Abstract
We report a patient with Lewis-Sumner syndrome (LSS) who showed an improvement only with plasma exchange (PE). The patient, 32-yr old man, had progressive multifocal motor-sensory deficits with persistent, multiple conduction blocks and marked slowing of NCVs. Nerve pathology supported a diagnosis of demyelinating neuropathy by revealing marked loss of myelinated fibers with inter- and intrafascicular variation. Although the patient was refractory to treatment with corticosteroid and intravenous immunoglobulin, PE produced a dramatic improvement. Our experience strongly proposes that PE should be tried for refractory LSS.
Lewis-Sumner syndrome (LSS), first reported by Lewis et al., is characterized by sensorimotor deficits starting in distal upper limb and demyelinating mononeuropathy multiplex with persistent conduction blocks involving both motor and sensory nerves (1). LSS has many synonyms, such as multifocal motor and sensory demyelinating neuropathy (MMSDN), upper limb predominant multifocal chronic inflammatory demyelinating polyneuropathy, multifocal acquired demyelinating sensory and motor neuropathy (MADSAM), and multifocal inflammatory demyelinating neuropathy (2-5). These nosologic confusions are produced by various views from many neurologists who have endeavored to differentiate the disease from chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) and multifocal motor neuropathy (MMN). Since LSS has many similarities with and also some distinguishing features from CIDP and MMN, there is still controversy whether it is a variant of CIDP, an intermediate link between CIDP and MMN, or a distinct clinical entity (5, 6). Although the identity of LSS is being disagreed on a concept, most of reports have been in agreement with the fact that either intravenous immune globulin (IVIg) or corticosteroid is the most effective in a majority of patients. Thus, these immunomodulating therapies are now regarded as a standard therapeutic modality for LSS (7-9). Although LSS is thought of a treatable disorder with these drugs, 10 to 20% of patients are still remained non-responders.
We report a patient with chronic relapsing form of LSS, who was refractory to standard treatment regimens for LSS even with typical clinical, electrophysiological and pathologic findings, but showed an improvement exclusively with plasma exchange (PE).
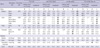
A 32-yr old fireman presented with tingling paresthesia in right fingers lasting for one month. Two months before admission, he had experienced muscle weakness in left fourth and fifth fingers and paresthesia with numbness in left palm. On admission, following muscle weakness was recorded: medical research council grade 3 (G3) in left wrist flexion, finger flexion and finger fanning, and G4 in left wrist extension and finger extension. Atrophy of small hand muscles was accompanied. Sensory system was abnormal revealing decreased pinprick and light touch sensation in left medial palm and right third finger (Fig. 1). All deep tendon reflexes (DTR) were lost. Nerve conduction study (NCS) on first admission is summarized in Table 1 and Fig. 2; conduction block and slowing of nerve conduction velocities (NCVs) in right median nerve were recorded, and complete conduction block and no compound nerve action potential (CNAP) were obtained in motor and sensory conduction studies of left ulnar nerve, respectively. Serum antibodies against myelin components such as GM1, GD1b, GQ1b, and MAG were all negative, and immunofixation and immunoelectrophoresis were unremarkable. CSF protein was not elevated (22 mg/L, normal; 15-45 mg/L). Other laboratory tests excluded diagnosable peripheral neuropathies. Based on above results, an inflammatory demyelinating neuropathy was considered as a possible diagnosis. Therefore, intravenous methylprednisolone 1 g/day for five days followed by the maintenance with oral prednisolone 1 mg/kg/day were treated. However, neither improvement nor further aggravation occurred.
Third attack has come two months after the second one; he complained of right ankle dorsiflexion weakness, suggesting the affection of right deep peroneal nerve, as well as worsening of preceding symptoms in bilateral arms. He was again treated with intravenous methylprednisolone (1 g/day for 7 days) followed by intravenous immunoglobulin (IVIg, 0.4 g/kg/day for 5 days), but these symptoms were sustained without improvement.
Being progressively disabled in his job and daily life (e.g. driving a car) with neurologic deficits accumulated, he readmitted four months after the third episode. There was obvious worsening of median and ulnar nerve conduction in electrophysiological study, as shown in Table 1. Ultrasonography, which was tried on median and ulnar nerves, disclosed enlarged nerve diameter and loss of normal lobulated pattern inside nerves, suggesting that there was an inflammatory response in these nerves. Oral prednisolone (an initial dose of 1 mg/kg/day) was started with slow tapering over several months, and azathioprine (an initial dose of 1 mg/kg/day) was subsequently added. Despite of various therapeutic trials, preceding symptoms were not improved. Furthermore, left wrist drop (fourth episode), but which was spontaneously recovered, and then left abducens nerve palsy (fifth episode) were subsequently reported with three to four month-intervals.
When he admitted with left abducens palsy as the fifth attack, the affection of right superficial peroneal nerve was also suspected in physical examination because he newly complained of numbness in anterolateral aspect of right lower leg and dorsum of right foot. Nerve conduction study comparably revealed reduced CNAP amplitude and slowed sensory NCV in right superficial peroenal nerve, as well as persistent multiple conduction blocks and marked slowing of NCVs in median and ulnar nerves even though there was some improvement in these nerves (Table 1). This result ultimately made it possible to take nerve biopsy on right superficial peroneal nerve. Nerve pathology was quite remarkable; interfascicular variation was observed, simultaneously displaying severely affected fascicles that lost most of myelinated fibers and relatively preserved ones (Fig. 3A). Semithin sections stained with toluidine blue showed prominent hypertrophy of myelinated fibers and onion bulb formation, which suggests the repeated episodes of demyelination and remyelination (Fig. 3B). There was no evidence of either vasculitis or perivascular inflammation. Based on above findings of nerve pathology, we could ultimately confirm the diagnosis of LSS.
As the treatment with steroid, azathioprine and IVIg were not helpful at all, plasma exchange (hereafter PE) with exchanged plasma volume of 3,850 mL five times every other day, was finally tried. Surprisingly, dramatic improvement was followed; left abducens palsy was reversed immediately after PE, and motor and sensory deficits in left upper and right lower extremities were progressively recovered. Partial improvement in electrophysiological study was also accompanied. Three months after PE, the patient could return back to his job only with mild dorsiflexion weakness in right ankle and decreased sensation in right dorsal foot. Five months later he declared mild weakness and paresthesia in right hand at the visit for a regular check-up. The result of NCS showed aggravation in right ulnar nerve despite of marked improvement in other nerves (Table 1).
During follow-up, a few minor attacks affecting radial and facial nerves were noticed. Each episode was well controlled by PE scheduled as previous.
The patient had all the typical features of chronic relapsing LSS in clinical and electrophysiological aspects; 1) initial neurologic deficits, both motor and sensory, started in upper extremities, and each of sequential attack was comparable to a mononeuropathy multiplex, 2) electrophysiological findings also reflected a pattern of mononeuropathy multiplex throughout the studies, 3) persisitent multifocal conduction blocks, temporal dispersion and marked slowing of NCVs along the affected nerves further revealed that it is a form of demyelinating neuropathy, and 4) normal CSF protein level and titers of antibodies directed against myelin components (e.g. GM1 ganglioside).
Nerve pathology is highlighted with marked loss of myelinated nerve fibers and interfascicular variation of the lesions, which have been reported as a hallmark of LSS (6, 8). Although marked interfascicular variation is more frequently observed with ischemic process, nerve pathology from our patient was evidenced neither on vasculitis nor perivascular inflammation. As the affection of right superficial peroneal nerve occurred only before nerve biopsy, it was unlikely that the nerve pathology was influenced by prior uses of steroid. Furthermore, nerve fiber hypertrophy and onion bulb formations as demonstrated in semithin sections might be another evidence of the repeated demyelination-remyelination process. Taken above findings altogether, what can be said for underlying pathology of the disease is - a demyelinating mononeuropathy multiplex.
Isolated abducens palsy, which was occurred as fifth episode and immediately resolved by PE, can also be a characteristic feature of LSS in our case. Actually, cranial nerve involvement is not uncommon in LSS and has been observed in 17-31% of patients from various reports. Whereas cranial nerves II, III, IV, V, VII, IX, and X have been described to be often involved (4, 5), abducens palsy has never been reported anywhere. Thus, we could here add abducens nerve to the list of cranial nerves which can be affected in LSS.
To date, IVIg and/or corticosteroid are considered as a standard therapy for LSS. According to the literatures, therapeutic response rates ranged from 50 to 67% with IVIg and 25 to 79% with corticosteroid, and only remaining 10 to 20% of the patients are non-responders (8, 9). Recent study based on a large cohort also reported overall 73% of response rate to immune-mediated therapies including IVIg, steroid and azathioprine. Therefore, our patient was expected to show an improvement with these drugs. However, the patient was totally refractory to all the standard treatment as discussed before; rather, a part of preceding symptoms were gradually worsened, and several times of sequential attacks involving different nerves were followed. Final improvement has come only after a course of PE, and which was quite dramatic; left abducens palsy has immediately resolved, and motor and sensory deficits were subsequently recovered.
Most of the reports concerning LSS therapies recommend either IVIg or steroid as a first-line therapy, and switching one from the other in non-responders to either of them. Meanwhile, PE was rarely tried in LSS, if any, it was mostly ineffective and even led to an acute exacerbation during or after the treatment (8). Many physicians feel reluctant to use PE as a first-line therapy when the expected result of PE is not much different compared with other immune therapies, due to a requirement of closer medical attentions and a major vascular access. In addition, use of PE as a main therapy is limited since PE is only adjunctive and its effect is not permanent, thereby making patients to be dependent on the treatment (10). Nevertheless, this case clearly represents that PE can draw excellent outcome in a refractory case to IVIg and steroid. It further means that PE can rescue significant population of the patients with LSS, who otherwise may fall into a group of non-responders. Thus, our report strongly proposes that PE should be considered as an alternative therapeutic option in LSS, and physicians may be encouraged to try PE, particularly because LSS is among few treatable neuropathies.
Figures and Tables
Fig. 2
The first nerve conduction study in right median and left ulnar nerves show conduction blocks and temporal dispersion with mild slowing of nerve conduction velocities.

Fig. 3
Pathological findings of right superficial peroneal nerve. (A) A profound loss of myelinated fibers is seen in one fascicle, while they are relatively spared in others (modified Gomori-Trichome, ×40). (B) On semithin sections, marked nerve fiber hypertrophy with onion bulb formations is suggested (toluidine blue, ×400).

References
1. Lewis RA, Sumner AJ, Brown MJ, Asbury AK. Multifocal demyelinating neuropathy with persistent conduction block. Neurology. 1982. 32:958–964.

2. Gorson KC, Ropper AH, Weinberg DH. Upper limb predominant, multifocal chronic inflammatory demyelinating polyneuropathy. Muscle Nerve. 1999. 22:758–765.

3. Oh SJ, Claussen GC, Kim DS. Motor and sensory demyelinating mononeuropathy multiplex (multifocal motor and sensory demyelinating neuropathy): a separate entity or a variant of chronic inflammatory demyelinating polyneuropathy? J Peripher Nerv Syst. 1997. 2:362–369.
4. Saperstein DS, Amato AA, Wolfe GI, Katz JS, Nations SP, Jackson CE, Bryan WW, Burns DK, Barohn RJ. Multifocal acquired demyelinating sensory and motor neuropathy: the Lewis-Sumner syndrome. Muscle Nerve. 1999. 22:560–566.

5. Van den Berg-Vos RM, Van den Berg LH, Franssen H, Vermeulen M, Witkamp TD, Jansen GH, van Es HW, Kerkhoff H, Wokke JH. Multifocal inflammatory demyelinating neuropathy: a distinct clinical entity? Neurology. 2000. 54:26–32.

6. Oh SJ, LaGanke C, Powers R, Wolfe GI, Quinton RA, Burns DK. Multifocal motor sensory demyelinating neuropathy: inflammatory demyelinating polyradiculoneuropathy. Neurology. 2005. 65:1639–1642.

7. Finsterer J. Treatment of immune-mediated, dysimmune neuropathies. Acta Neurol Scand. 2005. 112:115–125.

8. Verschueren A, Azulay JP, Attarian S, Boucraut J, Pellissier JF, Pouget J. Lewis-Sumner syndrome and multifocal motor neuropathy. Muscle Nerve. 2005. 31:88–94.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download