Abstract
While the disease course of stress-induced cardiomyopathy (SIC) is usually benign, it can be fatal. The prognostic factors to predict poorer outcome are not well established, however. We analyzed the Acute Physiology And Chronic Health Evaluation (APACHE) II score to assess its value for predicting poor prognosis in patients with SIC. Thirty-seven consecutive patients with SIC were followed prospectively during their hospitalization. Clinical factors, including APACHE II score, coronary angiogram, echocardiography and cardiac enzymes at presentation were analyzed. Of the 37 patients, 27 patients (73%) were women. The mean age was 66.1 ± 15.6 yr, and the most common presentation was chest pain (38%). Initial echocardiographic left ventricular ejection fraction (EF) was 42.5% ± 9.3%, and the wall motion score index (WMSI) was 1.9 ± 0.3. Six patients (16%) expired during the follow-up period of hospitalization. Based on the analysis of characteristics and clinical factors, the only predictable variable in prognosis was APACHE II score. The patients with APACHE II score greater than 20 had tendency to expire than the others (P = 0.001). Based on present study, APACHE II score more than 20, rather than cardiac function, is associated with mortality in patients with SIC.
Stress-induced cardiomyopathy (SIC) typically presents as transient cardiac dysfunction with unique apical ballooning (1). Management is generally supportive, and, because the cardiac dysfunction at presentation is almost transient and reversible, it is reasonably treated with standard medication for left ventricular systolic dysfunction (2). Although the prognosis for SIC is usually favorable, it can be fatal in up to 8% of hospitalized cases (3-6). In spite of the possibility of death, little effort has been made to identify predictive factors for poor prognosis in SIC.
The Acute Physiology And Chronic Health Evaluation (APACHE) II score is a well-known disease severity index for hospitalized adults that has a solid relationship with predicting the mortality of critically ill patients (7). We analyzed the value of the APACHE II score for predicting poor prognosis in hospitalized patients with SIC.
Between June 2006 and October 2010, 3,100 patients were seen in our institutions with suspected acute coronary syndrome (ACS). Of these, 37 patients fulfilled the following criteria (1, 8) for SIC: 1) older than 18 yr; 2) transient akinesia/dyskinesia beyond a single major coronary artery vascular distribution; 3) absence of significant coronary artery disease upon coronary angiogram (CAG) and 4) the presence of definite antecedent physical or mental trigger factors, identified by the attending physicians. No patients had a preexisting cardiomyopathy, intracranial bleeding, or pheochromocytoma. We applied ergonovine echocardiography to all patients diagnosed with SIC to rule out coronary vasospasm within two days after CAG, and there was no patient with positive finding on the test.
We reviewed medical records for chief complaint, smoking history, and co-morbidities. We also investigated the presence of physical stress (septic shock, surgery, or intubation, etc.) or mental stress (anger management issues, death of loved one, or interpersonal conflicts, etc.). Body mass index (BMI), level of cardiac enzymes (creatine kinase MB fraction, CK-MB; troponin-I), high sensitive C-reactive protein (hsCRP), systolic and diastolic blood pressure (BP), heart rate (HR), and Killip class were evaluated at the time of diagnosis for SIC.
Standardized electrocardiography (ECG) and echocardiographic studies were examined at the time of diagnosis and one or two weeks later to confirm the status of recovery. If regional wall motion abnormality (RWMA), observed on the first echocardiogram, was not definitely improved on the second one, a third echocardiogram was performed a few weeks after the second one. All patients showed resolution of RWMA. In echocardiography studies, we measured the left ventricular ejection fraction (LVEF) and regional wall motion score index (WMSI) to determine the severity of cardiac dysfunction. The LVEF was measured using the modified Simpson's method, and WMSI was calculated using all views, including the parasternal short axis and long axis and apical four chamber views. We classified ventricular ballooning into two categories, typical and atypical apical ballooning, based on the location of ballooning. Standard 2-dimensional and Doppler echocardiography was performed using a 2.5 MHz transducer with harmonic imaging. We used a Philips iE33 system (Philips Medical Systems, USA) for patients admitted to the general ward and ViVid I (GE Ultrasound, Horten, Norway) for patients in the intensive care unit. We calculated the APACHE II score, with the worst physiologic parameters during the first 24 hr after the event, to measure the clinical severity of each patient's objective physical condition upon presentation. APACHE II is composed of vital signs, serum creatinine level, oxygen pressure in arterial blood gas analysis, blood acidity, degree of leukocytosis, level of hematocrit, severity of electrolyte imbalance, Glasgow coma scale (GCS; representing patient mental status), and age of patient, each recorded at the most severe level in 24 hr (7).
All statistical analyses were performed using SPSS software (version 18.0, SPSS Inc, Chicago, IL, USA). Continuous variables were expressed as mean ± SD or mean with interquartile ranges. Frequencies and percentages were used to describe categorical variables and were compared based on the result of ROC curve analysis with Fisher's exact test. Continuous variables of the two groups (Group I and II, divided by APACHE II score 20) were analyzed and compared using the student T-test. To estimate the sensitivity and specificity of the APACHE II score for predicting death, ROC curve analysis was done. Kaplan-Meier survival analysis was performed to estimate the mortality according to survival period. Statistical significance was defined as P < 0.05 in all of the analyses.
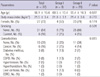
To find out the variable which is able to predict the outcomes of patients exceedingly, we analyzed the baseline characteristics and the clinical factors of patients, including the cardiac functions, in terms of LVEF and WMSI, cardiac enzymes, such as CK-MB and TnI, and APACHE II score based on survival (Table 1). And we figured out that APACHE II score was significantly different between the dead and the survived among multiple clinical variables (22.5 ± 1.6 vs 11.7 ± 6.2, P value = 0.001). Even though SIC is a kind of cardiomyopathy, the abnormalities in ECG, the shape of apical ballooning, the heart functions and cardiac markers did not show any significant difference between two groups. And more male patients were included in the death group than survival group (67% vs 19%, P value = 0.035). Based on this result, we carried out receiver operating characteristics (ROC) curve analysis to confirm the availability of APACHE II score as a prognostic marker. According to the result of ROC curve analysis we divided the patients into group I (APACHE II score > 20) and group II (APACHE II score ≤ 20), because APACHE II score 20 showed higher sensitivity and specificity than any other scores (Fig. 1). The comparison between group I and group II was done to find out any other clinical factors, which is related to the prognosis, as described beneath.
The baseline characteristics of patients are presented in Table 2. The mean age was 66.1 ± 15.6 yr old, and the mean BMI was 21.5 ± 3.4 kg/m2. Twenty-seven (73%) of 37 patients were female, and 31 (84%) were non-smokers. One third of the subjects had comorbidities, with cancer being most common (n = 6, 16%). Except for a few comorbidities, such as cancer or chronic obstructive pulmonary disease (COPD), most of them were not related to SIC itself.
The comparisons of clinical characteristics of the subjects are presented in Table 3. Physical stress, such as sepsis, surgery, or acidosis, was reported more often than mental stress in both groups (100% vs 0% in group I and 79% vs 21% in group II, respectively). Even though not described in the tables, operation was largest number of physical stress, followed by severe pneumonia, acute pyelonephritis, and acute exacerbation of COPD. And The most frequent initial symptom on presentation was chest pain (n = 14, 38%), followed by dyspnea, altered mentality and hypotension, with dyspnea in group I and chest pain in group II being the most common respectively. ECG on presentation showed no remarkable arrhythmia. Among ECG abnormalities, T wave inversion was most common (n = 16, 43%), followed by ST elevation and ST depression. Corrected QT interval (QTc) was prolonged at the time of diagnosis (485.3 ± 55.5 ms). Serum cardiac enzymes were elevated in all patients, and were not statistically different between groups. In the echocardiographic study at the time of diagnosis, mean LVEF was 42.5% ± 9.3%, and mean WMSI was 1.9 ± 0.3 and those are not significantly different between two groups (P value = 0.573 and 0.516, respectively). There was no significant difference in the proportion of typical ballooning between groups, although all patients in group I had typical ballooning at presentation (100% vs 79%, P value = 0.305). ROC curve indicated a high sensitivity (100%) and specificity (94%) of the APACHE II score for predicting death, with a threshold score of greater than 20 (Fig. 1). The APACHE II score at diagnosis was significantly higher in group I as compared to group II (22.1 ± 1.6 vs 11.0 ± 5.9, P = 0.001). Among multiple components of the APACHE II score, only maximal heart rate and Glascow coma scale were higher in group I. Six in group I and no one in group II died during hospitalization, all with physical stress and 4 of them were male (Table 4). Their mean APACHE II score and LVEF were 22.5 (range 21-25) and 40.5% (range 26%-49%), respectively. Mean time to death from diagnosis was 25 days (range 2-111 days). Kaplan-Meier survival curve shows significant difference in cumulative survival between two groups divided by APACHE II score 20 (Fig. 2).
In this prospective observational study, we could identify a few findings, as follows. First, the most frequent symptom was chest pain. This observation, similar result with another study in Korea (9), suggests that SIC should be one of the differential diagnoses for chest pain in conjunction with ACS. Second, the prevalence of SIC was much higher in women than men, even though there is no proven study about the reason of this preponderance associated with gender. The last, in spite of its old name 'broken heart syndrome', the patients were more connected with physical stress than mental stress.
We also found that the APACHE II score more than 20, rather than cardiac functions, was associated with mortality in patients with SIC, even though there was no study which proposed any prognostic factors using any kind of scoring systems. Most of studies with SIC were about its epidemiology, and the studies, interested in prognostic factor, were focusing only to cardiac findings, such as EKG results or cardiac markers. Based on our results, we suggest that outcomes may depend more upon the physical conditions of the patients than the severity of the symptoms or signs of cardiac dysfunction.
To the best of our knowledge, there have been few attempts to evaluate a scoring system, like the APACHE II, for patient physical condition and SIC prognosis. We hypothesized that the APACHE II score would correlate with patient prognosis, particularly mortality, and sought to identify other factors with prognostic value. After confirmation that APACHE II score on diagnosis was related to prognosis, we also found that an APACHE II score greater than 20 had a high sensitivity (100%) and specificity (94%) for predicting in-hospital death in patients with SIC (Fig. 1).
Among the components of the APACHE II score, maximal heart rate and GCS (a marker of consciousness regardless of inotropic or sedative use) were increased more in patients who had APACHE II score greater than 20. ECG could potentially offer information about the prognosis of SIC patients. Our findings were in agreement with previous research, however, showing no link between electrocardiographic abnormalities and poor outcome (10). Overall, we saw that the prevalence of SIC was higher in females, as expected (1, 4, 6).
There are a few limitations in our study. Despite the prospective enrollment of SIC patients, we could only offer a single center experience with a relatively small number of subjects, which was inevitable due to the low prevalence of SIC. Above this, we could not measure the relation between stress and prognosis, because there was no proven method for quantitative analysis of the physical and mental stress. And the cardiac functions were not evaluated with echocardiography in daily routine follow-up and at the time of death, nevertheless Lee et al. (11). suggested that the absence of left ventricular function recovery within a week could predict the poor outcome of patients. And the follow-up echocardiography was not done at right time, because of many reasons concerned with their refusals, short hospitalization and cost problems.
The prospective study comparing the characteristics, clinical factors and prognosis according to the threshold score of APACHE II score 20 should be performed, to confirm that it would be high sensitive and specific standard in predicting prognosis. The proper echocardiographic and cardiac marker follow-up should be considered, to make sure that the cardiac function and myocardial damages are not related to the prognosis of SIC. Given the small size of our study population, larger, prospective long-term observational studies are needed to confirm and validate these findings.
The APACHE II score is higher in SIC patients who was dead, and the score of greater than 20, rather than cardiac function, is associated with mortality. It is able to give more information to physicians, regarding to the prognosis of SIC patients.
Figures and Tables
Fig. 1
ROC curve of APACHE II score in predicting death in patients with stress-induced cardiomyopathy.

Fig. 2
Kaplan-Meier survival curve shows significant difference in cumulative survival between two groups divided by APACHE II score 20.

References
1. Kawai S, Kitabatake A, Tomoike H. Takotsubo Cardiomyopathy Group. Guidelines for diagnosis of takotsubo (ampulla) cardiomyopathy. Circ J. 2007. 71:990–992.
2. Bybee KA, Kara T, Prasad A, Lerman A, Barsness GW, Wright RS, Rihal CS. Systematic review: transient left ventricular apical ballooning: a syndrome that mimics ST-segment elevation myocardial infarction. Ann Intern Med. 2004. 141:858–865.
3. Tsuchihashi K, Ueshima K, Uchida T, Oh-mura N, Kimura K, Owa M, Yoshiyama M, Miyazaki S, Haze K, Ogawa H, Honda T, Hase M, Kai R, Morii I. Angina Pectoris-Myocardial Infarction Investigations in Japan. Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. Angina Pectoris-Myocardial Infarction Investigations in Japan. J Am Coll Cardiol. 2001. 38:11–18.
4. Sharkey SW, Lesser JR, Zenovich AG, Maron MS, Lindberg J, Longe TF, Maron BJ. Acute and reversible cardiomyopathy provoked by stress in women from the United States. Circulation. 2005. 111:472–479.
5. Akashi YJ, Goldstein DS, Barbaro G, Ueyama T. Takotsubo cardiomyopathy: a new form of acute, reversible heart failure. Circulation. 2008. 118:2754–2762.
6. Sharkey SW, Windenburg DC, Lesser JR, Maron MS, Hauser RG, Lesser JN, Haas TS, Hodges JS, Maron BJ. Natural history and expansive clinical profile of stress (tako-tsubo) cardiomyopathy. J Am Coll Cardiol. 2010. 55:333–341.
7. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985. 13:818–829.
8. Hahn JY, Gwon HC, Park SW, Choi SH, Choi JH, Choi JO, Lee SC, On YK, Kim JS, Kim DK, Jeon ES, Lee SH, Hong KP, Park JE. The clinical features of transient left ventricular nonapical ballooning syndrome: comparison with apical ballooning syndrome. Am Heart J. 2007. 154:1166–1173.
9. Lee HH, Gwon HC, Kim BJ, Lee KJ, Im ES, Won KH, Sung JD, Lee SC, Park SW, Kim DK, Lee SH, Seo JD. Clinical manifestation of novel stress-induced cardiomyopathy mimicking acute myocardial infarction: single center prospective registry. Korean Circ J. 2002. 32:1054–1063.
10. Dib C, Asirvatham S, Elesber A, Rihal C, Friedman P, Prasad A. Clinical correlates and prognostic significance of electrocardiographic abnormalities in apical ballooning syndrome (Takotsubo/stress-induced cardiomyopathy). Am Heart J. 2009. 157:933–938.
11. Lee PH, Song JK, Sun BJ, Choi HO, Seo JS, Na JO, Kim DH, Song JM, Kang DH, Kim JJ, Park SW. Outcomes of patients with stress-induced cardiomyopathy diagnosed by echocardiography in a tertiary referral hospital. J Am Soc Echocardiogr. 2010. 23:766–771.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download