Abstract
Complex regional pain syndrome (CRPS) is a chronically painful and disabling disorder. However, no data are available even on the epidemiology of CRPS in Korea. This study was undertaken to retrospectively assess the epidemiologic characteristics of CRPS in 150 consecutive patients at a tertiary chronic pain center from March 2002 to February 2006. Information was obtained regarding patients' demographics, nature of injury, and treatment modalities. Seventy-one percent of patients had CRPS type I. The mean 11-point verbal numerical rating scale score at initial examinations and at the time of study were 8.0 and 5.7, respectively. Thirty-two percent of patients showed no change or increase in pain intensity during follow-up at our pain center. The mean duration of CRPS symptoms prior to our pain center evaluation and prior to the time of study were 27 months and 50 months, respectively. These patients had seen on average 5 different physicians before being referred to our center. This study shows that the majority of CRPS patients were referred to our center after more than 2 yr of symptoms. The clinical implication of such delayed transfer and strategies to avoid this problem are discussed.
Complex regional pain syndrome (CRPS) is associated with topical pain, which develops primarily after trauma. The intensity and duration of CRPS are highly variable, though CRPS can induce serious impairment of the autonomic nervous system and of motor function, and consequently can result in diverse clinical outcomes.
The development of CRPS may be explained by various mechanisms, such as alterations in the central nervous system or by biofeedback from the sympathetic nervous system, but the underlying mechanism remains to be clarified. Although definite measures for the diagnosis and treatment of CRPS are being actively pursued (1, 2), as yet no objective diagnostic criterion nor a simple reliable test has been established. For this reason, it usually takes a long time to the final diagnosis of CRPS, which ultimately renders treatment outcomes worsened. Moreover, in Korea, not even epidemiological studies have been conducted as yet. Therefore, the aim of this study was to assess the epidemiologic characteristics of CRPS for the first time in Korean patients.
This retrospective study was approved by our institutional review board. The medical records of 150 consecutive patients diagnosed with CRPS at our pain center from March 2002 to February 2006 were reviewed and current patient status was determined using telephone interviews. At initial visits, all available prior medical data including neurological and radiological data were reviewed. Twenty-three patients were lost to follow-up and 7 had died, and thus, 120 patients were interviewed by telephone. Present pain intensity and the treatment modality regarded to be most helpful for alleviating pain were recorded. For each finding, patient percentages were calculated based on a responder basis rather than on total patient number.
Diagnoses were made in our pain center using the modified International Association of the Study of Pain (IASP) diagnostic criteria for CRPS (3). Many ancillary tests, such as, neuromuscular conduction, quantitative sensory, and autonomic function tests (including diagnostic sympathetic block), and infrared thermography and a 3-phase bone scan were usually performed at initial visits and during follow-up. Infrared thermographic results were interpreted as positive when the temperature difference between ipsilateral and contralateral extremities was ≥0.6℃ (4). Results of 3-phase bone scans were interpreted as positive when a difference in early blood pooling with or without an increase in diffuse bony uptake was observed (5).
The following details were available for analysis: patients' age, gender, type of CRPS, site of lesion, injury profile, pain intensities at presentation and at the time of study, duration of CRPS symptoms prior to our pain center evaluation and prior to the study, the number of physicians who had treated patients before referral to our center and their medical fields, the treatment modalities received, the treatment modality considered by patients to be most effective, and the presence of a history of spinal cord stimulation (SCS). Pain intensity was rated using an 11-point of verbal numerical rating scale (VNRS).
Data are presented as means±SD. Statistical analyses were performed using descriptive statistics.
Eighty-three patients (55%) were male and 67 (45%) were female (0.8: 1 female-to-male ratio). Patients' mean age at initial evaluations was 45±14 yr, and mean age at time of injury was 40±45 yr and 43±19 yr for male and female patients, respectively. CRPS developed most frequently in the third decade (22 patients) and in the fifth (22 patients) in men. The military personnel was 73% (16 patients) in the third decade. In female patients, CRPS developed most frequently in the fifth decade (18 patients), followed by the forth (16 patients) and sixth (13 patients) (Fig. 1). Seventy-one percent of patients had CRPS type.
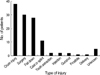
Mean VNRS scores at initial evaluations and by telephone interview were 8.0±1.9 and 5.7±2.5, respectively. Thirty-eight patients (32%) showed no change or increase in pain intensity during follow-up treatment. The mean durations of CRPS symptoms prior to our initial pain center evaluation and prior to the time of study were 27±52 months and 50±53 months, respectively, and 5±5 (range, 0-40) physicians were visited before referral to our center. Crush injury, surgery, and fall down trauma were common causes of CRPS (68 patients, 45%) (Fig. 2). Eighty-two percent of the patients complained of pain in one extremity only, and lower extremities (55%) were more commonly affected than upper extremities (27%). Eighteen percent complained of a pain in the face or chest. Seventy-five percent of patients had been treated by ≥1 anesthesiologist before being referred to our pain center.
The treatment modalities which were used at our pain center included physical therapy, pharmacotherapy, sympathetic blocks and/or chemical neurolysis, radiofrequency lesioning, intravenous infusion of ketamine or lidocaine, intravenous regional block, and spinal cord stimulation. Pharmacotherapy was the most common form of therapy (91 patients), followed by sympathetic block (42 patients), intravenous infusion of ketamine (36 patients), and/or nerve blocks (35 patients) (Fig. 3).
Seventy-six percent reported that sympathetic block or neurolysis including radiofrequency lesioning was the most effective treatment. Twenty-three percent of patients (24/108 patients) were implanted with a spinal cord stimulator (SCS). However, 38% (9/24) had their SCS removed during follow-up, but on the other hand, 21% (5/24) responded that they considered SCS stimulation the most effective treatment modality (Fig. 4). One patient received dorsal rhizotomy and a limb amputation, and 1 patient committed suicide.
Little published data are available on the epidemiology of CRPS, and this study is the first epidemiologic study of CRPS that was conducted in Korea. Overall, the epidemiologic data collected during this study are similar to those of previous studies (6, 7). However, our data showed a female-to-male ratio of 0.8:1, which does not concur with the findings of other studies, which have found that CRPS more commonly develops in women at gender ratios of 1:2.3-1:4.5 (6, 8, 9). In the present study, the condition occurred more often in male patients aged 20-29 yr than in other age groups. Obligatory military service in Korea may have increased the risk of trauma in this age group. The mean duration of CRPS symptoms prior to presentation at our pain center was 27 months, which is similar to that found by Allen et al. (6), but longer than that reported by Sandroni et al. (7). It is known that a prior injury, e.g., fractures, contusions, sprains, and surgical traumas, is the main cause of CRPS (6). The present study also shows that injuries such as traffic accidents and falls are leading causes of CRPS and that surgical trauma contributed to a lesser extent, which concurs with that reported elsewhere (6, 7). In addition, in the present study, immobilization due to a splint, gun shot wounds, tooth extractions, injections, and pregnancies were all found to induce CRPS.
We found that a lower limb was affected approximately twice as often as an upper limb, which concurs with the findings of Allen et al. (6). However, Sandroni et al.(7) reported that CRPS developed more frequently in an upper limb than in a lower limb. Moreover, in this study (7) bilateral side involvement was observed in some cases as an early manifestation. The over-expression of symptoms in relation to the reward may in part explain this phenomenon.
In the present study, the type I: type II ratio was 7:3, which differs from that reported by a previous study which indicated that the incidence of CRPS type II was extremely rare except during a war (10).
In the present study, pharmacotherapy was adopted most frequently, followed by a sympathetic nerve block, the intravenous infusion of ketamine, and a spinal nerve block. According to patients' subjective reports on treatment efficacy, a sympathetic block and the intravenous infusion of ketamine were the most effective treatment modalities among those treatment modalities received. Sympathetic nerve block has been reported to be only effective at treating sympathetic maintained pain, although it has been described as a first choice therapy (11). In addition, it has been reported that sympathetic nerve block is also effective at ameliorating elevated skin temperatures, edema, or allodynia that develops within 6 months (11). The present study revealed that intravenous ketamine (an NMDA receptor antagonist) was clinically effective in 44% of patients. Correll et al. (12) reported that 76% of patients with CRPS who did not respond to conventional treatment achieved complete remission after intravenous ketamine administration and that 18% achieved partial remission. Moreover, they found that the therapeutic effects of intravenous ketamine lasted between 3 and 12 months and that it could be reperformed in recurrente cases, although it was also found on occasions to induce headaches and hallucinations. SCS reduces the pain via neuromodulation. Taylor et al. (13) concluded that SCS is effective in 70% of CRPS patients and more cost-effective than conventional treatments. In our previous report (14), 57% of CRPS patients rated SCS as having an excellent or good effect. In this present study, 23% of patients underwent SCS implantation, but 62% of them have been used SCS at the time of study and only 20% of them was the most effective treatment modality they had encountered. Based on the present study, the possible reasons for the high removal rate and relatively low satisfaction with SCS were delayed diagnosis and treatment, high initial cost, higher dosage of opioids, high initial pain score, inaccurate evaluation of the effect of trial stimulation, and too high expectation of the benefits of SCS. After covering the cost of SCS by the National Health Insurance System in Korea on August 1 2005, the incidence of SCS implantation has increased year on year, and this might well increase future satisfaction rates.
At initial examinations, the mean VNRS score of patients was 8.0, which is similar to that reported previously (15). The mean VNRS score reduced to 5.8 after treatment, but 32% of patients showed no change or further symptom aggravation. Although a considerable number of patients with CRPS experience spontaneous remission (7), CRPS became an intractable chronic pain in one third of our cases, and some of these required dorsal rhizotomy or limb amputation. CRPS is more successfully treated when patients are early diagnosed and treated aggressively, as the risk of intractable chronic pain increases as the time between symptom onset and final diagnosis increases (16). In the present study, treatment outcomes were thought to be poorer than in a previous study (7) because the time between onset and final diagnosis of CRPS was longer. This poorer treatment outcome may also be attributed to the fact that patients in the present study had relatively severe pain and a long illness duration. Therefore, we advise that patients suspected of having CRPS be referred to specialists or specialty clinics to ensure early diagnosis and treatment.
This study had some limitations. First, it was intrinsically limited by its retrospective nature. Second, some cases were lost to follow-up and finally, the study subjects analyzed were treated at one university-based tertiary chronic pain center.
In conclusion, the present study describes the epidemiologic characteristics of CRPS patients for the first time in Korea. However, the information gained is limited in terms of its general applicability to all Korean CRPS patients. Thus, we recommend that a nationwide study be undertaken with a view toward documenting the epidemiologic characteristics of Korean CRPS patients as a means of facilitating early diagnosis and treatment.
Figures and Tables
References
2. Rho RH, Brewer RP, Lamer TJ, Wilson PR. Complex regional pain syndrome. Mayo Clin Proc. 2002. 77:174–180.

3. Bruehl S, Harden RN. Harden RN, Baron R, Janig W, editors. An empirical approach to modifying IASP diagnostic for CRPS. Complex regional pain syndrome. 2001. Seattle: IASP press;303–313.
4. Bruehl S, Lubenow TR, Nath H, Ivankovich O. Validation of thermography in the diagnosis of reflex sympathetic dystrophy. Clin J Pain. 1996. 12:316–325.

5. Park SH, Lee PB, Lim YH, Lee SY, Choi IY, Lee SJ, Oh YS. The usefulness of three-phase bone scan and thermography for making the diagnosis of CRPS-I. Korean J Pain. 2006. 19:81–86.

6. Allen G, Galer BS, Schwartz L. Epidemiology of complex regional pain syndrome: a retrospective chart review of 134 patients. Pain. 1999. 80:539–544.

7. Sandroni P, Benrud-Larson LM, McClelland RL, Low PA. Complex regional pain syndrome type I: incidence and prevalence in Olmsted county, a population-based study. Pain. 2003. 103:199–207.

8. Schwartzman RJ, Kerrigan J. The movement disorder of reflex sympathetic dystrophy. Neurology. 1990. 40:57–61.

9. Veldman PH, Reynen HM, Arntz IE, Goris RJ. Signs and symptoms of reflex sympathetic dystrophy: prospective study of 829 patients. Lancet. 1993. 342:1012–1016.

10. Hassantash SA, Afrakhteh M, Maier RV. Causalgia: a meta-analysis of the literature. Arch Surg. 2003. 138:1226–1231.
11. Galer BS, Schwartz L, Aller R. Loeser JD, Butler SH, Chapman CR, Turk DC, editors. Complex regional pain syndromestype I: reflex sympathetic dystrophy, and type II: causalgia. Bonica's Management of Pain. 2001. 3rd ed. Philadelphia: Lippincott Williams & Wilkins;404–408.
12. Correll GE, Maleki J, Gracely EJ, Muir JJ, Harbut RE. Subanesthetic ketamine infusion theraphy: a retrospective analysis of a novel therapeutic approach to complex regional pain syndrome. Pain Med. 2004. 5:263–275.
13. Taylor RS, Van Buyten JP, Buchser E. Spinal cord stimulation for complex regional pain syndrome: a systematic review of the clinical and cost-effectiveness literature and assessment of prognostic factors. Eur J Pain. 2006. 10:91–101.

14. Lee CJ, Kim YC, Shin JH, Yoo SY, Shin HY, Kim YH, Han SS, Joh JY, Lee EH, Lee SC, Park JH. Spinal Cord Stimulation in management of intractable chronic pain: a 5-year experience. Korean J Anesthesiol. 2006. 51:195–200.

15. Forouzanfar T, Weber WE, Kemler M, van Kleef M. What is a meaningful pain reduction in patients with complex regional pain syndrome type 1? Clin J Pain. 2003. 19:281–285.

16. Wakasugi B. Pain clinic shindan chiryou guide. 1994. Nilon Iji Shimosha;43–49.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download