Abstract
Abdominal fat accumulation is known to be strongly implicated in development of metabolic syndrome (MetS). We examined diagnostic values of obesity-related parameters in 95 men and 185 women, and we determined optimal cutoff values of visceral fat area (VFA) and waist circumference (WC) for predicting the presence of multiple non-adipose components of MetS. Receiver operating characteristic (ROC) curve analysis revealed that VFA was the best indicator of MetS. WC and VFA exhibited similar diagnostic values for men and postmenopausal women, whereas WC was inferior to VFA for premenopausal women (area under ROC curve of VFA and WC was 0.76 and 0.52, respectively; P < 0.001). Optimal cutoff points of VFA and WC for predicting MetS were 136 cm2 and 89 cm in men and 95 cm2 and 82 cm in women, respectively. Subjects with VFA and WC above these cutoff values exhibited increased insulin resistance and increased carotid intima-media thickness. In conclusion, WC has a diagnostic value similar to VFA for predicting MetS in men and postmenopausal women, but not in premenopausal women. Further studies are necessary to develop a simple clinical parameter that reflects visceral fat in premenopausal women.
Metabolic syndrome (MetS) is an important public health problem and it increases the risk of type 2 diabetes and cardiovascular disease (1). Although the pathogenesis of MetS has yet to be determined, it is evident that the abdominal fat accumulation plays a central role (2). Compared to the subcutaneous abdominal fat, the visceral abdominal fat confers more of a risk of metabolic and cardiovascular complications. This notion may be explained by the fact that the visceral fat has a higher lipolytic activity and it directly releases free fatty acids into the portal circulation, and this considerably contributes to insulin resistance (3). In addition, abdominal obesity has been strongly implicated in the development of MetS as well as increased all-cause and cardiovascular mortality (3, 4).
The International Diabetes Federation (IDF) includes abdominal obesity as an essential element of MetS and the IDF has defined the waist circumference (WC) cutoff values according to ethnicity and gender (e.g., the WC values of 90 cm for men and 80 cm for women in South Asia and China) (5). Compared to Caucasians, Asians typically exhibit a higher risk of obesity-related morbidity and mortality at a given body mass index (BMI) or WC (6). Furthermore, in the Obesity in Asia Collaboration, which evaluated the optimal WC cutoff values for the identification of diabetes in 155,122 individuals from 10 countries in the Asia-Pacific region (86% Asian; 2 study populations were from Australia), the cutoff values were 85 cm for men and 80 cm for women (7). This study showed that the prevalence of diabetes was consistently higher among Asians than that of Europeans at any given level of the BMI or WC. This clarifies the ethnic differences in the relationship between being overweight and having diabetes.
WC measurement is a simple and widely applicable method to evaluate central obesity (8). However, it does not accurately reflect the abdominal visceral fat mass since it is also influenced by the amount of subcutaneous fat. The currently available methods that reliably measure the amount of abdominal visceral fat include computed tomography (CT) and magnetic resonance imaging (MRI). CT and MRI can distinguish fat from other tissues and they allow measurement of the visceral and subcutaneous abdominal fat mass independently with high reproducibility (9, 10). Nevertheless, these methods are disadvantageous for routine use due to the radiation exposure, the technical difficulties and the high cost. In this regard, other methods of assessing the amount of visceral fat such as ultrasonography and the abdominal sagittal diameter have been suggested (11, 12). New, alternative, simple and noninvasive methods that can accurately reflect the visceral fat need to be developed. Therefore, we examined the diagnostic values and optimal cutoff points of various obesity-related parameters, including the CT-measured visceral fat area (VFA), to predict the risk of MetS in Korean men and women. In addition, we investigated whether these cutoff levels are useful in reflecting other markers of insulin resistance and atherosclerosis (e.g., the homeostasis model assessment for insulin resistance [HOMA-IR] and the mean carotid intima-media thickness [IMT]).
A total of 280 subjects (95 men and 185 women) aged 30-80 yr were recruited by local advertisement. The exclusion criteria consisted of the following: 1) an age < 30 or > 80 yr, 2) any individuals taking medications for hypertension, hyperglycemia, hyperlipidemia or obesity, and 3) pregnancy. The menopausal status in women was checked by self-report of the regularity of their menstrual cycle.
The height and body weight were measured to the nearest 0.1 cm and 0.1 kg, respectively, with the subjects standing barefoot and in light clothing. The BMI was calculated as the body weight in kilograms divided by the square of the height in meters. The WC was measured at the midpoint between the inferior border of the subcostal margin and iliac crest in the mid-axillary line after normal expiration with the subject standing; the hip girth was measured at the widest part of the hip across both greater trochanters, from which the waist-to-hip circumference ratio (WHR) was calculated. Blood pressure was measured using a mercury sphygmomanometer in a sitting position after the participants had remained seated for 10 min. The measurements were taken twice, 5 min apart.
After an overnight 12 hr fast, the plasma glucose, total cholesterol, triglyceride and high-density lipoprotein (HDL) cholesterol concentrations were measured enzymatically using an auto-analyzer (ADVIA 1650; Siemens Medical Solutions Diagnostics, Tarrytown, NY, USA). The plasma insulin concentrations were measured by radioimmunoassay (BioSource S. A., Nivelles, Belgium). The HOMA-IR was calculated using the following equation: HOMA-IR = (fasting insulin [µU/mL] × fasting glucose [mM/L])/22.5 (13).
A single CT scan (Sensation 16; Siemens AG, Forchheim, Germany) at the level of the L4-5 vertebra was obtained with the patient in the supine position and at the end of inspiration. The cross-sectional area of fat was determined with attenuation values selected between the range of -250 and -50 Hounsfield units and using commercial software (Rapidia; Infinitt, Seoul, Korea). Carotid ultrasound studies were performed once for each subject by a single technician using a linear probe. The mean IMT of the common carotid artery was measured by an ultrasonography apparatus (Logic 7; GE Medical Systems, Milwaukee, WI, USA) equipped with IMT measurement software (Intimascope; Media Cross Co., Tokyo, Japan) (14).
MetS was defined according to the IDF criteria (5). The IDF has defined MetS as the presence of central obesity (WC ≥ 90 cm in men, WC ≥ 80 cm in women) plus two or more of the following criteria: 1) a systolic blood pressure (SBP) ≥ 130 mmHg and/or a diastolic blood pressure (DBP) ≥ 85 mmHg; 2) HDL cholesterol < 40 mg/dL in men, < 50 mg/dL in women; 3) triglyceride ≥ 150 mg/dL and 4) the fasting plasma glucose ≥ 100 mg/dL.
Statistical analyses were conducted using SPSS version 11.5 for Windows (SPSS Inc., Chicago, IL, USA). Continuous variables were expressed as means ± standard deviations (SD). Each variable was examined for normality, and the skewed variables were tested after log-transformation. Continuous variables were compared by Student's t-test and the frequencies were compared by Pearson chi-squared test. The ROC curve analyses were performed to determine the optimal cutoff points for the VFA, the WC, the BMI, the WHR, the subcutaneous fat area (SFA) and the visceral-to-subcutaneous fat area ratio (V/S) for identifying the subjects with two or more components of MetS other than the WC. Comparisons of the diagnostic values of the tests were performed using the areas under the curves (AUC), and the significance of the difference between the two areas was assessed by the method described by Hanley and McNeil (15). The values of various obesity-related indices that resulted in maximizing the Youden index (sensitivity + specificity - 1) were defined as optimal (16). The WC and BMI values corresponding to each VFA cutoff were calculated by simple linear regression analysis. P values < 0.05 (two-tailed) were considered to be statistically significant.
The clinical characteristics of the study subjects are shown in Table 1. The prevalence of MetS according to the diagnostic criteria of IDF was 28.4% in the men and 19.5% in the women. The proportion of subjects having central obesity, which is defined as a WC ≥ 90 cm in men and a WC ≥ 80 cm in women, was 42.1% in the men and 57.3% in the women. The proportion of subjects having higher blood pressure, which is defined as a SBP ≥ 130 mmHg and/or a DBP ≥ 85 mmHg, was 29.5% in the men and 12.4% in the women. Regarding the triglyceride levels, 36.8% of the men and 18.9% of the women had triglyceride levels ≥ 150 mg/dL. A low HDL cholesterol level, which is defined as < 40 mg/dL in men and < 50 mg/dL in women, was seen in 45.3% of the men and 58.9% of the women. The proportion of subjects having fasting hyperglycemia, which is defined as ≥ 100 mg/dL, was 31.6% in the men and 11.9% in the women.
Table 2 presents the AUC values, the statistical significance of the difference between the AUC value of each parameter and that of the VFA, the optimal cutoff points of six obesity-related indices for detecting two or more components of MetS other than WC, and the sensitivity and specificity of the cutoff point. The AUC of the VFA was comparable with that of the WC, BMI or SFA in men, whereas the VFA showed significantly higher AUC values than did the WC, BMI, WHR or SFA in women. The optimal cutoff points of the VFA, SFA, V/S, WC, BMI, and WHR were 136.0 cm2, 134.0 cm2, 1.0, 89.0 cm, 24.1 kg/m2, and 0.9 in men, and 95.0 cm2, 213.0 cm2, 0.5, 85 cm, 24.0 kg/m2, and 0.9 in women, respectively. The sensitivity and specificity at the optimal cutoff points of the VFA were 74.3% and 78.3% in men and 79.1% and 77.4% in women, respectively, whereas those values at the optimal cutoff points of the WC were 69.8% and 70.6% in men and 51.0% and 81.3% in women, respectively. Subgroup analyses according to the menopausal status in women showed that the AUC of the VFA was significantly higher than that of the WC, BMI, or WHR in premenopausal women, whereas it was comparable to that of the WC, BMI, or WHR in postmenopausal women. The optimal cutoff points of the VFA, WC, and BMI were 87.3 cm2, 85.0 cm, and 25.2 kg/m2 in the postmenopausal women and 81.7 cm2, 81.0 cm, and 23.1 kg/m2 in the premenopausal women, respectively.
Fig. 1 shows the relationship of the WC and BMI with the VFA for the men and women. The WC and BMI values corresponding to the optimal cutoff points of the VFA were estimated by a simple linear regression equation. There was a significant correlation between the VFA and WC (r = 0.733, P < 0.001 for the men and r = 0.652, P < 0.001 for the women) and between the VFA and BMI (r = 0.612, P < 0.001 for the men and r = 0.608, P < 0.001 for the women). The WC corresponding to the VFA cutoff was 89 cm for the men and 82 cm for the women. The BMI corresponding to the VFA cutoff was 25.2 kg/m2 for the men and 24.5 kg/m2 for the women. Subgroup analyses according to the menopausal status in women showed that the VFA appeared to have better correlation with the WC and BMI in the postmenopausal women compared to that of the premenopausal women (r = 0.650, P < 0.001 and r = 0.630, P < 0.001 for the postmenopausal women and r = 0.581, P < 0.001 and r = 0.535, P < 0.001 for the premenopausal women). The WC and BMI corresponding to the VFA cutoff were 81 cm and 23.8 kg/m2 for the premenopausal women and 81 cm and 23.7 kg/m2 for the postmenopausal women, respectively (Fig. 2).
Fig. 3 shows the mean IMT and HOMA-IR according to the cutoff points of the VFA (136 cm2 for the men and 95 cm2 for the women) and WC (89 cm for the men and 82 cm for the women). The subjects who had a WC above the cutoff points exhibited higher values of the IMT (0.76 mm vs 0.70 mm, P = 0.021 for the men and 0.73 mm vs 0.67 mm, P = 0.001 for the women) and an elevated HOMA-IR (2.23 vs 1.18, P = 0.001 for the men and 1.57 vs 1.28, P = 0.024 for the women) as compared to their counterparts. Although the VFA displayed a similar trend with the WC, the IMT in men and the HOMA-IR in women were marginally higher for the subjects with a VFA above the cutoff points than those values for the subjects with a VFA below the cutoff points (0.76 mm vs 0.71 mm, P = 0.08 for the men and 1.56 vs 1.32, P = 0.069 for the women).
Fig. 4. shows the prevalence of MetS in the 4 groups that were subdivided by the VFA and WC cutoffs: 1) a lower VFA and a lower WC (a VFA below the cutoff and a WC below the cutoff), 2) a lower VFA and a higher WC (a VFA below the cutoff and a WC above the cutoff), 3) a higher VFA and a lower WC (a VFA above the cutoff and a WC below the cutoff), and 4) a higher VFA and a higher WC (a VFA above the cutoff and a WC above the cutoff) group. For the men, a WC cutoff value was associated with the prevalence of MetS among the subjects who had a VFA below the cutoff point (50.0% in the lower VFA and higher WC group vs 13.9% in the lower VFA and lower WC group, P = 0.042), but not among subjects who had a VFA above the cutoff point (72.4% in the higher VFA and higher WC group vs 71.4% in the higher VFA and lower WC group, P = 0.645). By contrast, for the women, the WC cutoff value was not associated with the prevalence of MetS among the subjects who had a VFA below the cutoff point (10.7% in the lower VFA and lower WC group vs 3.4% in the lower VFA and higher WC group, P = 0.224) and among subjects who had a VFA above the cutoff point (54.3% in the higher VFA and higher WC group vs 53.3% in the higher VFA and lower WC group, P = 0.589).
Our results demonstrated that the cutoff points of the VFA, which are 136 cm2 for men and 95 cm2 for women, are optimal for yielding the maximal sensitivity plus specificity for predicting two or more components of MetS other than the WC. To date, a few previous studies have determined the optimal cutoff points of the VFA for MetS in the Korean population. Han et al. (17) analyzed the data from a hospital-based sample of 276 Korean men (age: 45.5 ± 9.4 yr, BMI: 25.4 ± 2.5 kg/m2) and 540 Korean women (age: 40.7 ± 12.2 yr, BMI: 25.4 ± 2.7 kg/m2). They suggested 100 cm2 in men and 70 cm2 in women as the optimal cutoff points for identifying subjects with multiple risk factors of MetS as defined by the IDF criteria (17). In another Korean study, the VFA cutoff level was proposed to be 103.8 cm2 for both men (age: 41.3 ± 11.6 yr, BMI: 30.9 ± 5.2 kg/m2) and women (age: 43.2 ± 13.1 yr, BMI: 29.9 ± 5.7 kg/m2) (18). In 1,870 Japanese subjects (the mean age and BMI were 50.6 ± 7.8 yr and 24.9 ± 2.7 kg/m2 in men and 51.2 ± 7.2 yr and 23.5 ± 3.1 kg/m2 in women, respectively), the cutoff points of the VFA and WC for identifying subjects with at least two non-adipose components of MetS were 132.6 cm2 and 89.8 cm in men and 91.5 cm2 and 82.3 cm in women, respectively (19), which are quite similar to our results. They also showed that the VFA is a better parameter than the WC or BMI for detecting multiple metabolic risk factors (19). The results from these studies and ours suggest that the VFA cutoff levels for identifying subjects with multiple metabolic risk factors are influenced by the age and the BMI distribution of the study populations.
Previous studies have reported that insulin resistance is more strongly associated with the VFA rather than with the WHR or the WC (20). As the WC reflects not only visceral fat but also subcutaneous fat, it does not appear to be a good indicator of the VFA (21). Intriguingly, our current study displayed a gender difference in the diagnostic values of the VFA and other obesity-related anthropometric parameters for predicting non-adipose components of MetS. Subgroup analyses showed that for the men, the WC cutoff value was associated with the prevalence of MetS among the subjects who had a VFA below the cutoff point. However, only the VFA cutoff value, and not WC cutoff value, was associated with the prevalence of MetS in women (Fig. 4). In addition, although the AUC of the WC was comparable to that of the VFA in men, the WC exhibited a significantly lower AUC than the VFA in women, and more precisely in the premenopausal women, which indicates that the WC has limited value for predicting MetS in premenopausal women. In our study, the premenopausal women displayed a significantly lower V/S than did the postmenopausal women (0.43 vs 0.54, respectively, P < 0.001). Therefore, it can be concluded that the WC is more influenced by subcutaneous fat than by visceral fat in premenopausal women. In accordance with our finding, a recent study has demonstrated that the VFA rather than the WC itself is a major determinant of MetS in premenopausal Korean women (22), whereas the WC and VFA are similarly useful in identifying MetS in elderly Korean women (23). Since the body fat distribution is determined by several factors, including age, gender, and the menopausal status (24), different methods and cutoff values for predicting MetS may be necessary even in a single ethnic group. Especially, in premenopausal women, the directly measured VFA or a simple clinical measurement reflecting the VFA would be indispensable for predicting MetS.
We found significant differences in the mean IMT and HOMA-IR between the subgroups, as were divided by the WC cutoff point of 89 cm in men and 82 cm in women (Fig. 3). The HOMA-IR is an indicator of insulin resistance, and the IMT of the common carotid artery is an indicator of atherosclerosis and they have both proposed as independent predictors of cardiovascular disease (25, 26). In line with our results, the WC has been associated with surrogate measures of insulin resistance and atherosclerosis and with their progression in several population-based cross-sectional and longitudinal studies (27-29). Therefore, the WC cutoff values presented in this study may be useful for predicting insulin resistance and subclinical atherosclerosis, although they are slightly inferior to the VFA for identifying subjects with multiple non-adipose components of MetS.
In summary, this study demonstrates that the diagnostic values of the VFA and WC for predicting the presence of multiple metabolic risk factors are influenced by gender and the menopausal status. The optimal cutoff points of the VFA and WC for reflecting multiple non-adipose components of MetS were 136 cm2 and 89 cm in men and 95 cm2 and 82 cm in women, respectively. Further, these cutoff values may indicate an increased HOMA-IR and IMT. Although the WC and VFA are useful to a similar extent in men and postmenopausal women, the WC is inferior to the VFA in premenopausal women. It is mandatory to develop a simple clinical parameter that reflects visceral fat in premenopausal women.
Figures and Tables
Fig. 1
Body mass index and waist circumference corresponding to the visceral fat area (VFA) cutoff values for men and women.

Fig. 2
Body mass index and waist circumference corresponding to the visceral fat area (VFA) cutoff values for pre- and post-menopausal women.
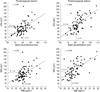
Fig. 3
Mean IMT and HOMA-IR according to the cutoff point of the visceral fat area (VFA) and waist circumference (WC) for men and women.

Fig. 4
Prevalence of metabolic syndrome according to the cutoff point of the visceral fat area (VFA) and waist circumference (WC) for men and women.

Table 2
Areas under the ROC curve for the obesity-related parameters as well as the sensitivity and specificity at the optimal cutoff point for detecting two or more components of metabolic syndrome other than waist circumference

*P value compared with the visceral fat area by the method of Hanley and McNeil (19). ROC, receiver operating characteristic; VFA, visceral fat area; WC, waist circumference; BMI, body mass index; WHR, waist-to-hip circumference ratio; V/S, visceral-to-subcutaneous fat area ratio; SFA, subcutaneous fat area ratio.
AUTHOR SUMMARY
Gender Differences in Diagnostic Values of Visceral Fat Area and Waist Circumference for Predicting Metabolic Syndrome in Koreans
Hong Il Kim, Jin Taek Kim, Sung Hoon Yoo, Soo Heon Kwak, Hak Chul Jang, Kyong Soo Park, Seong Yeon Kim, Hong Kyu Lee and Young Min Cho
Receiver operating characteristic (ROC) curve analysis revealed that the optimal cutoff points of visceral fat area and waist circumference for predicting metabolic syndrome in Korean population were 136 cm2 and 89 cm in men and 95 cm2 and 82 cm in women, respectively. The subjects with visceral fat area and waist circumference above these cutoff values exhibited increased insulin resistance and an increased carotid intima-media thickness. Diagnostic values of the obesity-related parameters for predicting metabolic syndrome are influenced by gender and the menopausal status. The waist circumference and visceral fat area exhibited similar diagnostic values for men and postmenopausal women, whereas waist circumference was inferior to visceral fat area for premenopausal women. Therefore, a simple clinical parameter that reflects visceral fat in premenopausal women needs to be developed.
References
1. Gami AS, Witt BJ, Howard DE, Erwin PJ, Gami LA, Somers VK, Montori VM. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol. 2007. 49:403–414.
2. Després JP. Abdominal obesity as important component of insulin-resistance syndrome. Nutrition. 1993. 9:452–459.
3. Carr DB, Utzschneider KM, Hull RL, Kodama K, Retzlaff BM, Brunzell JD, Shofer JB, Fish BE, Knopp RH, Kahn SE. Intra-abdominal fat is a major determinant of the National Cholesterol Education Program Adult Treatment Panel III criteria for the metabolic syndrome. Diabetes. 2004. 53:2087–2094.
4. Pischon T, Boeing H, Hoffmann K, Bergmann M, Schulze MB, Overvad K, van der Schouw YT, Spencer E, Moons KG, Tjønneland A, Halkjaer J, Jensen MK, Stegger J, Clavel-Chapelon F, Boutron-Ruault MC, Chajes V, Linseisen J, Kaaks R, Trichopoulou A, Trichopoulos D, Bamia C, Sieri S, Palli D, Tumino R, Vineis P, Panico S, Peeters PH, May AM, Bueno-de-Mesquita HB, van Duijnhoven FJ, Hallmans G, Weinehall L, Manjer J, Hedblad B, Lund E, Agudo A, Arriola L, Barricarte A, Navarro C, Martinez C, Quirós JR, Key T, Bingham S, Khaw KT, Boffetta P, Jenab M, Ferrari P, Riboli E. General and abdominal adiposity and risk of death in Europe. N Engl J Med. 2008. 359:2105–2120.
5. Alberti KG, Zimmet P, Shaw J. Metabolic syndrome: a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med. 2006. 23:469–480.
6. Misra A, Vikram NK, Gupta R, Pandey RM, Wasir JS, Gupta VP. Waist circumference cutoff points and action levels for Asian Indians for identification of abdominal obesity. Int J Obes (Lond). 2006. 30:106–111.
7. Huxley R, Barzi F, Lee CM, Lear S, Shaw J, Lam TH, Caterson I, Azizi F, Patel J, Suriyawongpaisal P, Oh SW, Kang JH, Gill T, Zimmet P, James PT, Woodward M. Waist circumference thresholds provide an accurate and widely applicable method for the discrimination of diabetes. Diabetes Care. 2007. 30:3116–3118.
8. Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr. 2004. 79:379–384.
9. Ross R, Léger L, Morris D, de Guise J, Guardo R. Quantification of adipose tissue by MRI: relationship with anthropometric variables. J Appl Physiol. 1992. 72:787–795.
10. Thaete FL, Colberg SR, Burke T, Kelley DE. Reproducibility of computed tomography measurement of visceral adipose tissue area. Int J Obes Relat Metab Disord. 1995. 19:464–467.
11. Kim SK, Kim HJ, Hur KY, Choi SH, Ahn CW, Lim SK, Kim KR, Lee HC, Huh KB, Cha BS. Visceral fat thickness measured by ultrasonography can estimate not only visceral obesity but also risks of cardiovascular and metabolic diseases. Am J Clin Nutr. 2004. 79:593–599.
12. Pouliot MC, Després JP, Lemieux S, Moorjani S, Bouchard C, Tremblay A, Nadeau A, Lupien PJ. Waist circumference and abdominal sagittal diameter: best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women. Am J Cardiol. 1994. 73:460–468.
13. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985. 28:412–419.
14. Yanase T, Nasu S, Mukuta Y, Shimizu Y, Nishihara T, Okabe T, Nomura M, Inoguchi T, Nawata H. Evaluation of a new carotid intima-media thickness measurement by B-mode ultrasonography using an innovative measurement software, intimascope. Am J Hypertens. 2006. 19:1206–1212.
15. Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983. 148:839–843.
16. Youden WJ. Index for rating diagnostic tests. Cancer. 1950. 3:32–35.
17. Han JH, Park HS, Kim SM, Lee SY, Kim DJ, Choi WH. Visceral adipose tissue as a predictor for metabolic risk factors in the Korean population. Diabet Med. 2008. 25:106–110.
18. Kim JA, Choi CJ, Yum KS. Cut-off values of visceral fat area and waist circumference: diagnostic criteria for abdominal obesity in a Korean population. J Korean Med Sci. 2006. 21:1048–1053.
19. Oka R, Kobayashi J, Yagi K, Tanii H, Miyamoto S, Asano A, Hagishita T, Mori M, Moriuchi T, Kobayashi M, Katsuda S, Kawashiri MA, Nohara A, Takeda Y, Mabuchi H, Yamagishi M. Reassessment of the cutoff values of waist circumference and visceral fat area for identifying Japanese subjects at risk for the metabolic syndrome. Diabetes Res Clin Pract. 2008. 79:474–481.
20. Brochu M, Starling RD, Tchernof A, Matthews DE, Garcia-Rubi E, Poehlman ET. Visceral adipose tissue is an independent correlate of glucose disposal in older obese postmenopausal women. J Clin Endocrinol Metab. 2000. 85:2378–2384.
21. Bonora E, Micciolo R, Ghiatas AA, Lancaster JL, Alyassin A, Muggeo M, DeFronzo RA. Is it possible to derive a reliable estimate of human visceral and subcutaneous abdominal adipose tissue from simple anthropometric measurements? Metabolism. 1995. 44:1617–1625.
22. Hyun YJ, Kim OY, Jang Y, Ha JW, Chae JS, Kim JY, Yeo HY, Paik JK, Lee JH. Evaluation of metabolic syndrome risk in Korean premenopausal women: not waist circumference but visceral fat. Circ J. 2008. 72:1308–1315.
23. Seo JA, Kim BG, Cho H, Kim HS, Park J, Baik SH, Choi DS, Park MH, Jo SA, Koh YH, Han C, Kim NH. The cutoff values of visceral fat area and waist circumference for identifying subjects at risk for metabolic syndrome in elderly Korean: Ansan Geriatric (AGE) cohort study. BMC Public Health. 2009. 9:443.
24. Enzi G, Gasparo M, Biondetti PR, Fiore D, Semisa M, Zurlo F. Subcutaneous and visceral fat distribution according to sex, age, and overweight, evaluated by computed tomography. Am J Clin Nutr. 1986. 44:739–746.
25. Jeppesen J, Hansen TW, Rasmussen S, Ibsen H, Torp-Pederson C, Madsbad S. Insulin resistance, the metabolic syndrome, and risk of incident cardiovascular disease: a population-based study. J Am Coll Cardiol. 2007. 49:2112–2119.
26. Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE. Common carotid intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam Study. Circulation. 1997. 96:1432–1437.
27. Tabata S, Yoshimitsu S, Hamachi T, Abe H, Ohnaka K, Kono S. Waist circumference and insulin resistance: a cross-sectional study of Japanese men. BMC Endocr Disord. 2009. 9:1.
28. Park K, Lee DH, Erickson DJ, Himes JH, Shikany JM, Jacobs DR Jr. Association of long-term change in waist circumference with insulin resistance. Obesity. 2010. 18:370–376.
29. Hassinen M, Lakka TA, Komulainen P, Haapala I, Nissinen A, Rauramaa R. Association of waist and hip circumference with 12-year progression of carotid intima-media thickness in elderly women. Int J Obes (Lond). 2007. 31:1406–1411.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download