Abstract
Complement 1 (C1) inhibitor is an acute phase protein with anti-inflammatory properties. The aim of the present study was to elucidate the relationship between brachial ankle pulse wave velocity (baPWV), the parameter of arterial stiffness, and C1 inhibitor. One hundred subjects were randomly enrolled in this study. Data about baPWV, age, gender, hypertension, smoking, and body mass index (BMI) were measured. Blood tests for total cholesterol, low density lipoprotein, high density lipoprotein, triglycerides, hemoglobin A1c, erythrocyte sedimentation rate, C-reactive protein, complement 3, and C1 inhibitor were performed. Based on the Pearson correlation, the C1 inhibitor showed a positive relation to the baPWV (P<0.001). Multiple regression analysis revealed the significant predictors of baPWV were not only the conventional risk factors of arteriosclerosis and/or atherosclerosis, such as age (P<0.001), gender (P<0.001), hypertension (P<0.001), and BMI (P=0.006), but also the acute phase protein, C1 inhibitor (P=0.025). In conclusion, C1 inhibitor is associated with arterial stiffness through its association with increased inflammation.
The complement system is a biochemical cascade which helps clear pathogens from a host organism. However, the complement system also has the potential to be extremely detrimental to host tissues, meaning its activation must be tightly regulated to prevent developing inflammatory reactions (1). Complement 1 (C1) inhibitor is a naturally occurring serine proteinase inhibitor that inhibits activated serine proteinases, C1s and C1r, from the classical pathway of complement, and is a main inhibitor of activated factor FXII from the contact system, and also is an inhibitor of kallikrein and activated factor XI (2). Furthermore, C1 inhibitor is an acute phase protein, the plasma level of which may increase 2- to 2.5-fold during an inflammatory condition, such as an infection or rheumatoid arthritis (3, 4). Arteriolosclerosis or arterial stiffness is any hardening of arteries due to loss of elasticity. On the other hand, atherosclerosis is an inflammatory disease of the artery and shows hardening of artery specifically due to an atheromatous plaque (5-8). Atherosclerosis is the most common form of arteriosclerosis, thus the risk factors of both are similar (6, 7). Recently it has been reported that arterial stiffness is strongly associated with atherosclerosis and accelerated by risk factors such as aging, hypertension, diabetes, and renal insufficiency (6, 7, 9). The non-invasive test for arterial stiffness, brachial ankle pulse wave velocity (baPWV), is used in large scale populations and has become available in clinical settings (10). As arterial stiffness is closely related to atherosclerosis, an inflammatory disease of arterial wall (9, 11), we postulated that if the arterial stiffness is progressing, the inflammation of the arterial wall will correspondingly deteriorate. Thus, we hypothesize that if baPWV increases, the serum level of the acute phase protein, C1 inhibitor, may also rise to counteract the inflammation. To investigate this hypothesis, we measured baPWV and C1 inhibitor. At the same time, to evaluate the clinical relevance of baPWV, we also measured the conventional risk factors of arteriosclerosis and/or atherosclerosis (6-8, 12), such as age, gender, hypertension, smoking, body mass index (BMI), total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), triglycerides (TG), hemoglobin A1c (HbA1c), and the parameters of inflammation (erythrocyte sedimentation rate [ESR], C-reactive protein [CRP], and C3).
One hundred consecutive subjects, 18-77 yr of age, from the Department of Surgery of our hospital were enrolled in this study between June and December 2008, and analyzed cross-sectionally at the end of the study. All the subjects were enrolled voluntarily and randomly without any inclusion or exclusion criteria, however all the patients had surgical diseases such as varicose vein, hemorrhoid, and inguinal hernia (Table 1). A total of 40.5% of male (17/42) and 20.7% of female (12/58) patients had hypertension. They had calcium channel blocker (14 patients), angiotensin-2 receptor inhibitor (10 patients), beta blocker (4 patients), and diuretics (1 patient). A total of 19% of male (8/42) and 13.8% of female (8/58) patients had diabetes, and all of them administered oral hypoglycemic agents. Two patients with hypercholesterolemia had HMG CoA reductase inhibitor. In this study, hypertension was defined as a systolic blood pressure ≥140 mmHg and a diastolic pressure ≥90 mmHg, or for the subject who was taking antihypertensive medications, regardless of the current pressure. Smokers included the subjects who were smoking at the time of the measurement and ex-smokers. BMI was calculated as the body weight in kilograms divided by the height in meters squared. Informed consent was obtained from all the subjects. This study was approved by the Institutional Review Board of Masan Samsung Hospital of Sungkyunkwan University School of Medicine in Masan, Korea.
Blood samples were obtained from an antecubital vein in the morning after 12 hr of overnight fasting. An automatic analyzer (Modular System; Roche, Mannheim, Germany) was used to measure total cholesterol, LDL, HDL, and TG. HbA1c was measured by an automatic machine (HLC723-G7; TOSOH, Tokyo, Japan). CRP and C3 were analyzed by an automatic analyzer (COBAS Integra 800; Roche, Rotkreuz, Swiss). C1 inhibitor was measured using a kit (C1 inactivator; RID, San Diego, CA, U.S.A.). ESR was measured manually with the Wintrobe tube method (Espette, Kormed, Seoul, Korea).
The baPWV was measured by a volume plethysmographic apparatus (Vasoguard, model P84; Nicolet Vascular, Golden, CO, U.S.A.). For the assessment of inter-observer reliability (reproducibility) and intra-observer reliability (repeatability), 10 volunteers (5 males and 5 females; 26-67 yr of age range; mean age, 45 yr; 95% CI, 34-56 yr) were measured consecutively by 3 observers (technicians of the vascular laboratory) with 10 min intervals. Cuffs were rewrapped at every measurement. The same measurements were repeated the next day; hence there were a total of 60 measurements. All the measurements were performed in the morning after overnight fasting. To obtain the reproducibility and repeatability of measuring baPWV by Vasoguard, the intraclass correlation coefficient (ICC) was calculated using the data of the right baPWV of the volunteers.
In this study, 100 subjects were examined for baPWV in the morning after 10 min of rest in a temperature-controlled warm room (24±1℃). They did not take any medications on the day of the examination. Measurements were performed in the supine position. Waveforms were obtained from volume plethysmographic sensors in cuffs on the right brachium and both ankles. The time intervals (ΔTba) between the wave at the right brachium and at both ankles were recorded automatically by the machine. The distance between the sampling points of baPWV was calculated using the following equations: the length from the suprasternal notch to the right brachium (Lb)=0.2195×height (cm)-2.0734, and the length from the suprasternal notch to the ankle (La)=0.8129×height (cm)+12.328. The baPWV=(La-Lb)/ΔTba (10). The average values of the right and left baPWVs were used in the statistical analysis.
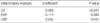
Intraclass correlation coefficient (ICC) was calculated by SAS (version 9.1; SAS Institute Inc., Cary, NC, U.S.A.). ICC values <0.4 represent poor reliability, and ICC values between 0.4 and 0.75 indicate fair-to-good reliability, whereas an ICC value >0.75 represents excellent reliability (13). The relation between C1 inhibitor and other inflammatory markers was tested by Spearman Correlation. The age distribution was tested by the Kolmogorov-Smirnov test of normality. The differences between males and females were compared by an independent sample t-test and the chi-square test. The univariate analysis between baPWV and age, BMI, total cholesterol, LDL, HDL, TG, HbA1c, C1 inhibitor, C3, ESR, and CRP was performed by Pearson and Spearman Correlation depending on the distribution patterns of the variables. Using the independent sample t-test, the differences of baPWV were measured as a function of gender, smoking, and hypertension. Multiple regression analysis using the stepwise method was performed to identify the predictors of baPWV. The independent variables included in the multiple regression analysis were age, gender, hypertension, BMI, total cholesterol, TG, HbA1c, C3, ESR, CRP, and C1 inhibitor. LDL, HDL cholesterol, and smoking were not included in the multiple regression analysis, because LDL and HDL cholesterol showed multicollinearity with total cholesterol (VIF 13.84, 3.40, and 15.19 respectively), and there were marked difference in smoking rate between males (80.9%, 34/42) and females (1.7%, 1/58). Statistical analysis was done using SPSS (version 11.5; SPSS Inc., Chicago, IL, U.S.A.). P values <0.05 were considered statistically significant.
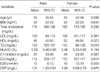
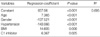
Inter-observer and intra-observer reliability, calculated by the ICC were 0.8783 and 0.8927, respectively, thus indicating that measuring baPWV with the Vasoguard machine has excellent reproducibility and repeatability (Fig. 1). The normality assumption for the distribution of age for 100 subjects and for males and females were not rejected by Kolmogorov-Smirnov test (P value=0.200, 0.110, and 0.200, respectively). The mean and 95% confidence interval of age for 100 subjects were 47.81 and 44.92-50.70 yr, and its values ranged from 18 to 77. There was no age difference between the males and females (Table 2); however, the smoking habit (male 80.9% vs. female 1.7%) and hypertension rate (male 40.5% vs. female 20.7%) were higher in males than females (P value <0.001 and 0.044, respectively by chi-square test). Fig. 2 depicts that baPWVs increase in proportion to the advancing age in both males and females. In Table 3, male gender, smokers, and hypertensive subjects had higher baPWVs than females, non-smokers, and non-hypertensive subjects. The univariate analysis indicated that baPWV had a positive correlation with age, BMI, TG, HbA1c, C1 inhibitor, C3, and CRP; however, HDL had a negative correlation (Table 4). The multiple regression analysis (stepwise method) showed not only the conventional risk factors of arteriosclerosis and/or atherosclerosis, such as age, gender, hypertension, and BMI but also the acute phase protein, C1 inhibitor, was a significant predictor of baPWV (Table 5, Fig. 3). C1 inhibitor revealed positive correlation with other inflammatory markers, C3 and CRP (Table 6).
In the current study, baPWV had a significant association with the conventional risk factors of arteriosclerosis and/or atherosclerosis, such as age, gender, hypertension, and BMI in both univariate and multivariate studies. This means that baPWV is a clinically relevant method to evaluate the arteries, and this result is compatible with the other studies on the relation between baPWV and risk factors (6, 7, 10, 14, 15). According to our hypothesis, we measured the relatively novel inflammatory marker, C1 inhibitor. In the result, the serum level of C1 inhibitor was positively related to baPWV, and C1 inhibitor was one of the significant predictors of baPWV. The serine proteinase inhibitor, C1 inhibitor, is synthesized and secreted from the several cell types, including hepatocytes, mononuclear phagocytes, fibroblasts, and umbilical vein endothelial cells (16-18). The major function of the C1 inhibitor is inhibition of the complement system to prevent spontaneous activation, in which the amount of C1 inhibitor in the serum is crucial. A minimal C1 inhibitor concentration of approximately 5.5 mg/dL (22% of the normal human serum level) is required to control C1-autoactivation (19). Originally, C1 inhibitor was shown to be associated with angioedema, and its deficiency was identified as the cause of hereditary angioedema (20, 21). However, C1 inhibitor belongs to a group of acute phase proteins, and its production and release increase during inflammation (3, 4). In our study, C1 inhibitor revealed positive correlation with C3 and CRP, thus indicating that C1 inhibitor was a member of acute phase proteins. Recently, it has been suggested that all the risk factors of atherosclerosis contribute to the development of atherosclerosis by aggravating the underlying inflammatory process (5, 8, 9, 11, 22-25). Although the exact mechanism is unknown, it has been reported that the inflammatory cytokine, interferon-gamma (IFN-gamma) is highly expressed in atherosclerotic lesions (26), moreover, IFN-gamma also enhances the expression of C1 inhibitor mRNA, primarily due to an enhanced transcription rate (27). Other cytokines, such as tumor necrosis factor alpha, interferon-alpha, monocyte colony stimulating factor, and interleukin-6 were also identified to stimulate the synthesis of C1 inhibitor (2). Determination of baPWV involves a simple and non-invasive method, and its validity, reproducibility, and clinical significance have been evaluated and confirmed in a previous study (10). In this study, we also demonstrated that the reproducibility and repeatability of measuring baPWV with Vasoguard equipment is reliable. In recent years, baPWV has been used more widely in assessing arterial stiffness, and has become available in a clinical setting as a simple predictor of the prognosis of patients (9, 14, 15, 28-30). In current study, we measured baPWV as a parameter of arterial stiffness and C1 inhibitor as a counteracting anti-inflammatory substance. Our result showed that baPWV had positive relation with C1 inhibitor; the higher the baPWV, the greater the serum level of C1 inhibitor. In summary, C1 inhibitor was positively related to baPWV, and was one of the significant predictors of baPWV. The present study suggests that C1 inhibitor is associated with arterial stiffness through its association with increased inflammation.
Figures and Tables
Fig. 1
Inter-observer and intra-observer reliability of measurements of the brachial ankle pulse wave velocity (cm/sec). (A) Inter-observer reliability (reproducibility) depicts the relationship between three independent measurements by three observers, r1 (observer 1), r2 (observer 2), and r3 (observer 3). The ICC value is 0.8783. (B) Intra-observer reliability (repeatability) shows the relationship between two different measurements by one observer. The ICC value is 0.8927.

Fig. 2
Linear regression graphs between baPWV and age in both males and females. (A) male, (B) female, baPWVs increase in proportion to the age in both males and females.

Fig. 3
Linear regression graph between baPWV and C1 inhibitor. Brachial ankle pulse wave velocity showed positive relationship to the serum level of C1 inhibitor. baPWV increases according to the increasing serum level of C1 inhibitor.
Table 3
Comparison of brachial ankle pulse wave velocity as a function of gender, smoking, and hypertension

Table 4
Univariate analysis between brachial ankle pulse wave velocity and the variables

*Pearson correlation (Variables have normal distribution.); †Spearman correlation (Variables do not have normal distribution.); P<0.05 is significant. BMI, body mass index; LDL, low density lipoprotein; HDL, high density lipoprotein; TG, triglycerides; HbA1c, hemoglobin A1c; C1, complement 1; C3, complement 3; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein.
References
1. Zanker KS. General introduction to innate immunity: Dr. Jekyl/Mr. Hyde quality of the innate immune system. Contrib Microbiol. 2008. 15:12–20.
2. Caliezi C, Wuillemin WA, Zeerleder S, Redondo M, Eisele B, Hack CE. C1-Esterase inhibitor: an anti-inflammatory agent and its potential use in the treatment of diseases other than hereditary angioedema. Pharmacol Rev. 2000. 52:91–112.
3. Kalter ES, Daha MR, ten Cate JW, Verhoef J, Bouma BN. Activation and inhibition of Hageman factor-dependent pathways and the complement system in uncomplicated bacteremia or bacterial shock. J Infect Dis. 1985. 151:1019–1027.

4. Woo P, Lachmann PJ, Harrison RA, Amos N, Cooper C, Rosen FS. Simultaneous turnover of normal and dysfunctional C1 inhibitor as a probe of in vivo activation of C1 and contact activatable proteases. Clin Exp Immunol. 1985. 61:1–8.
5. Kostner KM, Fahti RB, Case C, Hobson P, Tate J, Marwick TH. Inflammation, complement activation and endothelial function in stable and unstable coronary artery disease. Clin Chim Acta. 2006. 365:129–134.

7. Wykretowicz A, Gerstenberger P, Guzik P, Milewska A, Krauze T, Adamska K, Rutkowska A, Wysocki H. Arterial stiffness in relation to subclinical atherosclerosis. Eur J Clin Invest. 2009. 39:11–16.

8. Ridker PM, Silvertown JD. Inflammation, C-reactive protein, and atherothrombosis. J Periodontol. 2008. 79(8):Suppl. 1544–1551.

9. van Popele NM, Grobbee DE, Bots ML, Asmar R, Topouchian J, Reneman RS, Hoeks AP, van der Kuip DA, Hofman A, Witteman JC. Association between arterial stiffness and atherosclerosis: the Rotterdam Study. Stroke. 2001. 32:454–460.
10. Yamashina A, Tomiyama H, Takeda K, Tsuda H, Arai T, Hirose K, Koji Y, Hori S, Yamamoto Y. Validity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurement. Hypertens Res. 2002. 25:359–364.

11. Nicoletti A, Caligiuri G, Hansson GK. Immunomodulation of atherosclerosis: myth and reality. J Intern Med. 2000. 247:397–405.

12. Kullo IJ, Gau GT, Tajik AJ. Novel risk factors for atherosclerosis. Mayo Clin Proc. 2000. 75:369–380.

13. Rosner B. Fundamentals of Biostatistics. 1995. 4th ed. Belmont, California, USA: Duxbury Press.
14. Kim DH, Kim J, Kim JM, Lee AY. Increased brachial-ankle pulse wave velocity is independently associated with risk of cerebral ischemic small vessel disease in elderly hypertensive patients. Clin Neurol Neurosurg. 2008. 110:599–604.

15. Xu Y, Wu Y, Li J, Ma W, Guo X, Luo Y, Hu D. The predictive value of brachial-ankle pulse wave velocity in coronary atherosclerosis and peripheral artery diseases in urban Chinese patients. Hypertens Res. 2008. 31:1079–1085.

16. Lappin D, Whaley K. Regulation of C1-inhibitor synthesis by interferons and other agents. Behring Inst Mitt. 1989. (84):180–192.
17. Zuraw BL, Lotz M. Regulation of the hepatic synthesis of C1 inhibitor by the hepatocyte stimulating factors interleukin 6 and interferon gamma. J Biol Chem. 1990. 265:12664–12670.

18. Prada AE, Zahedi K, Davis AE 3rd. Regulation of C1 inhibitor synthesis. Immunobiology. 1998. 199:377–388.

19. Windfuhr JP, Alsenz J, Loos M. The critical concentration of C1-esterase inhibitor (C1-INH) in human serum preventing auto-activation of the first component of complement (C1). Mol Immunol. 2005. 42:657–663.

20. Johnson AM, Alper CA, Rosen FS, Craig JM. C1 inhibitor: evidence for decreased hepatic synthesis in hereditary angioneurotic edema. Science. 1971. 173:553–554.

21. Donaldson VH, Rosen FS. Action of complement in hereditary angioneurotic edema: the role of C'1-esterase. J Clin Invest. 1964. 43:2204–2213.
22. Natali A, L'Abbate A, Ferrannini E. Erythrocyte sedimentation rate, coronary atherosclerosis, and cardiac mortality. Eur Heart J. 2003. 24:639–648.

23. Buono C, Come CE, Witztum JL, Maguire GF, Connelly PW, Carroll M, Lichtman AH. Influence of C3 deficiency on atherosclerosis. Circulation. 2002. 105:3025–3031.

24. Mallika V, Goswami B, Rajappa M. Atherosclerosis pathophysiology and the role of novel risk factors: a clinicobiochemical perspective. Angiology. 2007. 58:513–522.

25. Bisoendial RJ, Kastelein JJ, Stroes ES. C-reactive protein and atherogenesis: from fatty streak to clinical event. Atherosclerosis. 2007. 195:e10–e18.

26. McLaren JE, Ramji DP. Interferon gamma: a master regulator of atherosclerosis. Cytokine Growth Factor Rev. 2009. 20:125–135.

27. Zahedi K, Prada AE, Davis AE 3rd. Transcriptional regulation of the C1 inhibitor gene by gamma-interferon. J Biol Chem. 1994. 269:9669–9674.

28. Tomiyama H, Koji Y, Yambe M, Shiina K, Motobe K, Yamada J, Shido N, Tanaka N, Chikamori T, Yamashina A. Brachial--ankle pulse wave velocity is a simple and independent predictor of prognosis in patients with acute coronary syndrome. Circ J. 2005. 69:815–822.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download