Abstract
We report a rare case of giant mesenteric lipoma presenting with colicky abdominal pain. A 29-yr-old woman underwent laparoscopic resection for a giant mesenteric lipoma causing compression of the ileal loop. The resected ileal segment was encased by a giant fatty tissue, and normal mucosal fold patterns of the resected ileum were effaced by the mass. Microscopically, the mass was characterized by homogenous mature adipose tissue without cellular atypia, which was compatible with the diagnosis of a mesenteric lipoma. Despite the benign nature of this tumor, total excision with or without the affected intestinal loop should be considered if intestinal symptoms such as abdominal pain are present.
Solitary or multiple lipomas can occur almost anywhere in the trunk, extremities, mediastinum, pelvis, and retroperitoneum, but they rarely originate in the intestinal mesentery (1-4). A search of the English literature has revealed less than 30 documented cases. In the literature review, mesenteric lipomas do not cause any intestinal symptoms in most cases as they usually allow the passage of intestinal contents (1, 5), and those causing abdominal pain make up only a small percentage (2, 6). Mesenteric lipomas may cause abdominal pain by complete intestinal obstruction as a result of torsion or volvulus (3, 7-9) or partial intestinal obstruction associated with compression of the intestine.
In the present report, we describe a case of a giant mesenteric lipoma causing abdominal pain by entrapment of an ileal loop and review the cases with mesenteric lipomas causing abdominal pain.
A 29-yr-old woman presented with colicky lower abdominal pain. Her abdominal pain had developed 3 yr before intermittently, but it had worsened over the past 6 months. She was unable to sleep well due to her abdominal pain, which aggravated after eating meals. She also experienced episodes of abdominal distension, constipation, and urinary frequency or urgency. Other symptoms, as well as her past medical history and family history, were otherwise unremarkable.
The patient had a height of 164 cm and weight of 59.6 kg, for a body mass index of 22.2. Physical examination revealed a slightly distended abdomen, but the remainder of the examination was unremarkable. Routine blood tests, including renal function and urine analysis, were normal.
Computed tomography (CT) of the abdomen and pelvis revealed a homogenous fatty mass in the lower abdominal cavity (Fig. 1). The entire small bowel loop was displaced upward by the mass, and one segment of the ileal loop was slightly straightened by entrapment of the bowel. Small bowel series revealed ileal loop entrapped in fatty tissue and associated ileal diverticula (Fig. 2).
Laparoscopic surgical resection was recommended because of her symptoms. The laparoscopic surgery showed an encapsulated, yellowish mass originating from the ileal mesentery in the lower abdominal cavity. The mass extended to the antimesenteric border of the small bowel and was free of any adhesions or signs of necrosis. Some segment of the ileum appeared to be "stretched" over the fatty mesenteric mass with edema, however, its luminal patency was preserved in spite of luminal narrowing by compression. Lymphadenopathy or fluid collection was not observed. Surgical removal of the fatty mass and the affected ileal loop was performed without difficulty under a laparoscopic magnified view. The resected mesenteric mass was a soft, yellow mass and 19×10×5.1 cm in size (Fig. 3). Microscopically, the mass was characterized by homogenous mature adipose tissue without cellular atypia, which was compatible with the diagnosis of a mesenteric lipoma (Fig. 4). Any evidence of necrosis or malignancy was not observed.
She had no postoperative complications and was free of any signs of disease recurrence 15 months after the operation.
The exact prevalence of lipomas is unknown, however, it is likely far higher than reported because most cases with lipomas may be ignored due to their silent nature. Lipomas may show a familial tendency and an increased incidence in people who are obese, have diabetes mellitus or hypercholesterolemia, and experience a traumatic injury (4); however, none of these factors were applicable to our patient. Although benign lipomas can arise in any location in which fat is normally present, reported mesenteric lipomas have been very rare (1-9). They generally form as a slow-growing, non-lobulated, soft, mobile mass that does not penetrate into surrounding organs (1, 4). Although many lipomas are an incidental finding, they may cause variable symptoms when the tumor grows very large. Their uncommon symptoms include anorexia, abdominal distension, weight loss, abdominal pain, constipation, and sensation of fullness, especially after meals, as our case. When the tumor is near the intestinal lumen and far from the mesenteric root, it may cause abdominal pain by pressing upon the intestinal loops, however, passage of the intestinal contents may be allowed as our case due to the consistency of the lipoma and liquid nature of small intestinal contents (4). Our patient, who suffered from chronic intermittent abdominal pain and constipation, has been examined at the primary clinic several times during the last 3 yr without receiving a definite diagnosis. Even though pelvic ultrasonographic examination was performed by primary physician, it was misdiagnosed as mesenteric fat. Mesenteric lipomas may pose diagnostic difficulties due to absence of abnormal laboratory findings and its vague non-specific symptoms as our case. Therefore, physicians should be aware of the various manifestations of mesenteric lipomas and avoid inappropriate managements.
We reviewed reports of mesenteric lipomas identified using a computerized search of Pubmed (articles in English between 1965 and 2007), and thirteen cases of which causing abdominal pain (Table 1). The incidence of this tumor is equal for both sexes, and seven of the cases have been reported in children (2, 8, 11-13, 15). All tumors are located in the mesentery of the small intestine, mostly the ileum, as our case. The main sequelae of mesenteric lipoma are complete intestinal obstruction as a result of torsion or volvulus (3, 7, 9-13) or partial intestinal obstruction due to compression of intestine by giant lipomas (2, 8, 14-16). Abdominal pain may also be related to altered peristalsis secondary to adhered small bowel loops. In terms of size, mesenteric lipomas have a tendency to produce symptoms dependent on their size. The size of the mesenteric lipoma in our patient was one of the largest reported in the literature.
Generally, the size of mesenteric lipomas with obstruction by compression of intestinal loop (mean=21 cm) was larger than those of mesenteric lipomas with obstruction caused by torsion or volvulus (mean=13 cm).
Radiological examination suggests the possible diagnosis, and the best definitive diagnostic procedure is CT, which demonstrates a proliferation of homogenous adipose tissue in the lower abdominal cavity (18, 19). The CT number reading provides information about the nature of the lesion, and the density of the fatty mass with attenuation values between -80 and -120 HU, which is identical to that of subcutaneous fat, may lead to its diagnosis (19). When a large mesenteric lipoma extends lower in the abdominal or even pelvic cavity due to its gravity as our case, CT findings of mesenteric lipoma may mimic pelvic lipomatosis, which is a rare condition defined as a nonmalignant overgrowth of normal fat in the perivesical and perirectal spaces (20-22). Ultrasound can detect mesenteric lipoma as a homogenous echogenic mass (7), however, it may be misdiagnosed as mesenteric fat as our case because the mesentery is rich in fat. Therefore, primary physicians should keep in mind the possibility of this rare disease when faced with the prominent fatty tissue in the abdominal cavity during ultrasonographic examination.
Definitive treatment for mesenteric lipoma has not been established. Entire resection with, or if possible without, the affected intestinal loop may be the treatment of choice for the large mesenteric lipomas due to the risk of partial or complete intestinal obstruction by compression or volvulus. As reported by Tsushimi et al. (23), laparoscopic surgery has gained wide acceptance as the treatment of choice for benign tumors of the abdomen because it is less invasive than conventional open surgery and is economically, cosmetically, and physically beneficial. In addition, it may provide better surgical planes under magnified views than conventional laparotomy. In this regard, laparoscopic surgery may be favored for the removal of a large mesenteric lipoma despite limited experiences for this rare disease.
Mesenteric lipomas are rare, however, they may be considered in the differential diagnosis of unusual abdominal pain. Despite the benign nature of this tumor, total excision with or without the affected intestinal loop by laparoscopic approach may be considered if intestinal symptoms such as abdominal pain are present.
Figures and Tables
Fig. 1
Contrast-enhanced CT scan of a mesenteric lipoma. The coronal reformation image shows a prominent mass with homogenous fatty attenuation (arrows) in the lower abdominal cavity. A narrowing and elongation of an entrapped small bowel segment was observed (arrowheads).
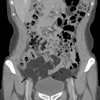
Fig. 2
A small bowel follow-through image shows upward deviation of the entire small bowel loop, except for one segment of the ileal loop (arrows) entrapped within the prominent fatty tissue. Note the diverticula in the entrapped ileal loop.
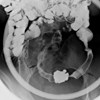
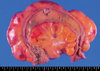
Fig. 3
Resected small bowel and mesenteric lipoma. The normal mucosal fold pattern of the resected small bowel lumen was effaced.
References
1. Prando A, Wallace S, Marins JL, Pereira RM, de Oliveira ER, Alvarenga M. Sonographic features of benign intraperitoneal lipomatous tumor in children: report of 4 cases. Pediatr Radiol. 1990. 20:571–574.
2. Kaniklides C, Frykberg T, Lundkvist K. Pediatric mesenteric lipoma; an unusual cause of repeated abdominal pain. A case report. Acta Radiol. 1998. 39:695–697.
3. Takagi Y, Yasuda K, Nakada T, Abe T, Saji S. Small bowel volvulus caused by a lipoma of the mesentery showing a distinct pattern on preoperative computed tomography. Dis Colon Rectum. 1998. 41:122–123.

4. Ilhan H, Tokar B, Işiksoy S, Koku N, Pasaoglu O. Giant mesenteric lipoma. J Pediatr Surg. 1999. 34:639–640.

5. Signer RD, Bregman D, Klausner S. Giant lipoma of the mesentery: report of an unusual case and review of the literature. Am Surg. 1976. 42:595–597.
6. Sato M, Ishida H, Konno K, Komatsuda T, Naganuma H, Segawa D, Watanabe S, Ishida J. Mesenteric lipoma: report of a case with emphasis on US findings. Eur Radiol. 2002. 12:793–795.

7. Sheen AJ, Drake I, George PP. A small bowel volvulus caused by a mesenteric lipoma: report of a case. Surg Today. 2003. 33:617–619.

8. Ozel SK, Apak S, Ozercan IH, Kazez A. Giant mesenteric lipoma as a rare cause of ileus in a child: report of a case. Surg Today. 2004. 34:470–472.

9. Wong HI, Chen CY, Liu GC. Primary mesenteric lipoma causing closed loop bowel obstruction: a case report. Kaohsiung J Med Sci. 2005. 21:138–141.

10. McCoubrey AS, Thompson RL. Small bowel volvulus secondary to a mesenteric lipoma: a case report and review of the literature. Ir J Med Sci. 2006. 175:79–80.

11. Kisra M, Ettayebi F, EI Azzouzi D, Benhammou M. Image of the month. Mesenteric lipoma. Arch Surg. 2006. 141:1046.
12. Cherian A, Singh SJ, Broderick N, Zaitoun AM, Kapila L. Small bowel volvulus due to giant mesenteric lipoma. Pediatr Surg Int. 2004. 20:869–871.

13. Wolko JD, Rosenfeld DL, Lazar MJ, Underberg-Davis SJ. Torsion of a giant mesenteric lipoma. Pediatr Radiol. 2003. 33:34–36.

14. Sherer DM, Lysikiewicz A, Chambers JT, Frager D, Eliakim R, Miodovnik M. Large mesenteric lipoma ultrasonographically mimicking a mature cystic teratoma during pregnancy. J Ultrasound Med. 2002. 21:473–476.

15. Gupta DK, Rohatgi M, Rao PS. Mesenteric lipoma. Indian Pediatr. 1988. 25:1007–1009.
16. Locker A. Giant lipoma of the mesentery. Br J Clin Pract. 1987. 41:977–978.
17. Livne PM, Zer M, Shmuter Z, Dintsman M. Acute intestinal obstruction caused by necrotic mesenteric lipoma-a case report. Am J Proctol Gastroenterol Colon Rectal Surg. 1981. 32:19–22.
18. Pereira JM, Sirlin CB, Pinto PS, Casola G. CT and MR imaging of extrahepatic fatty masses of the abdomen and pelvis: techniques, diagnosis, differential diagnosis, and pitfalls. Radiographics. 2005. 25:69–85.

19. Méndez-Uriburu L, Ahualli J, Méndez-Uriburu J, Méndez-Uriburu M, Fajre L, Méndez-Uriburu F, Carabajal R. CT appearances of intraabdominal and intrapelvic fatty lesions. AJR Am J Roentgenol. 2004. 183:933–943.

20. Fogg LB, Smyth JW. Pelvic lipomatosis: a condition simulating pelvic neoplasm. Radiology. 1968. 90:558–564.

21. Klein FA, Smith MJ, Kasenetz I. Pelvic lipomatosis: 35-year experience. J Urol. 1988. 139:998–1001.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download