96 mg/dL, 50.42 ± 15.61 mg/dL, 132.63 ± 106.25 mg/dL, 169.69 ± 263.97 mg/dL, respectively. Anti-TPO Ab was positive in 28.4% of patients; and Anti-Tg Ab was positive in 26.6% of patients.
Thyroid cancer was diagnosed in 8 patients at the beginning of the study. The majority of patients, 80 of 169 (47.3%), became having normal thyroid function after 5 yr of follow up. Sixty-two patients (36.7%) remained SCH continuously; and 19 patients (11.2%) progress to overt hypothyroidism. During the study, 5 patients (2.9%) developed painless thyroiditis while 3 (1.7%) progressed to hyperthyroidism.
SCH progressed to overt hypothyroidism in 1 patient at 6 month, 6 at 1th year, 5 at 2nd year, 4 at 3rd year, 2 at 4th year, and 1 at 5th year respectively. Overt hypothyroidism occurred within 3 yr mostly. Painless thyroiditis occurred in 3 patients at 1th year, 2 at 2nd year and hyperthyroidism occurred at 1th, 2nd, and 4th year respectively (Fig. 1).
There was no difference in age, sex and lipid levels between three subject groups based on thyroid function. The mean TSH level at the baseline study was significantly high in overt hypothyroidism (6.59 ± 2.32 µIU/mL vs 7.39 ± 2.33 µIU/mL vs 8.86 ± 2.40 µIU/mL [normal thyroid function group vs subclinical hypothyroidism vs overt hypothyroidism]) (Table 2). The mean free T4 level was also significantly low in overt hypothyroidism of 0.97 ± 0.11 ng/dL compared to normal thyroid function (1.17 ± 0.17 ng/dL) and SCH (1.11 ± 0.19 ng/dL), respectively. The cut off values for prediction of overt hypothyroidism were TSH >7.45 µIU/mL and free T4 < 1.09 ng/dL.
The positive ratio of Anti-TPO Ab was the highest in overt hypothyroidism group (46.7%) compared to SCH (34.6%) and normal thyroid function (16.7%), respectively. Also the positive rate of Anti-Tg Ab was the highest in overt hypothyroidism (46.7%) compared to SCH (34.9%) and normal thyroid function (18.3%), respectively. The Anti-TPO Ab titer was also significantly the highest in overt hypothyroidism of 680.33 ± 300.34 IU/mL compared to normal thyroid function (94.63 ± 100.22 IU/mL) and SCH (153.79 ± 218.43 IU/mL), respectively. There was no difference in anti-Tg Ab titer between the three groups.
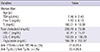
Multivariable logistic regression analysis showed TSH (odds ratio [OR], 1.27; 95% CI, 0.935-1.723; P = 0.050), free T4 (OR, 0.65; 95% CI, 0.478-1.421; P = 0.040), anti-TPO Ab titer (OR, 1.00; 95% CI 1.000-1.047; P = 0.03) and positivity of anti-TPO Ab (OR, 1.25; 95% CI 0.764-2.987; P = 0.04) as possible predictors of overt hypothyroidism (Table 3).
The frequencies of heterogeneous and homogenous echogenicity were 45.7% and 54.7% in SCH patients, respectively. The overt hypothyroidism group had higher heterogeneous echogenicity compared to normal thyroid function and SCH groups (76.5% vs 50.0% vs 35.0%, P = 0.048) (Table 2). The thyroid nodule was seen in 48.6% of SCH patients. Most of SCH patients had 1 to 2 nodules and only 3% of patients with thyroid nodule had more than 6 nodules.
In this study, of 169 patients, the number of women were 124 (73.4%) and that of men were 45 (26.6%). The majority of patients were women in many other SCH studies (18-20). The sex distribution of our study subject is comparable to previous studies for SCH. The prevalence of overt hypothyroidism was 4% to 15% in several studies (2,19). In this study the prevalence of overt hypothyroidism had similar result. SCH is related with coronary artery disease, cognitive function disorder, mood disorder, hyperlipidemia. We compared the presence of dyslipidemia related with thyroid dysfunction, however, there was no statistical relation between SCH and dyslipidemia.
Unlike previous studies that evaluated the natural history of SCH simply focused on the development of overt hypothyroidism. This is, to our knowledge, the first prospective study that evaluated not only the development of the overt hypothyroidism but also the occurrence of the other thyroid dysfunction in SCH. The majority of previous studies has done to observe the natural course of SCH for 1-3 yr. One prospective study of the spontaneous course of SCH over was done 9 yr. However, the study had a limitation that the subjects consisted of only women (16).
In our study for 5 yr, there was overt hypothyroidism of 19 patients (11.2%), painless thyroiditis of 5 (2.9%), hyperthyroidism of 3 patients (1.7%), SCH of 62 patients (36.7%), and normal thyroid function of 80 patients (47.3%). This study showed that the development of overt hypothyroidism or other thyroid dysfunction in SCH patients occurred within 3 yr. Therefore, we recommended that SCH patients were followed up thyroid function test at least 3 yr.
Pedro et al. (18) studied 117 patients of SCH for 3 yr and got the results of overt hypothyroidism of 27.3%, SCH of 20.5%, normal thyroid function of 52.1%. Huber et al. (15) reported 52% incidence rate of overt hypothyroidism during 9 yr study. One of Japan study for SCH, the incidence rate of overt hypothyroidism of 7% was similar to our study (19). Compared to our study, the higher incidence rate of overt hypothyroidism in western study was due to the difference of races and the number of study population composition. In our study 5 painless thyroiditis (2.9%) and 3 hyperthyroidism (1.7%) occurred. Painless thyroiditis occurred during 1-2 yr observation and hyperthyroidism occurred at 1-2 yr, and at the 4th year. The relation between overt hypothyroidism and painless thyroiditis were found by Glinoer et al. (20). There was increased SCH with high TSH value in pregnant women with thyroid autoimmune antibody as well as increase frequency of thyroiditis after delivery. All of 5 painless thyroiditis patients had thyroid autoantibody titers more than 10 times above the normal range in this study. Hyperthyroidism patients progress from SCH also had increased value of thyroid autoantibody. These patients with hyperthyroidism was diagnosed as Graves' disease and had high titer of thyroid binding inhibiting immunoglobulin, although, we did not evaluate the thyroid binding inhibiting immunoglobulin in all patients at base line study.
The clinical significance of mild elevation of TSH and the upper limit of normal for the serum TSH level have remained subjects of debate. In this study the cut off values for overt hypothyroidism showed TSH > 7.45 µIU/mL and free T4 < 1.09 ng/dL. Huber et al. (15) suggested that a TSH level higher than 12 µIU/mL predicts a higher rate of progression, and a level of less than 6 µIU/mL predicts a lower likelihood of progression. Our result showed that the cut off value for overt hypothyroidism was lower than previous studies (15, 19). In a Japanese study, TSH level > 8 µIU/mL was a predictive value for progression of overt hypothyroidism (19). The serum TSH level showed similar to our result. This could be suggested in part by the ethnic variation or also by study population and selection. A multivariate logistic regression analysis identified possible factor that were predictive of overt hypothyroidism: initial TSH, free T4, Anti-TPO Ab titer levels. The positive ratio of both thyroid autoantibodies (Anti-TPO Ab and Anti-Tg Ab) was the highest in overt hypothyroidism group compared to SCH and normal thyroid function in this study. Autoimmune thyroiditis is the most common cause of hypothyroidism and it's positivity of Anti-TPO Ab is over 90%, but our study showed lower rate of positivity of thyroid autoantibody than reported in previous studies. It can be explained in part by small sized population or by population selection. The Anti-TPO Ab titer was significantly high in overt hypothyroidism, compared to normal thyroid function and SCH. Cut off value of Anti-TPO Ab titer for prediction of overt hypothyroidism was 560 IU/mL. There were a few data about the cut off value of Anti-TPO Ab titer for prediction of overt hypothyroidism. In one study reported that antibody titers more than 10 times above the normal range had a significantly higher incidence of developing overt hypothyroidism than patients with negative.
In agreement with previous studies, these results demonstrate that the presence of thyroid autoantibodies is predictive parameter of overt hypothyroidism. In Korean study, they showed that Anti-Tg Ab also appear to be better predictive thyroid autoantibody like Anti-TPO Ab for development of overt hypothyroidism (21). Huber et al. (15) suggested that Anti-Tg Ab did not have a predictive value for the progression to overt hypothyroidism, which is in contradiction with our findings.
There were a few data about the evaluation of thyroid nodule in SCH. 48.6% of enrolled patients had thyroid nodules in our study. Generally the prevalence of ultrasound detectable thyroid nodule is between 19% and 67%. Most of all patients with thyroid nodules has less than 2 nodules, and only 3% of patients with thyroid nodule had more than six. There were 8 patients who was diagnosed thyroid papillary cancer. Cooper et al. (12) reported that the overall risk of malignancy in a thyroid nodule is 5% to 10%. In this study, the prevalence of thyroid cancer was 9.3% in SCH with thyroid nodule. These results showed that SCH had similar prevalence of thyroid nodule and cancer as in general population. Vejbjerg et al. (22) reported that heterogeneous echogenicity in thyroid USG and higher serum TSH level even in subjects without overt thyroid disease are possible marker of thyroid failure. Similarly, the overt hypothyroidism group had higher heterogeneous echogenicity compared to normal thyroid function and SCH groups in this study.
In conclusion, this study suggested that subclinical hypothyroidism has various courses. Initial TSH, free T4, presence of thyroid autoantibody, high level of thyroid autoantibody titer and thyroid USG findings may be prediction factors for the progression of overt hypothyroidism. Additionally, our findings suggested that there may be a benefit to initiate therapy in SCH patients who had these factors at initial evaluation.
Figures and Tables
Fig. 1
Incidence of thyroid dysfunction. TSH, Thyroid stimulating hormone; SCH, Subclinical hypothyroidism.

Table 2
Prognostic factors for development of overt hypothyroidism
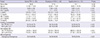
Reference range of Thyroid function test. TSH, 0.17-4.05 µIU/mL; Free T4, 0.89-1.79 ng/dL; T3, 78-182 ng/dL; Anti-TPO Ab, anti-thyroid peroxidase autoantibody; Anti-Tg Ab, thyroglobulin antibody; TSH, Thyroid stimulating hormone; SCH, Subclinical hypothyroidism; TC, Total cholesterol; TG, Triglyceride; USG, Ultrasonography.
References
1. Cooper DS. Clinical practice: subclinical hypothyroidism. N Engl J Med. 2001; 345:260–265.
2. Kang HC. Selective therapy of subclinical hypothyroidism. J Korean Thyroid Assoc. 2009; 2:93–97.
3. Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med. 2000; 160:526–534.
4. Hak AE, Pols HA, Visser TJ, Drexhage HA, Hofman A, Witteman JC. Subclinical hypothyroidism is an independent risk factor for atherosclerosis and myocardial infarction in elderly women: the Rotterdam Study. Ann Intern Med. 2000; 132:270–278.
5. Rodondi N, Newman AB, Vittinghoff E, de Rekeneire N, Satterfield S, Harris TB, Bauer DC. Subclinical hypothyroidism and the risk of heart failure, other cardiovascular events, and death. Arch Intern Med. 2005; 165:2460–2466.
6. Biondi B, Cooper DS. The clinical significance of subclinical thyroid dysfunction. Endocr Rev. 2008; 29:76–131.
7. Samuels MH, Schuff KG, Carlson NE, Carello P, Janowsky JS. Health status, mood, and cognition in experimentally induced subclinical hypothyroidism. J Clin Endocrinol Metab. 2007; 92:2545–2551.
8. Roberts LM, Pattison H, Roalfe A, Franklyn J, Wilson S, Hobbs FD, Parle JV. Is subclinical thyroid dysfunction in the elderly associated with depression or cognitive dysfunction? Ann Intern Med. 2006; 145:573–581.
9. Surks MI, Ortiz E, Daniels GH, Sawin CT, Col NF, Cobin RH, Franklyn JA, Hershman JM, Burman KD, Denke MA, et al. Subclinical thyroid disease: scientific review and guidelines for diagnosis and management. JAMA. 2004; 291:228–238.
10. McDermott MT, Ridgway EC. Subclinical hypothyroidism is mild thyroid failure and should be treated. J Clin Endocrinol Metab. 2001; 86:4585–4590.
11. Danese MD, Ladenson PW, Meinert CL, Powe NR. Clinical review 115: effect of thyroxine therapy on serum lipoproteins in patients with mild thyroid failure: a quantitative review of the literature. J Clin Endocrinol Metab. 2000; 85:2993–3001.
12. Cooper DS, Halpern R, Wood LC, Levin AA, Ridgway EC. L-Thyroxine therapy in subclinical hypothyroidism: a double-blind, placebo-controlled trial. Ann Intern Med. 1984; 101:18–24.
13. Nyström E, Caidahl K, Fager G, Wikkelsö C, Lundberg PA, Lindstedt G. A double-blind cross-over 12-month study of L-thyroxine treatment of women with 'subclinical' hypothyroidism. Clin Endocrinol (Oxf). 1988; 29:63–75.
14. Razvi S, Ingoe L, Keeka G, Oates C, McMillan C, Weaver JU. The beneficial effect of L-thyroxine on cardiovascular risk factors, endothelial function, and quality of life in subclinical hypothyroidism: randomized, crossover trial. J Clin Endocrinol Metab. 2007; 92:1715–1723.
15. Huber G, Staub JJ, Meier C, Mitrache C, Guglielmetti M, Huber P, Braverman LE. Prospective study of the spontaneous course of subclinical hypothyroidism: prognostic value of thyrotropin, thyroid reserve, and thyroid antibodies. J Clin Endocrinol Metab. 2002; 87:3221–3226.
16. Kabadi UM. 'Subclinical hypothyroidism': natural course of the syndrome during a prolonged follow-up study. Arch Intern Med. 1993; 153:957–961.
17. Karlin NJ, Weintraub N, Chopra IJ. Current controversies in endocrinology: screening of asymptomatic elderly for subclinical hypothyroidism. J Am Med Dir Assoc. 2004; 5:333–336.
18. Rosário PW, Bessa B, Valadão MM, Purisch S. Natural history of mild subclinical hypothyroidism: prognostic value of ultrasound. Thyroid. 2009; 19:9–12.
19. Imaizumi M, Sera N, Ueki I, Horie I, Ando T, Usa T, Ichimaru S, Nakashima E, Hida A, Soda M, et al. Risk for progression to overt hypothyroidism in an elderly Japanese population with subclinical hypothyroidism. Thyroid. 2011; 21:1177–1182.
20. Glinoer D, Riahi M, Grün JP, Kinthaert J. Risk of subclinical hypothyroidism in pregnant women with asymptomatic autoimmune thyroid disorders. J Clin Endocrinol Metab. 1994; 79:197–204.
21. Shin DY, Kim EK, Lee EJ. Role of ultrasonography in outcome prediction in subclinical hypothyroid patients treated with levothyroxine. Endocr J. 2010; 57:15–22.
22. Vejbjerg P, Knudsen N, Perrild H, Laurberg P, Pedersen IB, Rasmussen LB, Ovesen L, Jørgensen T. The association between hypoechogenicity or irregular echo pattern at thyroid ultrasonography and thyroid function in the general population. Eur J Endocrinol. 2006; 155:547–552.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download