Abstract
Streptococcus pneumoniae can asymptomatically colonize the nasopharynx and cause a diverse range of illnesses. This clinical spectrum from colonization to invasive pneumococcal disease (IPD) appears to depend on the pneumococcal capsular serotype rather than the genetic background. According to a literature review, serotypes 1, 4, 5, 7F, 8, 12F, 14, 18C, and 19A are more likely to cause IPD. Although serotypes 1 and 19A are the predominant causes of invasive pneumococcal pneumonia, serotype 14 remains one of the most common etiologic agents of non-bacteremic pneumonia in adults, even after 7-valent pneumococcal conjugate vaccine (PCV7) introduction. Serotypes 1, 3, and 19A pneumococci are likely to cause empyema and hemolytic uremic syndrome. Serotype 1 pneumococcal meningitis is prevalent in the African meningitis belt, with a high fatality rate. In contrast to the capsule type, genotype is more closely associated with antibiotic resistance. CC320/271 strains expressing serotype 19A are multidrug-resistant (MDR) and prevalent worldwide in the era of PCV7. Several clones of MDR serotype 6C pneumococci emerged, and a MDR 6D clone (ST282) has been identified in Korea. Since the pneumococcal epidemiology of capsule types varies geographically and temporally, a nationwide serosurveillance system is vital to establishing appropriate vaccination strategies for each country.
Streptococcus pneumoniae (pneumococcus) is an important pathogen with high associated morbidity and mortality worldwide. It causes otitis media, sinusitis, pneumonia, and invasive pneumococcal diseases (IPD). Diagnosis of IPD requires pneumococcus isolation from a normally sterile site, such as blood, cerebrospinal fluid (CSF), and pleural or ascitic fluid. The incidence of IPD in developed countries is estimated to be 8-34 cases per 100,000 inhabitants with geographical variance (1), and the mortality rate ranged from 10% to 30% (2-4). Despite the availability of vaccines and antibiotics, a 2008 report from the World Health Organization (WHO) indicated that S. pneumoniae is responsible for approximately 1.6 million deaths annually, particularly among young children and the elderly (5).
Pneumococci are spherical, Gram-positive bacteria, which have many virulence factors, including capsular polysaccharides, pneumolysin, pneumococcal surface protein A (PspA), pneumococcal surface protein C (PspC), and pneumococcal surface adhesin A (PsaA). Among these, capsular polysaccharides are considered to be the most important virulence factor as they surround pneumococci and shield them from phagocytes. Currently, 94 capsular serotypes, including the recently reported serotypes 6C, 6D, 11E, and 20A/20B, have been identified (6-9). Each serotype is distinguished by serological response (the ability to react with specific antibodies against the capsular antigen), the chemical structure of capsular polysaccharides, and other related genetic mutations. Based on these pathogenic mechanisms, a serotype-specific pneumococcal polysaccharide vaccine (PPV) was developed, which contained pooled capsular polysaccharides of various serotypes. In 1983, a 23-valent PPV (PPV23) was approved, expanding serotype coverage to more than 85% of the organisms causing IPD at the time (10). However, the poor immunogenicity of T-cell-independent PPV23 in infants led to development of the pneumococcal conjugate vaccine (PCV). Covalent coupling of the polysaccharide to a protein carrier effectively converts the T-cell-independent Type 2 polysaccharide into a T-cell-dependent antigen; carrier proteins include a non-toxic mutant of diphtheria toxin (CRM197), as well as other proteins such as protein D of non-typeable Haemophilus influenzae (11). The first 7-valent PCV (PCV7) was licensed in the United States (US) in 2000 and introduced to Korea in 2003. This PCV included capsular polysaccharides of serotypes 4, 6B, 9V, 14, 18C, 19F, and 23F, representing approximately 80%-90% of IPD in children (12). With serotype shifts resulting from vaccine pressure, however, the protective coverage of PCV7 was reduced, and PCV7 did not include serotypes 1, 3, and 5, which are common in Europe, Asia, and Africa (13, 14). Therefore, a 13-valent PCV (PCV13), which included serotypes 1, 3, 5, 6A, 7F, and 19A, was introduced for children in 2010 and later licensed for adults in 2012.
Thus, pneumococcal capsules play the most important role in pathogenesis, and they have a great implication in vaccine development. Of note, serotype distributions of pneumococcal capsules vary geographically and temporally in terms of nasopharyngeal carriage, pathogenicity and clinical presentation (13, 15). This article will review the serotype-specific characteristics of pneumococcus with regard to the epidemiological and clinical aspects, including carriage rate, invasive disease potential, clinical presentation, and antibiotic resistance.
Pneumococcus exists only in the nasopharynx of humans, and it has no natural reservoir in animals. Humans are the exclusive targets of pneumococcal diseases, with transmission only coming from other human carriers. Thus, carriage is essential for the propagation of pneumococcal diseases, and its epidemiology is important. Pneumococcal colonization may be influenced by multiple factors. Although these factors are not entirely clear, there is no doubt that the local host immune response plays an important regulatory role in the trafficking of pathogens in the nasopharynx. Poorly immunogenic serotypes tend to colonize for longer periods, and the low carriage rates in adults suggest the existence of immunological protection after previous exposure (16).
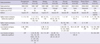
Pneumococcal carriage occurs early in life, usually with a prevalence of about 30%-60% in infants and 1%-10% in adults (17, 18). In some cases, more than 95% of children can be colonized with up to six different serotypes by the age of two (19). The prevalence of co-colonization by multiple serotypes was estimated to range from 1.3% to 48.8% (20, 21). Geographical factors, study population, and different detection techniques may be responsible for this variation (21). The epidemiology and clinical significance of co-colonization needs better clarification. As children grow older, the prevalence of pneumococcal carriage decreases, and the distribution of colonizing serotypes changes to those found in adults. Before the age of nine, the carriage rate is maintained above 30%-40%, but it declines progressively afterward (Table 1) (22-24). However, the carriage rate is quite variable according to the local epidemiology, trending toward higher carriage rates in impoverished communities with low vaccination rates. Studies by Mackenzie et al. and Hill et al. showed remarkably high carriage rates (≥ 30%), even in young adults (Table 1) (25, 26). In Korea, the pneumococcal carriage rate was estimated to be 34.3% among children aged 5 yr or younger before the introduction of PCV7 (27), and it was 16.5% among those aged 18 yr or less in the era of PCV7 (28). Considering the difference in study populations, there is a limitation to comparing the results of these two studies (Table 1), and data on Korean adults is not available.
Common colonizing serotypes differ between young children (< 5 yr) and adolescents/adults. Before the introduction of PCV7, serotypes 19F, 6A, 6B, and 23F were prevalent in young children aged less than 5 yr, while serotypes 3 and 23F were relatively common in adolescents and adults (22, 23, 29). After the introduction of PCV7, these were replaced by non-vaccine serotypes, including 19A, 6C, 11A, 15A, and 15B/C (28, 30).
The duration of colonization can range from days to months and depends on the serotype (31). Serotype 1 is rarely found to colonize the nasopharynx, and serotypes 4, 5, and 7F also colonize to lesser degrees (32, 33). These serotypes are able to initiate colonization of the nasopharynx, but colonization may be much shorter in duration compared to other serotypes. Sleeman et al. (33) estimated the duration of pneumococcal carriage among common colonizing serotypes. The duration ranged from 5.9 weeks for serotype 15C to 19.9 weeks for serotype 6B.
Causative mechanisms of carriage rate remain unclear. Several mechanisms have been postulated, most of which hinge on interactions between the bacteria and host immune defenses. Serotype-specific polysaccharide capsules protect against immune-mediated clearance in several ways, including blocking the deposition and function of opsonins (34), trapping by neutrophil extracellular traps (NETs), and clearance by mucus (35, 36). Both the prevalence of carriage and virulence appear to be directly related to the degree of encapsulation. In a murine study, Weinberger et al. (37) demonstrated higher carriage rates among serotypes with larger capsules. Furthermore, those serotype capsules containing more carbon molecules per polysaccharide repeat unit tend to be smaller and more prone to nonopsonic killing. Authors from this study suggest that low-carbon polysaccharide repeats would require less energy to manufacture and afford a lower "metabolic cost," allowing a larger polysaccharide bulk and therefore improved fitness for carriage.
Pneumococcal capsule types are known to be associated with many important pathogenic processes, including complement deposition, inflammation, and binding to the C-type lectin of host phagocytes (38, 39). In an animal study by Briles et al. (40), a very strong association was demonstrated between capsular serotype and virulence (the ability of an isolate to kill mice and the length of time between inoculation and death). In mice, serotypes 3, 4, 6A, and 6B were virulent; serotype 1 isolates were marginally virulent; and serotypes 14, 19, and 23 were avirulent. Clinically, global surveillance demonstrates that a limited number of capsular serotypes cause more than 70%-80% of IPD (41), and the invasive property of pneumococci seems to be determined by capsular serotype rather than genotype, as determined by multilocus sequence typing (MLST) (42). Genetic elements may contribute to the heterogeneity of invasive disease potential among the same serotype (43).
Some serotypes commonly colonize the nasopharynx, thereby having a greater temporal opportunity for invasion. In comparison, some serotypes are more likely to cause invasive disease with each episode of colonization. Several parameters have been used to estimate the serotype-specific invasive disease potential: invasive odds ratio (OR), invasive capacity (IC), and attack rate. Among them, invasive OR has been used most frequently in the literature (29, 42-46). Invasive OR is calculated by reference to all the other serotypes as follows: OR = (ad)/(bc), where a is the number of invasive A serotypes, b is the number of carriage A serotypes, c is the number of invasive non-A serotypes, and d is the number of carriage non-A serotypes. IC is calculated as the ratio of IPD incidence to carriage prevalence, while the attack rate is defined as the ratio of IPD incidence to the incidence of acquisition for each serotype (33, 47). Both are expressed as the number of IPD cases per 100,000 carriages or acquisitions. Sleeman et al. (33) classified a high attack rate as 20 or more IPD cases per 100,000 acquisitions, and a low attack rate as less than 10 IPD cases per 100,000 acquisitions. Table 2 summarizes studies about the relationship between pneumococcal serotype and invasive disease potential. Some serotypes (1, 4, 5, 7F, 8, 12F, 14, 18C, and 19A) were considered highly invasive, while others (6A, 6B, 11A, 15B/C, and 23F) were generally less invasive in most studies (29, 33, 42, 43, 45-47). Serotype prevalence was variable between studies, which may be due to geographic and epidemiologic differences. Serotype 6B was highly invasive according to the report by Hanage et al. (44), but was not as invasive in other studies (29, 33, 42, 43, 45, 46). Also, reports of the invasive disease potential of serogroup 9 (9A, 9V, 9N, and 9L) showed some variation (29, 33, 42-46). Except for the study by Yildirim et al. (47), all the studies of Table 2 were conducted before the widespread use of PCV7. Recently, Scott et al. (24) assessed changes in the serotype-specific invasive disease potential during the PCV7 era and found no remarkable change in the invasive potential among serotypes. Although the serotype-specific IPD incidence might be proportional to the carriage prevalence, it is important to continue monitoring the change in the serotype-specific invasive disease potential.
Different pneumococcal serotypes are known to cause different clinical presentations of pneumococcal diseases. Globally, serotypes 3, 6A, 6B, 9V, 14, 19A, 19F, and 23F were reported to cause acute otitis media (AOM) in young children, according to a recent review (48). Particularly, serotype 19A pneumococcal AOM increased predominantly after the introduction of PCV7 (49, 50). Serotypes 3, 11A, and non-typeable (NT) pneumococci are associated with acute conjunctivitis (46). Regarding IPD, serotypes 1, 5, and 7F usually affect healthy young adults with a low mortality rate, while serotypes with low or intermediate invasive potential are more likely to affect the elderly with underlying comorbidities (32, 51, 52). Yildirim et al. (53) compared the incidence and serotype distribution of IPD among children less than 18 yr of age between the early (2001-2006) and late (2007-2010) periods of the PCV7 era in the US. The overall IPD incidence rate was 7.5 cases per 100,000 inhabitants, without a statistical difference between these two periods, although the proportion of bacteremic pneumonia among all IPD cases was almost three-fold greater in 2009-2010 compared to the early period. IPD due to serotypes 19A and 7F increased during the late period of the PCV7 era, representing 41% and 20% of all IPD cases in the same period, respectively. Changes in the distribution of serotypes may affect the clinical presentation of IPD.
A recent meta-analysis evaluated serotype-specific case fatality rates (CFRs). This study revealed that serotypes 1, 7F, and 8 were associated with lower mortality, whereas serotypes 3, 6A, 6B, 9N, and 19F were associated with increased mortality (54). In a nationwide, population-based cohort study of IPD in Denmark over the period of 1977-2007, serotypes 3, 10A, 11A, 15B, 16F, 17F, 19F, 31, and 35F were associated with highly increased mortality as compared with serotype 1 (adjusted odds ratio ≥ 3, P < 0.001) (55). Van Hoek et al. (56) estimated the CFRs of IPD by serotype and age group (< 5, 5-64, and ≥ 65 yr) in England from April 2002 to March 2011. Among patients younger than 5 yr, CFR was low (overall 3%), with the highest rate occurring with serotype 6A (7%), followed by 19F (5%), 9V (5%), and 3 (5%). In the age group of 5-64 yr, the overall CFR was 10%; serotypes 31 (33%), 11A (30%), and 19F (21%) had the highest CFRs, while serotypes 1 (3%), 7F (4%), and 8 (6%) had the lowest rates. Patients aged 65 yr and older had the highest CFR (overall 30%); serotypes 19F (41%), 31 (40%), and 3 (39%) were associated with the highest CFRs, whereas serotypes 1 (17%), 7F (20%), and 12F (21%) were associated with lower CFRs.
S. pneumoniae is the most common cause of community-acquired pneumonia (CAP) in children and adults (57). While the majority of pneumococcal pneumonia cases are non-bacteremic (60%-80%), bacteremic pneumonia is more severe (58-60). Bacteremic and non-bacteremic pneumonia are considered to be different clinical entities. In mice, several thousand colony-forming units (CFUs) of S. pneumoniae of serotypes 2 or 3 in the lungs result in bacteremia and death, whereas S. pneumoniae of serogroup 19 is unable to induce bacteremia after lung infection and results in a nonprogressive course unless tens of millions of CFUs are inoculated (61).
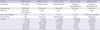
According to a recent meta-analysis, pneumococcal serotype 14 was the most prevalent etiologic agent of pneumococcal CAP, followed by serotypes 1 and 5, in Latin America and the Caribbean (Table 3) (62). Since PCV7 was not adopted into the national immunization program in the Latin America and Caribbean regions during the study periods, it was not possible to determine the serotype shift between the pre- and post-vaccination eras. In the studies which included the post-PCV7 periods, serotype 1 was predominant, followed by serotypes 19A and 3. The prevalence of serotype 14 was decreased to around 5% (60, 63, 64).
Among adults, Burgos et al. (65) reported that serotype 14 was still one of the most common causes of pneumococcal pneumonia in Spain, even after PCV7 introduction. Likewise, in a UK study, Bewick et al. (66) also reported that the most common serotypes were 14, 1, 8, 3, and 19A in adult pneumococcal CAP, while serotypes 19A, 3, and 6A/C were the most prevalent in IPD. They emphasized that cohort studies of IPD alone may underestimate the true prevalence of serotype 14. In comparison, Cilloniz et al. (60) reported serotypes 1 and 19A as the predominant agents of invasive pneumococcal pneumonia in Spanish adults. Although the vaccination rate and secular trend affect the outcomes, there may be some differences in the serotype distributions between invasive and non-invasive pneumococcal pneumonia, particularly among adults. As for the serotype distribution in pneumonia, no data was available from Asian countries.
Necrotizing pneumonia is a complicated pneumococcal infection, which is associated with a significant increase in morbidity and mortality. In the pre-antibiotic era, studies of autopsy cases described a necrotizing change in about 5% (0.7%-27%) of cases, and a recent large-series study (using computed tomography) reported its occurrence in 6.6% of adult pneumococcal pneumonia cases (67). Serotype 3 strains have been recognized as the most common etiologic agents (63, 67, 68).
Serotypes 1, 3, 7F, 14, and 19A are known to be associated with empyema complications after pneumococcal infection (69-72). Empyema was considered rare in children, but it has been increasing worldwide over the last decade (69, 73-75). Lee et al. (76) evaluated 62 Korean children with empyema, where serotype 19A was most frequently identified (46.2% of pneumococcal empyema). In a recent US study of 49 cases of pediatric empyema, serotypes 3 (26.5%) and 19A (22.4%) were the most common etiologies, followed by serotypes 7F (14.3%) and 1 (12.2%) (77). However, many studies showed that most pediatric empyema cases were more directly linked to non-PCV7 serotype 1, due to selective PCV7 pressure (64, 78, 79). According to the MLST of serotype 1 isolates, sequence types (ST) 227, ST228, and ST304 were genotypes that previously existed, while ST306 was newly detected after PCV7 introduction (78, 80). Serotype 1 pneumococcal empyema was also common in adults aged between 18 and 50 yr; according to the report by Burgos et al. (81), more than 40% of pneumococcal empyema were caused by serotype 1. It is also possible that serotype 1 is associated with empyema due to the zwitterionic polysaccharides found in its capsule, which have been related to abscess formation in animal models (32).
S. pneumoniae is estimated to cause more than 60,000 meningitis-associated deaths and long-term disabilities in children five years of age or younger worldwide annually (82). The incidence of pneumococcal meningitis is highest in children under one year of age, but data on the serotype distribution remain insufficient in Asian countries. According to surveillance in Ugandan children aged less than five years, the most common serotype was 6A/6B (40%), followed by 22A, 23F, 14, and 19A (83). Previously, serotypes 1, 3, and 5 were rarely reported in cases of meningitis (52). However, recent studies in the African meningitis belt revealed that 60%-80% of pneumococcal meningitis was caused by serotype 1, with higher incidence and case fatality ratios compared to meningococcal meningitis (84). Compared to the US and Europe, where a bimodal age distribution is observed, the pneumococcal meningitis epidemiology of the African meningitis belt is quite different. Serotype 1 is predominant, and older children and working-age adults are more likely to be infected, with a high case fatality rate. Such differences might be due to the properties of the African lineage of serotype 1, rather than the general characteristics of serotype 1 (85). MLST has identified three clonal lineages of serotype 1, and these were geographically segregated. As for travelers to African meningitis belt areas, PCV13 vaccination is recommended in addition to the meningococcal vaccination.
Serotype prevalence in the US has undergone a significant shift since routine immunization with PCV7 commenced. Comparing data from 1998-1999 to 2004-2005, there has been a significant reduction in pneumococcal meningitis among the PCV7 serotypes, from 59 to 23 percent of cases (P < 0.001) (86). Non-PCV7 serotype disease has expectantly increased, from 28 to 65 percent (P < 0.001), with a preponderance of the increase being attributed to serotypes 19A and 22F (86). Despite the observed serotype shift, the overall incidence of pneumococcal meningitis in the US has decreased by 30 percent to 0.79 cases/100,000 (86).
Primary pneumococcal peritonitis in children has been recognized for more than a century (87, 88). Its peak incidence occurs in children between the ages of 5 and 7 yr, and it is more common in girls than in boys (89). Pneumococcal peritonitis is usually associated with nephrotic syndrome in children, while it is related to cirrhosis in adults (90-92). In healthy adults, pneumococcal peritonitis is unusual, but it typically occurs in young women as a result of serotype 1 pneumococci (93, 94), causing pelvic abscesses or other reproductive tract infections. Pneumococci are still common etiologic agents of spontaneous bacterial peritonitis in cirrhotic patients; however, there is no published data on the serotype distribution.
Hemolytic uremic syndrome (HUS) is characterized by the triad of microangiopathic hemolytic anemia, thrombocytopenia, and acute renal failure. Typical HUS usually follows an episode of gastroenteritis with enterotoxigenic Escherichia coli. Although S. pneumoniae-associated HUS (SP-HUS) occurs after bacterial infection, similar to typical HUS, the clinical outcomes are worse than typical HUS, with a higher dialysis requirement (82% vs 42%) and mortality rate (< 11% vs < 5%) (95). SP-HUS is known to occur exclusively in children after IPD, with a low incidence rate (0.4%-0.6%) (96, 97). However, SP-HUS is often mistaken for disseminated intravascular coagulation (DIC), and, as result, not all SP-HUS cases may have been reported. Nevertheless, case reports are increasing after the introduction of PCV7 (98-100).
The hypothesized pathogenic mechanism of SP-HUS suggests that neuraminidase-producing pneumococcus exposes the normally hidden Thomsen-Freidenreich antigens (T-Ag) of erythrocytes, platelets, and renal endothelial cells. Free T-Ag reacts with anti-T immunoglobulin, resulting in hemolysis, polyagglutination, endothelial damage, and thrombotic microangiopathy (101, 102). Positive T-Ag activation and a direct Coombs' test are predictive of SP-HUS after IPD, and these aid in differentiating typical and atypical HUS (95, 99).
Considering the pathogenic mechanism, SP-HUS development may not be dependent on the capsule serotype. Limited data suggest a weak association of SP-HUS with specific serotypes (1, 3, 6A, 7F, 12F, 14, 19A, 22F, and 23F), as well as a high concurrence with empyema (103, 104). In mouse models, pneumococcal neuraminidase expression was higher in the lungs than in blood and was greater in bacteria growing in biofilms than in planktonic forms, potentially explaining the strong association between SP-HUS and empyema (105). Pneumococcal serotypes with a high predilection to cause complicated pneumonia accompanying empyema may be major etiologies of SP-HUS. Before the introduction of PCV7, serotype 14 was the most common, but a serotype shift was observed, with increasing cases of serotypes 1, 3, 7F, and 19A, with serotype 3 being predominant (100, 106-108).
The ability of S. pneumoniae to undergo horizontal gene transfer leads to its genetic diversity and helps the organism adapt to environmental changes, including antibiotic pressure. Theoretically, the genotype should primarily correlate with antibiotic resistance. However, strategies for pneumococcal vaccines are actually based on serotype distribution, and therefore serotype-related antibiotic resistance has also been studied with interest. Herein, the relations between the pneumococcal serotype and genotype were addressed with regard to antibiotic resistance. Hsieh et al. (109) showed that different serotypes of S. pneumoniae possess different levels of genetic competence, which is the ability of a cell to take up extracellular DNA from its environment. Isolates belonging to serotypes 3 and 18C that were 100% sensitive to penicillin were significantly less competent than isolates belonging to serotypes 6B, 14, 19F, 9V, and 23F, which were frequently resistant to penicillin. Intriguingly, the capsule (cps) locus of S. pneumoniae is flanked by the pbp2x and pbp1a genes, which code for penicillin-binding proteins (PBPs) (110). PBPs are enzymes involved in cell wall synthesis and are targets for β-lactam antibiotics. Under the natural selection imposed by host immunity and antibiotics, the recombination events would involve PBP genes, as well as the cps operon, and would change both the serotype and the resistance profile of the strain.
The prevalence of antibiotic-resistant S. pneumoniae has increased worldwide and might be related to the spread of pediatric pneumococcal serotypes (6A, 6B, 9V, 14, 15A, 19F, 19A, and 23F). After the introduction of PCV7, the prevalence of PCV7 serotypes and serotype 6A were reduced and subsequently replaced by non-PCV7 serotypes, including serotype 19A. Although Spain23F-ST81 and Spain6B-ST90 were well-established multidrug-resistant clones in the 1980s and 1990s, their prevalence decreased after the introduction of PCV7 (111).
Serotype 19A is the most prominent serotype worldwide, both clinically important and multidrug-resistant (non-susceptible to ≥ 3 antibiotic classes) in the era of PCV7. More than 30% of serotype 19A isolates were multidrug resistant (112, 113). With dual macrolide resistance mechanisms (ermB and mefA), they showed resistance to erythromycin (high level, MIC ≥ 32 µg/mL), tetracycline, clindamycin, cefuroxime, and trimethoprim/sulfamethoxazole (114, 115). Erythromycin resistance was highly correlated with azithromycin and clarithromycin resistance (113). Although the resistance rate for penicillin is quite low (minimum inhibitory concentration [MIC] ≥ 8 µg/mL, < 5%) based on the revised 2008 Clinical and Laboratory Standards Institute (CLSI) breakpoint, multidrug-resistant serotype 19A isolates showed relatively high penicillin MICs (MIC50, 1.5 µg/mL) (116).
In addition, some strains of recently identified serotypes 6C and 6D S. pneumoniae showed multidrug resistance (117-119). While serotype 6C was first described in 2006, it has been identified from isolates dating back to 1962 (117). Serotype 6D S. pneumoniae isolates were reported in several regions, including Korea, Japan, China, Hong Kong, Fiji, Australia, Finland, Poland, Peru, and Canada (7, 120-128).
Of note, serotype 19A pneumococci with multidrug resistance had already been reported in some regions before the introduction or widespread use of PCV7. According to a surveillance study in Korea, serotype 19A had already increased among children aged less than 5 yr before the introduction of PCV7 (8% increase between 1991 and 1997 and an 18% increase between 1997 and 2003) (116). The pre-existing ST320 genotype was responsible for the expansion of multidrug-resistant serotype 19A, which belonged to the clonal complex (CC) 320/271. ST320 serotype 19A isolates showed a higher rate of antibiotic resistance compared to non-ST320 isolates: penicillin (MIC ≥ 2 µg/mL, 47.8% vs 34.1%), cefuroxime (82.6% vs 63.7%), erythromycin (71.7% vs 65.9%), clindamycin (73.9% vs 59.3%), and trimethoprim/sulfamethoxazole (82.6% vs 64.8%) (113). Antibiotic abuse/overuse might facilitate the spread of multidrug-resistant serotype 19A strains. CC320/271 serotype 19A strains were not limited just to Korea, having become prevalent in several Asian countries. The Asian Network for Surveillance of Resistant Pathogens (ANSORP) study surveyed ten Asian countries (Korea, Japan, Hong Kong, Taiwan, Malaysia, Philippines, Thailand, Saudi Arabia, India, and Vietnam) during the period of 2008-2009 and found that 5.6% of clinical pneumonia isolates were serotype 19A pneumococci, and 51.6% of them were ST320 strains (129).
In the US and Canada, CC320/271-expressing serotype 19A emerged and expanded after PCV7 introduction, which may have arisen from a capsular switch with Taiwan19F-ST236 (130). The Active Bacterial Core Surveillance system of the US Centers for Disease Control and Prevention (CDC) reported that the proportion of IPD by penicillin non-susceptible S. pneumoniae (PNSP) expressing serotype 19A increased significantly during 2004-2008, reaching 43.7% (MIC ≥ 2 µg/mL) by 2008 (131). The proportion of CC320/271 serotype 19A isolates increased in parallel, from 20.9% to 32.9% of IPD isolates during 2005-2007. In 2007, 82.1% (202 among 246) of serotype 19A isolates belonged to CC320/271.
In Europe, ST230 and ST276, the members of CC230, have been identified as a major serotype 19A lineage responsible for causing IPD (111, 132). Compared to Korea and North America, the STs were diverse, and ST320 was infrequent. In a Portuguese surveillance study from 2001 to 2006, ST320 was absent, and ST230 was the most common genotype (133). A French study characterizing invasive isolates also identified ST276 as a representative clone (132). In Italy, the increased prevalence of serotype 19A was due to expansion of CC199 (ST416 and ST199) after PCV7 introduction (134). According to the Spanish Pneumococcal Reference Laboratory (SPRL) study, however, the prevalences of ST81 and ST202 were decreasing, while those of ST878 and ST320 showed increasing trends (135). During the study period, serotype 19A increased from 5.7% in 2000 to 16.8% in 2008 (135). Therefore, continuous monitoring is required to detect the spread of multidrug-resistant clones, and strict control of antibiotic use might be an important strategy to minimize further spread.
In the late PCV7 period, the prevalence of serotype 6C pneumococci increased in the US, Spain, and Portugal (117, 119, 136). The rate of multidrug resistance increased, and the strains were genetically diverse. In the US, the two main clonal clusters were ST473 and ST1292 (117). Both STs were non-susceptible to erythromycin and trimethoprim/sulfamethoxazole, and ST1292 showed decreased susceptibility to penicillin and ceftriaxone. In Spain, the increase of serotype 6C prevalence was associated with the emergence of ST386/ST4310/ST4825, which were non-susceptible to penicillin, erythromycin, tetracycline and clindamycin (119). Considering that serotype 6C was more common in older children and adults, fluoroquinolone resistance should be monitored, although its frequency has remained low (119, 137).
While serotype 6D S. pneumoniae has been isolated in several regions, it is characteristically prevalent in Korea, comprising more than 10% of serogroup 6 isolates (138, 139). Among the three clones of serotype 6D S. pneumoniae found in Korea (ST189, ST282, and ST3171), ST189 and ST282 strains are related to CC81 (138). Ko et al. (118) reported that all ST282 isolates were non-susceptible to penicillin and cefuroxime, and more than 50% of them were resistant to trimethoprim/sulfamethoxazole. In comparison, ST3171 isolates showed resistance to only macrolides and clindamycin. Fortunately, ST282 strains have only been reported in Korea, and STs of serotype 6D pneumococci were very diverse worldwide: Japan (ST2924), China (ST982 and ST4190), Hong Kong (ST5085 and ST5086), Fiji (ST639, ST473, and ST4240), Australia (ST4241), Finland (ST5163), Poland (ST948, ST2181, ST1612, and ST4734), and Peru (ST6148) (118). While currently insignificant, the trend of antibiotic resistance in serotype 6D S. pneumoniae should be monitored with vigilance.
Pneumococcal serotype appears to be much more important in determining colonization, disease development, and clinical phenotype compared to the genetic background. Among the current 94 serotypes, a limited number of serotypes cause more than 70%-80% of IPD (41). Serotypes 1, 4, 5, 7F, 8, 12F, 14, 18C, and 19A are more likely to cause IPD (29, 33, 42, 43, 45-47). Though serotypes 1 and 19A are predominantly responsible for invasive pneumococcal pneumonia, serotype 14 is still one of the most common etiologic agents of non-bacteremic pneumococcal pneumonia among adults in the era of PCV7 (65, 66). Serotype 1 pneumococcal meningitis is prevalent in the African meningitis belt, with a high case fatality rate (84), while meningitis by non-PCV7 serotypes has increased, with a preponderance for serotypes 19A and 22F in the US since routine PCV7 immunization (86). New manifestations of IPD, such as pediatric empyema and HUS, became more common in the era of PCV7 (69, 74, 98-100). Serotypes 1, 3, and 19A pneumococci are likely to cause empyema and HUS (76, 81, 100, 106, 107).
In contrast to the capsular serotype, the genotype is more closely associated with antibiotic resistance. CC320/271 strains with serotype 19A are multidrug-resistant and prevalent worldwide, particularly in North America and many Asian countries (129, 131). Several clones of multidrug-resistant serotype 6C pneumococci emerged in the US and Europe, and a multidrug-resistant 6D clone (ST282) has been identified in Korea (117-119, 138, 139).
After the introduction of PCV7 for pediatric patients, pre-existing nonvaccine serotypes expanded (serotype 19A), and new serotypes were identified (serotypes 6C, 6D, and 11E). Interestingly, serotype 6D comprises more than 10% of serogroup 6 in Korea, although it remains relatively uncommon in other areas (138, 139). Meanwhile, PCV13 was introduced for children in 2010. In turn, it was additionally licensed for adults in 2012 as the first conjugate vaccine for adults. In addition to the economic aspects (vaccination rates and cost-effectiveness), serotype distribution should be monitored to detect the emergence and expansion of undiscovered serotypes and recombinant capsular clones.
The pneumococcal epidemiology of capsule types varies geographically and temporally (13, 15). Knowledge of the serotype distribution is necessary for conjugate vaccine usage, but the seroepidemiological data is inadequate in many countries including Korea. A nationwide serosurveillance system is vital to establishing appropriate vaccination strategies for each country.
Figures and Tables
References
1. World Health Organization. 23-valent pneumococcal polysaccharide vaccine - WHO position paper. Wkly Epidemiol Rec. 2008. 373–384.
2. Laurichesse H, Romaszko JP, Nguyen LT, Souweine B, Poirier V, Guólon D, André M, Ruivard M, De Champs C, Caillaud D, et al. Clinical characteristics and outcome of patients with invasive pneumococcal disease, Puy-de-Dôme, France, 1994-1998. Eur J Clin Microbiol Infect Dis. 2001. 20:299–308.
3. Bravo LC. Overview of the disease burden of invasive pneumococcal disease in Asia. Vaccine. 2009. 27:7282–7291.
4. Pebody RG, Hellenbrand W, D'Ancona F, Ruutu P. Pneumococcal disease surveillance in Europe. Euro Surveill. 2006. 11:171–178.
5. Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, Jha P, Campbell H, Walker CF, Cibulskis R, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010. 375:1969–1987.
6. Park IH, Pritchard DG, Cartee R, Brandao A, Brandileone MC, Nahm MH. Discovery of a new capsular serotype (6C) within serogroup 6 of Streptococcus pneumoniae. J Clin Microbiol. 2007. 45:1225–1233.
7. Jin P, Kong F, Xiao M, Oftadeh S, Zhou F, Liu C, Russell F, Gilbert GL. First report of putative Streptococcus pneumoniae serotype 6D among nasopharyngeal isolates from Fijian children. J Infect Dis. 2009. 200:1375–1380.
8. Calix JJ, Porambo RJ, Brady AM, Larson TR, Yother J, Abeygunwardana C, Nahm MH. Biochemical, genetic and serological characterization of two capsule subtypes among streptococcus pneumoniae serotype 20 strains: discovery of a new pneumococcal serotype. J Biol Chem. 2012. 287:27885–27894.
9. Calix JJ, Dagan R, Pelton SI, Porat N, Nahm MH. Differential occurrence of Streptococcus pneumoniae serotype 11E between asymptomatic carriage and invasive pneumococcal disease isolates reflects a unique model of pathogen microevolution. Clin Infect Dis. 2012. 54:794–799.
10. Robbins JB, Austrian R, Lee CJ, Rastogi SC, Schiffman G, Henrichsen J, Mäkelä PH, Broome CV, Facklam RR, Tiesjema RH, et al. Considerations for formulating the second-generation pneumococcal capsular polysaccharide vaccine with emphasis on the cross-reactive types within groups. J Infect Dis. 1983. 148:1136–1159.
11. Käyhty H, Eskola J. New vaccines for the prevention of pneumococcal infections. Emerg Infect Dis. 1996. 2:289–298.
12. Advisory Committee on Immunization Practices. Preventing pneumococcal disease among infants and young children: recommendation of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2000. 49:1–35.
13. Hausdorff WP, Siber G, Paradiso PR. Geographical differences in invasive pneumococcal disease rates and serotype frequency in young children. Lancet. 2001. 357:950–952.
14. Hausdorff WP, Bryant J, Paradiso PR, Siber GR. Which pneumococcal serogroups cause the most invasive disease: implications for conjugate vaccine formulation and use. Part I. Clin Infect Dis. 2000. 30:100–121.
15. Harboe ZB, Benfield TL, Valentiner-Branth P, Hjuler T, Lambertsen L, Kaltoft M, Krogfelt K, Slotved HC, Christensen JJ, Konradsen HB. Temporal trends in invasive pneumococcal disease and pneumococcal serotypes over 7 decades. Clin Infect Dis. 2010. 50:329–337.
16. García-Rodríguez JA, Fresnadillo Martínez MJ. Dynamics of nasopharyngeal colonization by potential respiratory pathogens. J Antimicrob Chemother. 2002. 50:Suppl S2. 59–73.
17. Bogaert D, De Groot R, Hermans PW. Streptococcus pneumoniae colonisation: the key to pneumococcal disease. Lancet Infect Dis. 2004. 4:144–154.
18. Ferreira DM, Jambo KC, Gordon SB. Experimental human pneumococcal carriage models for vaccine research. Trends Microbiol. 2011. 19:464–470.
19. Gray BM, Converse GM 3rd, Dillon HC Jr. Epidemiologic studies of Streptococcus pneumoniae in infants: acquisition, carriage, and infection during the first 24 months of life. J Infect Dis. 1980. 142:923–933.
20. Brugger SD, Frey P, Aebi S, Hinds J, Mühlemann K. Multiple colonization with S. pneumoniae before and after introduction of the seven-valent conjugated pneumococcal polysaccharide vaccine. PLoS One. 2010. 5:e11638.
21. Turner P, Hinds J, Turner C, Jankhot A, Gould K, Bentley SD, Nosten F, Goldblatt D. Improved detection of nasopharyngeal cocolonization by multiple pneumococcal serotypes by use of latex agglutination or molecular serotyping by microarray. J Clin Microbiol. 2011. 49:1784–1789.
22. Abdullahi O, Nyiro J, Lewa P, Slack M, Scott JA. The descriptive epidemiology of Streptococcus pneumoniae and Haemophilus influenzae nasopharyngeal carriage in children and adults in Kilifi district, Kenya. Pediatr Infect Dis J. 2008. 27:59–64.
23. Adetifa IM, Antonio M, Okoromah CA, Ebruke C, Inem V, Nsekpong D, Bojang A, Adegbola RA. Pre-vaccination nasopharyngeal pneumococcal carriage in a Nigerian population: epidemiology and population biology. PLoS One. 2012. 7:e30548.
24. Scott JR, Millar EV, Lipsitch M, Moulton LH, Weatherholtz R, Perilla MJ, Jackson DM, Beall B, Craig MJ, Reid R, et al. Impact of more than a decade of pneumococcal conjugate vaccine use on carriage and invasive potential in Native American communities. J Infect Dis. 2012. 205:280–288.
25. Hill PC, Akisanya A, Sankareh K, Cheung YB, Saaka M, Lahai G, Greenwood BM, Adegbola RA. Nasopharyngeal carriage of Streptococcus pneumoniae in Gambian villagers. Clin Infect Dis. 2006. 43:673–679.
26. Mackenzie GA, Leach AJ, Carapetis JR, Fisher J, Morris PS. Epidemiology of nasopharyngeal carriage of respiratory bacterial pathogens in children and adults: cross-sectional surveys in a population with high rates of pneumococcal disease. BMC Infect Dis. 2010. 10:304.
27. Kim SM, Hur JK, Lee KY, Shin YK, Park SE, Ma SH, Min AY, Kang JH. Epidemiological study of pneumococcal nasal carriage and serotypes among Korean children. Korean J Pediatr. 2004. 47:611–616.
28. Cho EY, Kang HM, Lee J, Kang JH, Choi EH, Lee HJ. Changes in serotype distribution and antibiotic resistance of nasopharyngeal isolates of Streptococcus pneumoniae from children in Korea, after optional use of the 7-valent conjugate vaccine. J Korean Med Sci. 2012. 27:716–722.
29. Kronenberg A, Zucs P, Droz S, Mühlemann K. Distribution and invasiveness of Streptococcus pneumoniae serotypes in Switzerland, a country with low antibiotic selection pressure, from 2001 to 2004. J Clin Microbiol. 2006. 44:2032–2038.
30. Kim KH, Hong JY, Lee H, Kwak GY, Nam CH, Lee SY, Oh E, Yu J, Nahm MH, Kang JH. Nasopharyngeal pneumococcal carriage of children attending day care centers in Korea: comparison between children immunized with 7-valent pneumococcal conjugate vaccine and non-immunized. J Korean Med Sci. 2011. 26:184–190.
31. Smith T, Lehmann D, Montgomery J, Gratten M, Riley ID, Alpers MP. Acquisition and invasiveness of different serotypes of Streptococcus pneumoniae in young children. Epidemiol Infect. 1993. 111:27–39.
32. Ritchie ND, Mitchell TJ, Evans TJ. What is different about serotype 1 pneumococci? Future Microbiol. 2012. 7:33–46.
33. Sleeman KL, Griffiths D, Shackley F, Diggle L, Gupta S, Maiden MC, Moxon ER, Crook DW, Peto TE. Capsular serotype-specific attack rates and duration of carriage of Streptococcus pneumoniae in a population of children. J Infect Dis. 2006. 194:682–688.
34. Hostetter MK. Serotypic variations among virulent pneumococci in deposition and degradation of covalently bound C3b: implications for phagocytosis and antibody production. J Infect Dis. 1986. 153:682–693.
35. Nelson AL, Roche AM, Gould JM, Chim K, Ratner AJ, Weiser JN. Capsule enhances pneumococcal colonization by limiting mucus-mediated clearance. Infect Immun. 2007. 75:83–90.
36. Wartha F, Beiter K, Albiger B, Fernebro J, Zychlinsky A, Normark S, Henriques-Normark B. Capsule and D-alanylated lipoteichoic acids protect Streptococcus pneumoniae against neutrophil extracellular traps. Cell Microbiol. 2007. 9:1162–1171.
37. Weinberger DM, Trzciński K, Lu YJ, Bogaert D, Brandes A, Galagan J, Anderson PW, Malley R, Lipsitch M. Pneumococcal capsular polysaccharide structure predicts serotype prevalence. PLoS Pathog. 2009. 5:e1000476.
38. Kang YS, Kim JY, Bruening SA, Pack M, Charalambous A, Pritsker A, Moran TM, Loeffler JM, Steinman RM, Park CG. The C-type lectin SIGN-R1 mediates uptake of the capsular polysaccharide of Streptococcus pneumoniae in the marginal zone of mouse spleen. Proc Natl Acad Sci U S A. 2004. 101:215–220.
39. Melin M, Trzciński K, Meri S, Käyhty H, Väkeväinen M. The capsular serotype of Streptococcus pneumoniae is more important than the genetic background for resistance to complement. Infect Immun. 2010. 78:5262–5270.
40. Briles DE, Crain MJ, Gray BM, Forman C, Yother J. Strong association between capsular type and virulence for mice among human isolates of Streptococcus pneumoniae. Infect Immun. 1992. 60:111–116.
41. Hausdorff WP, Feikin DR, Klugman KP. Epidemiological differences among pneumococcal serotypes. Lancet Infect Dis. 2005. 5:83–93.
42. Brueggemann AB, Griffiths DT, Meats E, Peto T, Crook DW, Spratt BG. Clonal relationships between invasive and carriage Streptococcus pneumoniae and serotype- and clone-specific differences in invasive disease potential. J Infect Dis. 2003. 187:1424–1432.
43. Sá-Leão R, Pinto F, Aguiar S, Nunes S, Carrico JA, Frazão N, Goncalves-Sousa N, Melo-Cristino J, de Lencastre H, Ramirez M. Analysis of invasiveness of pneumococcal serotypes and clones circulating in Portugal before widespread use of conjugate vaccines reveals heterogeneous behavior of clones expressing the same serotype. J Clin Microbiol. 2011. 49:1369–1375.
44. Hanage WP, Kaijalainen TH, Syrjänen RK, Auranen K, Leinonen M, Mäkelä PH, Spratt BG. Invasiveness of serotypes and clones of Streptococcus pneumoniae among children in Finland. Infect Immun. 2005. 73:431–435.
45. Rivera-Olivero IA, del Nogal B, Sisco MC, Bogaert D, Hermans PW, de Waard JH. Carriage and invasive isolates of Streptococcus pneumoniae in Caracas, Venezuela: the relative invasiveness of serotypes and vaccine coverage. Eur J Clin Microbiol Infect Dis. 2011. 30:1489–1495.
46. Shouval DS, Greenberg D, Givon-Lavi N, Porat N, Dagan R. Site-specific disease potential of individual Streptococcus pneumoniae serotypes in pediatric invasive disease, acute otitis media and acute conjunctivitis. Pediatr Infect Dis J. 2006. 25:602–607.
47. Yildirim I, Hanage WP, Lipsitch M, Shea KM, Stevenson A, Finkelstein J, Huang SS, Lee GM, Kleinman K, Pelton SI. Serotype specific invasive capacity and persistent reduction in invasive pneumococcal disease. Vaccine. 2010. 29:283–288.
48. Rodgers GL, Arguedas A, Cohen R, Dagan R. Global serotype distribution among Streptococcus pneumoniae isolates causing otitis media in children: potential implications for pneumococcal conjugate vaccines. Vaccine. 2009. 27:3802–3810.
49. Casey JR, Adlowitz DG, Pichichero ME. New patterns in the otopathogens causing acute otitis media six to eight years after introduction of pneumococcal conjugate vaccine. Pediatr Infect Dis J. 2010. 29:304–309.
50. Mahjoub-Messai F, Doit C, Mariani-Kurkdjian P, Francois M, Bingen E. Epidemiology of acute otitis media caused by Streptococcus pneumoniae: emergence of serotype 19A. Arch Pediatr. 2008. 15:1713–1716.
51. Jansen AG, Rodenburg GD, van der Ende A, van Alphen L, Veenhoven RH, Spanjaard L, Sanders EA, Hak E. Invasive pneumococcal disease among adults: associations among serotypes, disease characteristics, and outcome. Clin Infect Dis. 2009. 49:e23–e29.
52. Rodríguez MA, González AV, Gavín MA, Martínez FM, Marín NG, Blázquez BR, Moreno JC. Invasive pneumococcal disease: association between serotype, clinical presentation and lethality. Vaccine. 2011. 29:5740–5746.
53. Yildirim I, Stevenson A, Hsu KK, Pelton SI. Evolving picture of invasive pneumococcal disease in Massachusetts children: a comparison of disease in 2007-2009 with earlier periods. Pediatr Infect Dis J. 2012. 31:1016–1021.
54. Weinberger DM, Harboe ZB, Sanders EA, Ndiritu M, Klugman KP, Ruckinger S, Dagan R, Adegbola R, Cutts F, Johnson HL, et al. Association of serotype with risk of death due to pneumococcal pneumonia: a meta-analysis. Clin Infect Dis. 2010. 51:692–699.
55. Harboe ZB, Thomsen RW, Riis A, Valentiner-Branth P, Christensen JJ, Lambertsen L, Krogfelt KA, Konradsen HB, Benfield TL. Pneumococcal serotypes and mortality following invasive pneumococcal disease: a population-based cohort study. PLoS Med. 2009. 6:e1000081.
56. van Hoek AJ, Andrews N, Waight PA, George R, Miller E. Effect of serotype on focus and mortality of invasive pneumococcal disease: coverage of different vaccines and insight into non-vaccine serotypes. PLoS ONE. 2012. 7:e39150.
57. Niederman MS. Review of treatment guidelines for community-acquired pneumonia. Am J Med. 2004. 117:Suppl 3A. 51S–57S.
58. Brandenburg JA, Marrie TJ, Coley CM, Singer DE, Obrosky DS, Kapoor WN, Fine MJ. Clinical presentation, processes and outcomes of care for patients with pneumococcal pneumonia. J Gen Intern Med. 2000. 15:638–646.
59. Burman LA, Trollfors B, Andersson B, Henrichsen J, Juto P, Kallings I, Lagergård T, Möllby R, Norrby R. Diagnosis of pneumonia by cultures, bacterial and viral antigen detection tests, and serology with special reference to antibodies against pneumococcal antigens. J Infect Dis. 1991. 163:1087–1093.
60. Cillóniz C, Ewig S, Polverino E, Muñoz-Almagro C, Marco F, Gabarrús A, Menéndez R, Mensa J, Torres A. Pulmonary complications of pneumococcal community-acquired pneumonia: incidence, predictors, and outcomes. Clin Microbiol Infect. 2012. 18:1134–1142.
61. Briles DE, Hollingshead SK, Paton JC, Ades EW, Novak L, van Ginkel FW, Benjamin WH Jr. Immunizations with pneumococcal surface protein A and pneumolysin are protective against pneumonia in a murine model of pulmonary infection with Streptococcus pneumoniae. J Infect Dis. 2003. 188:339–348.
62. Gentile A, Bardach A, Ciapponi A, Garcia-Marti S, Aruj P, Glujovsky D, Calcagno JI, Mazzoni A, Colindres RE. Epidemiology of community-acquired pneumonia in children of Latin America and the Caribbean: a systematic review and meta-analysis. Int J Infect Dis. 2012. 16:e5–e15.
63. Bender JM, Ampofo K, Korgenski K, Daly J, Pavia AT, Mason EO, Byington CL. Pneumococcal necrotizing pneumonia in Utah: does serotype matter? Clin Infect Dis. 2008. 46:1346–1352.
64. Resti M, Moriondo M, Cortimiglia M, Indolfi G, Canessa C, Becciolini L, Bartolini E, de Benedictis FM, de Martino M, Azzari C. Community-acquired bacteremic pneumococcal pneumonia in children: diagnosis and serotyping by real-time polymerase chain reaction using blood samples. Clin Infect Dis. 2010. 51:1042–1049.
65. Burgos J, Falcó V, Borrego A, Sordé R, Larrosa MN, Martinez X, Planes AM, Sánchez A, Palomar M, Rello J, et al. Impact of the emergence of non-vaccine pneumococcal serotypes on the clinical presentation and outcome of adults with invasive pneumococcal pneumonia. Clin Microbiol Infect. 2012. doi: 10.1111/j.1469-0691.2012.03895.x.
66. Bewick T, Sheppard C, Greenwood S, Slack M, Trotter C, George R, Lim WS. Serotype prevalence in adults hospitalised with pneumococcal non-invasive community-acquired pneumonia. Thorax. 2012. 67:540–545.
67. Pande A, Nasir S, Rueda AM, Matejowsky R, Ramos J, Doshi S, Kulkarni P, Musher DM. The incidence of necrotizing changes in adults with pneumococcal pneumonia. Clin Infect Dis. 2012. 54:10–16.
68. Yangco BG, Deresinski SC. Necrotizing or cavitating pneumonia due to Streptococcus pneumoniae: report of four cases and review of the literature. Medicine (Baltimore). 1980. 59:449–457.
69. Byington CL, Korgenski K, Daly J, Ampofo K, Pavia A, Mason EO. Impact of the pneumococcal conjugate vaccine on pneumococcal parapneumonic empyema. Pediatr Infect Dis J. 2006. 25:250–254.
70. Eastham KM, Freeman R, Kearns AM, Eltringham G, Clark J, Leeming J, Spencer DA. Clinical features, aetiology and outcome of empyema in children in the north east of England. Thorax. 2004. 59:522–525.
71. Obando I, Arroyo LA, Sánchez-Tatay D, Moreno D, Hausdorff WP, Brueggemann AB. Molecular typing of pneumococci causing parapneumonic empyema in Spanish children using multilocus sequence typing directly on pleural fluid samples. Pediatr Infect Dis J. 2006. 25:962–963.
72. Weil-Olivier C, Levy C, Marguet C, Sardet A, de La Rocque F, Lécuyer A, Cohen R. Groupe des Pédiatres et Pneumopédiatres. Multicenter pediatric retrospective study on pneumonia with empyema in France. Arch Pediatr. 2005. 12:823–826.
73. Buckingham SC, King MD, Miller ML. Incidence and etiologies of complicated parapneumonic effusions in children, 1996 to 2001. Pediatr Infect Dis J. 2003. 22:499–504.
74. Gupta R, Crowley S. Increasing paediatric empyema admissions. Thorax. 2006. 61:179–180.
75. Langley JM, Kellner JD, Solomon N, Robinson JL, Le Saux N, McDonald J, Ulloa-Gutierrez R, Tan B, Allen U, Dobson S, et al. Empyema associated with community-acquired pneumonia: a Pediatric Investigator's Collaborative Network on Infections in Canada (PICNIC) study. BMC Infect Dis. 2008. 8:129.
76. Lee JH, Kim SH, Lee J, Choi EH, Lee HJ. Diagnosis of pneumococcal empyema using immunochromatographic test on pleural fluid and serotype distribution in Korean children. Diagn Microbiol Infect Dis. 2012. 72:119–124.
77. Yu J, Salamon D, Marcon M, Nahm MH. Pneumococcal serotypes causing pneumonia with pleural effusion in pediatric patients. J Clin Microbiol. 2011. 49:534–538.
78. Byington CL, Hulten KG, Ampofo K, Sheng X, Pavia AT, Blaschke AJ, Pettigrew M, Korgenski K, Daly J, Mason EO. Molecular epidemiology of pediatric pneumococcal empyema from 2001 to 2007 in Utah. J Clin Microbiol. 2010. 48:520–525.
79. Muñoz-Almagro C, Gala S, Selva L, Jordan I, Tarragó D, Pallares R. DNA bacterial load in children and adolescents with pneumococcal pneumonia and empyema. Eur J Clin Microbiol Infect Dis. 2011. 30:327–335.
80. Obando I, Muñoz-Almagro C, Arroyo LA, Tarrago D, Sanchez-Tatay D, Moreno-Perez D, Dhillon SS, Esteva C, Hernandez-Bou S, Garcia-Garcia JJ, et al. Pediatric parapneumonic empyema, Spain. Emerg Infect Dis. 2008. 14:1390–1397.
81. Burgos J, Lujan M, Falcó V, Sánchez A, Puig M, Borrego A, Fontanals D, Planes AM, Pahissa A, Rello J. The spectrum of pneumococcal empyema in adults in the early 21st century. Clin Infect Dis. 2011. 53:254–261.
82. O'Brien KL, Wolfson LJ, Watt JP, Henkle E, Deloria-Knoll M, McCall N, Lee E, Mulholland K, Levine OS, Cherian T, et al. Burden of disease caused by Streptococcus pneumoniae in children younger than 5 years: global estimates. Lancet. 2009. 374:893–902.
83. Kisakye A, Makumbi I, Nansera D, Lewis R, Braka F, Wobudeya E, Chaplain D, Nalumansi E, Mbabazi W, Gessner BD. Surveillance for Streptococcus pneumoniae meningitis in children aged <5 years: implications for immunization in Uganda. Clin Infect Dis. 2009. 48:Suppl 2. S153–S161.
84. Gessner BD, Mueller JE, Yaro S. African meningitis belt pneumococcal disease epidemiology indicates a need for an effective serotype 1 containing vaccine, including for older children and adults. BMC Infect Dis. 2010. 10:22.
85. Brueggemann AB, Spratt BG. Geographic distribution and clonal diversity of Streptococcus pneumoniae serotype 1 isolates. J Clin Microbiol. 2003. 41:4966–4970.
86. Hsu HE, Shutt KA, Moore MR, Beall BW, Bennett NM, Craig AS, Farley MM, Jorgensen JH, Lexau CA, Petit S, et al. Effect of pneumococcal conjugate vaccine on pneumococcal meningitis. N Engl J Med. 2009. 360:244–256.
87. Annand WF, Bowen WH. Pneumococcal peritonitis. Lancet. 1906. 1:1591–1597.
88. McCartney JE, Fraser J. Pneumococcal peritonitis. Br J Surg. 1922. 9:479–489.
89. Fowler R. Primary peritonitis: changing aspects 1956-1970. Aust Paediatr J. 1971. 7:73–83.
90. Correia JP, Conn HO. Spontaneous bacterial peritonitis in cirrhosis: endemic or epidemic? Med Clin North Am. 1975. 59:963–981.
91. Epstein M, Calia FM, Gabuzda GJ. Pneumococcal peritonitis in patients with postnecrotic cirrhosis. N Engl J Med. 1968. 278:69–73.
92. Pahmer M. Pneumococcal peritonitis in nephrotic and non-nephrotic children. J Pediatr. 1940. 17:90–95.
93. Hemsley C, Eykyn SJ. Pneumococcal peritonitis in previously healthy adults: case report and review. Clin Infect Dis. 1998. 27:376–379.
94. Sirotnak AP, Eppes SC, Klein JD. Tuboovarian abscess and peritonitis caused by Streptococcus pneumoniae serotype 1 in young girls. Clin Infect Dis. 1996. 22:993–996.
95. Andrade AL, Toscano CM, Minamisava R, Costa PS, Andrade JG. Pneumococcal disease manifestation in children before and after vaccination: what's new? Vaccine. 2011. 29:Suppl 3. C2–C14.
96. Cabrera GR, Fortenberry JD, Warshaw BL, Chambliss CR, Butler JC, Cooperstone BG. Hemolytic uremic syndrome associated with invasive Streptococcus pneumoniae infection. Pediatrics. 1998. 101:699–703.
97. Kaplan SL, Mason EO Jr, Barson WJ, Wald ER, Arditi M, Tan TQ, Schutze GE, Bradley JS, Givner LB, Kim KS, et al. Three-year multicenter surveillance of systemic pneumococcal infections in children. Pediatrics. 1998. 102:538–545.
98. Brandt J, Wong C, Mihm S, Roberts J, Smith J, Brewer E, Thiagarajan R, Warady B. Invasive pneumococcal disease and hemolytic uremic syndrome. Pediatrics. 2002. 110:371–376.
99. Lee CS, Chen MJ, Chiou YH, Shen CF, Wu CY, Chiou YY. Invasive pneumococcal pneumonia is the major cause of paediatric haemolytic-uraemic syndrome in Taiwan. Nephrology (Carlton). 2012. 17:48–52.
100. Waters AM, Kerecuk L, Luk D, Haq MR, Fitzpatrick MM, Gilbert RD, Inward C, Jones C, Pichon B, Reid C, et al. Hemolytic uremic syndrome associated with invasive pneumococcal disease: the United Kingdom experience. J Pediatr. 2007. 151:140–144.
101. Klein PJ, Bulla M, Newman RA, Müller P, Uhlenbruck G, Schaefer HE, Krüger G, Fisher R. Thomsen-Friedenreich antigen in haemolytic-uraemic syndrome. Lancet. 1977. 2:1024–1025.
102. Ramasethu J, Luban N. T activation. Br J Haematol. 2001. 112:259–263.
103. Huang YH, Lin TY, Wong KS, Huang YC, Chiu CH, Lai SH, Hsia SH. Hemolytic uremic syndrome associated with pneumococcal pneumonia in Taiwan. Eur J Pediatr. 2006. 165:332–335.
104. von Vigier RO, Fossali E, Crosazzo L, Bianchetti MG. Positive Coombs test in postpneumococcal hemolytic-uremic syndrome. Pediatr Infect Dis J. 2005. 24:1028–1029.
105. Oggioni MR, Trappetti C, Kadioglu A, Cassone M, Iannelli F, Ricci S, Andrew PW, Pozzi G. Switch from planktonic to sessile life: a major event in pneumococcal pathogenesis. Mol Microbiol. 2006. 61:1196–1210.
106. Bender JM, Ampofo K, Byington CL, Grinsell M, Korgenski K, Daly JA, Mason EO, Pavia AT. Epidemiology of Streptococcus pneumoniae-induced hemolytic uremic syndrome in Utah children. Pediatr Infect Dis J. 2010. 29:712–716.
107. Copelovitch L, Kaplan BS. Streptococcus pneumoniae--associated hemolytic uremic syndrome: classification and the emergence of serotype 19A. Pediatrics. 2010. 125:e174–e182.
108. Merieau E, Lanotte P, Chantreuil J, Cantagrel S. Streptococcus pneumoniae 19A-induced hemolytic-uremic syndrome: a new pathology? Arch Pediatr. 2008. 15:1825–1827.
109. Hsieh YC, Wang JT, Lee WS, Hsueh PR, Shao PL, Chang LY, Lu CY, Lee CY, Huang FY, Huang LM. Serotype competence and penicillin resistance in Streptococcus pneumoniae. Emerg Infect Dis. 2006. 12:1709–1714.
110. Trzciński K, Thompson CM, Lipsitch M. Single-step capsular transformation and acquisition of penicillin resistance in Streptococcus pneumoniae. J Bacteriol. 2004. 186:3447–3452.
111. Ardanuy C, Tubau F, Pallares R, Calatayud L, Domínguez MA, Rolo D, Grau I, Martín R, Liñares J. Epidemiology of invasive pneumococcal disease among adult patients in Barcelona before and after pediatric 7-valent pneumococcal conjugate vaccine introduction, 1997-2007. Clin Infect Dis. 2009. 48:57–64.
112. Kaplan SL, Barson WJ, Lin PL, Stovall SH, Bradley JS, Tan TQ, Hoffman JA, Givner LB, Mason EO Jr. Serotype 19A Is the most common serotype causing invasive pneumococcal infections in children. Pediatrics. 2010. 125:429–436.
113. Shin J, Baek JY, Kim SH, Song JH, Ko KS. Predominance of ST320 among Streptococcus pneumoniae serotype 19A isolates from 10 Asian countries. J Antimicrob Chemother. 2011. 66:1001–1004.
114. Farrell DJ, Jenkins SG, Brown SD, Patel M, Lavin BS, Klugman KP. Emergence and spread of Streptococcus pneumoniae with erm(B) and mef(A) resistance. Emerg Infect Dis. 2005. 11:851–858.
115. Song JH, Chang HH, Suh JY, Ko KS, Jung SI, Oh WS, Peck KR, Lee NY, Yang Y, Chongthaleong A, et al. Macrolide resistance and genotypic characterization of Streptococcus pneumoniae in Asian countries: a study of the Asian Network for Surveillance of Resistant Pathogens (ANSORP). J Antimicrob Chemother. 2004. 53:457–463.
116. Choi EH, Kim SH, Eun BW, Kim SJ, Kim NH, Lee J, Lee HJ. Streptococcus pneumoniae serotype 19A in children, South Korea. Emerg Infect Dis. 2008. 14:275–281.
117. Green MC, Mason EO, Kaplan SL, Lamberth LB, Stovall SH, Givner LB, Bradley JS, Tan TQ, Barson WJ, Hoffman JA, et al. Increase in prevalence of Streptococcus pneumoniae serotype 6C at Eight Children's Hospitals in the United States from 1993 to 2009. J Clin Microbiol. 2011. 49:2097–2101.
118. Ko KS, Baek JY, Song JH. Multidrug-resistant Streptococcus pneumoniae serotype 6D clones in South Korea. J Clin Microbiol. 2012. 50:818–822.
119. Rolo D, Fenoll A, Ardanuy C, Calatayud L, Cubero M, de la Campa AG, Liñares J. Trends of invasive serotype 6C pneumococci in Spain: emergence of a new lineage. J Antimicrob Chemother. 2011. 66:1712–1718.
120. Zhuo F, Xiao M, Kong F, Oftadeh S, Zhou F, Zhang J, Gilbert GL. Prevalence and genetic diversity of pneumococcal serogroup 6 in Australia. Clin Microbiol Infect. 2011. 17:1246–1253.
121. Yao KH, Liu ZJ, Yu JG, Yu SJ, Yuan L, Nahm MH, Yang YH. Type distribution of serogroup 6 Streptococcus pneumoniae and molecular epidemiology of newly identified serotypes 6C and 6D in China. Diagn Microbiol Infect Dis. 2011. 70:291–298.
122. Nahm MH, Oliver MB, Siira L, Kaijalainen T, Lambertsen LM, Virolainen A. A report of Streptococcus pneumoniae serotype 6D in Europe. J Med Microbiol. 2011. 60:46–48.
123. Mercado E, Srinivasan V, Hawkins P, Chochua S, Ochoa T, Beall B, McGee L. First report of Streptococcus pneumoniae serotype 6D in South America. J Clin Microbiol. 2011. 49:2080–2081.
124. Kuch A, Sadowy E, Skoczyńska A, Hryniewicz W. First report of Streptococcus pneumoniae serotype 6D isolates from invasive infections. Vaccine. 2010. 28:6406–6407.
125. Ho PL, Ang I, Chow KH, Lai EL, Chiu SS. The prevalence and characteristics of Streptococcus pneumoniae isolates expressing serotypes 6C and 6D in Hong Kong prior to the introduction of the 7-valent pneumococcal conjugate vaccine. Diagn Microbiol Infect Dis. 2010. 68:439–444.
126. Chang B, Otsuka T, Iwaya A, Okazaki M, Matsunaga S, Wada A. Isolation of Streptococcus pneumoniae serotypes 6C and 6D from the nasopharyngeal mucosa of healthy Japanese children. Jpn J Infect Dis. 2010. 63:381–383.
127. Bratcher PE, Kim KH, Kang JH, Hong JY, Nahm MH. Identification of natural pneumococcal isolates expressing serotype 6D by genetic, biochemical and serological characterization. Microbiology. 2010. 156:555–560.
128. Adam HJ, Karlowsky JA, Nichol KA, Gilmour MW, Hoban DJ, Embree J, Zhanel GG. Baseline epidemiology of Streptococcus pneumoniae serotypes in Canada prior to the introduction of the 13-valent pneumococcal vaccine. Microb Drug Resist. 2012. 18:176–182.
129. Kim SH, Song JH, Chung DR, Thamlikitkul V, Yang Y, Wang H, Lu M, So TM, Hsueh PR, Yasin RM, et al. Changing trends in antimicrobial resistance and serotypes of Streptococcus pneumoniae isolates in Asian countries: an Asian Network for Surveillance of Resistant Pathogens (ANSORP) study. Antimicrob Agents Chemother. 2012. 56:1418–1426.
130. Moore MR, Gertz RE Jr, Woodbury RL, Barkocy-Gallagher GA, Schaffner W, Lexau C, Gershman K, Reingold A, Farley M, Harrison LH, et al. Population snapshot of emergent Streptococcus pneumoniae serotype 19A in the United States, 2005. J Infect Dis. 2008. 197:1016–1027.
131. Beall BW, Gertz RE, Hulkower RL, Whitney CG, Moore MR, Brueggemann AB. Shifting genetic structure of invasive serotype 19A pneumococci in the United States. J Infect Dis. 2011. 203:1360–1368.
132. Mahjoub-Messai F, Doit C, Koeck JL, Billard T, Evrard B, Bidet P, Hubans C, Raymond J, Levy C, Cohen R, et al. Population snapshot of Streptococcus pneumoniae serotype 19A isolates before and after introduction of seven-valent pneumococcal Vaccination for French children. J Clin Microbiol. 2009. 47:837–840.
133. Aguiar SI, Pinto FR, Nunes S, Serrano I, Melo-Cristino J, Sá-Leão R, Ramirez M, de Lencastre H. Denmark14-230 clone as an increasing cause of pneumococcal infection in Portugal within a background of diverse serotype 19A lineages. J Clin Microbiol. 2010. 48:101–108.
134. Ansaldi F, Canepa P, de Florentiis D, Bandettini R, Durando P, Icardi G. Increasing incidence of Streptococcus pneumoniae serotype 19A and emergence of two vaccine escape recombinant ST695 strains in Liguria, Italy, 7 years after implementation of the 7-valent conjugated vaccine. Clin Vaccine Immunol. 2011. 18:343–345.
135. Tarragó D, Aguilar L, García R, Gimenez MJ, Granizo JJ, Fenoll A. Evolution of clonal and susceptibility profiles of serotype 19A Streptococcus pneumoniae among invasive isolates from children in Spain, 1990 to 2008. Antimicrob Agents Chemother. 2011. 55:2297–2302.
136. Nunes S, Valente C, Sá-Leão R, de Lencastre H. Temporal trends and molecular epidemiology of recently described serotype 6C of Streptococcus pneumoniae. J Clin Microbiol. 2009. 47:472–474.
137. Park IH, Moore MR, Treanor JJ, Pelton SI, Pilishvili T, Beall B, Shelly MA, Mahon BE, Nahm MH. Differential effects of pneumococcal vaccines against serotypes 6A and 6C. J Infect Dis. 2008. 198:1818–1822.
138. Choi EH, Lee HJ, Cho EY, Oh CE, Eun BW, Lee J, Kim MJ. Prevalence and genetic structures of Streptococcus pneumoniae serotype 6D, South Korea. Emerg Infect Dis. 2010. 16:1751–1753.
139. Baek JY, Ko KS, Song JH. Streptococcus pneumoniae serotype 6D cross-reacting with serotype 6A, 6B, and 6C factor sera. J Clin Microbiol. 2011. 49:765–766.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download