Abstract
We examined the antiallodynic interaction between gabapentin and adenosine A1 receptor agonist, N6-(2-phenylisopropyl)-adenosine R-(-)isomer (R-PIA), in a rat model of nerve ligation injury. Rats were prepared with ligation of left L5-6 spinal nerves and intrathecal catheter implantation for drug administration. Mechanical allodynia was measured by applying von Frey filaments. Gabapentin and R-PIA were administered to obtain the dose-response curve and the 50% effective dose (ED50). Fractions of ED50s were administered concurrently to establish the ED50 of the drug combination. The drug interaction between gabapentin and R-PIA was analyzed using the isobolographic method. Adenosine A1 receptor antagonist was administered intrathecally to examine the reversal of the antiallodynic effect. Locomotor function changes were evaluated by rotarod testing. Intrathecal gabapentin and R-PIA and their combination produced a dose-dependent antagonism against mechanical allodynia without severe side effects. Intrathecal gabapentin synergistically enhanced the antiallodynic effect of R-PIA when coadministered. There were no significant changes in rotarod performance time, except gabapentin 300 μg. In the combination group, the maximal antiallodynic effect was reversed by A1 adenosine receptor antagonist. These results suggest that activation of adenosine A1 receptors at the spinal level is required for the synergistic interaction on the mechanical allodynia.
Peripheral nerve injury may result in mechanical allodynia, a condition of extreme cutaneous sensitivity to normally innocuous mechanical stimuli. Unilateral ligation of L5 and L6 spinal nerves produces some signs that seem representative of neuropathic pain (1). Signs of mechanical allodynia were most evident in the nerve ligation model among several experimental animal models (2). The spinal pharmacology at spinal nerve ligation-induced allodynia has been shown to be distinct from that associated with acute nociceptive input.
Adenosine is an endogenous purine compound functioning as an extracellular signaling molecule in the central and peripheral nervous systems (3). Adenosine is released locally at tissue sites in response to trauma, ischemia and interactions with specific receptors. There are many experimental data showing the role of adenosine in the modulation of nociceptive transmission at the spinal level (4, 5). Four types of adenosine receptors have been identified and cloned as A1, A2A, A2B, and A3 (3, 6). It is known that the antiallodynic effects are mediated through the activation of spinal A1 adenosine receptors and motor dysfunction effects are mediated through A2 adenosine receptors at the spinal level (7).
Gabapentin is a 3-alkylated analogue of gamma-amino butyric acid, which modulates α2δcalcium-channel subunits, a mechanism thought to be important in neuropathic pain (8). Gabapentin analgesia is unaffected by opioid antagonism, and repeated administration of gabapentin does not lead to analgesic tolerance (9). Preclinical studies suggest that additive interactions may occur between gabapentin and morphine (10, 11) and that opioid tolerance can be prevented by the use of gabapentin (12). However, mechanisms underlying analgesic effects of gabapentin are not fully understood.
The combination of mechanistically distinct analgesic agents may result in additivity or synergism and may improve efficacy at lower doses, with fewer side effects than with the use of one agent alone. This strategy has been advocated in cases of partial treatment response (13).
There is no study on the antiallodynic interaction of intrathecal gabapentin and A1 adenosine receptor agonist in the spinal nerve ligation rat model. Therefore, in the present study, we have investigated the intrathecal interaction of gabapentin and A1 adenosine receptor agonist, R-PIA (N6-[2-phenylisopropyl]-adenosine R-[-]isomer) on mechanical allodynia in nerve-ligated neuropathic pain rats. The effect of A1 adenosine receptor antagonist (DPCPX; 1,3-Dipropyl-8-cyclopentylxanthine) against the antiallodynic effect produced by combination of each drug was also examined.
This study was performed under a protocol approved by the Animal Use and Care Committee at ASAN Institute for Life Science. The experiments were conducted in male Sprague-Dawley rats (weight 160-180 g), which were housed individually in a temperature-controlled vivarium and allowed to acclimate for 3 days in a 12/12-hr, light/dark cycle. For creating the neuropathic rat model, a surgical procedure was performed (1). Under enflurane anesthesia, the left L5 and L6 spinal nerves were gently isolated and ligated tightly with 6-0 black silk distal to the dorsal root ganglion and proximal to the formation of the sciatic nerve. If the rats showed a withdrawal threshold of <4.0 g by postoperative day 7, these rats were defined as demonstrating mechanical allodynia. For spinal drug administration, the rats were chronically implanted with catheters as previously described (14). Intrathecal polyethylene catheter (PE-10, Becton Dickinson and Company, Sparks, MD, U.S.A.) was passed caudally from the cistern magna to the spinal cord level of lumbar enlargement. Proper location was confirmed by a temporary motor block of both hindlimbs after injection of 2% lidocaine 10 μL. Only animals with no evidence of neurologic deficit after the operation were studied. Mechanical allodynia develops within 1 week after nerve ligation surgery and it lasts for 6-8 weeks. All experiments were conducted 1 week after implantation of the intrathecal catheter. The animals were 8-10 weeks of age at the time of drug testing.
For intrathecal administration, the drugs were given by using a microinjection syringe over a 60-sec interval in a volume of 10 μL, followed by a 10 μL flush. The drugs given were blind to the experimenter. For the determination of the time to peak effect and the dose (ED50) estimated to produce 50% maximal possible effect (%MPE) for each drug, gabapentin (Sigma, St. Louis, MO, U.S.A.) and R-PIA (Sigma) were administered intrathecally. The doses of 3, 10, 30, 100, and 300 μg (n=9 per subgroup) were injected for gabapentin, and 0.03, 0.1, 0.3, 1, 3, and 10 μg (n=9 per subgroup) were injected for R-PIA, respectively. Fractions of ED50s (1/2, 1/4, 1/8, and 1/16; n=9 per subgroup) were administered intrathecally in an equal dose ratio to establish the ED50 of the drug combination. When the drug combinations were given, the intrathecal injections were concurrent because the times of the peak effect of intrathecal gabapentin and R-PIA coincided. Thereafter, the interaction between these two drugs was assessed isobolographically. For the evaluation of an antagonistic effect in each pretreatment group, DPCPX (Sigma) 10 μg (n=9) was administered intrathecally 15 min before injections of the combination of the two. For the control group, normal saline (n=9) was administered. The maximal reversal from the peak effect of the combination group for antagonist was assessed and compared with peak %MPE.
All drugs were dissolved in 0.9% sodium chloride solution. There was at least a 7-day interval between drug injections of successive experiments to minimize any possibility of tolerance development and to eliminate the residual effects of a drug. Each animal received a maximum of three injections.
Behavioral testing was performed during the day portion of the circadian rhythm. All behavioral tests were conducted at fixed times (10:00 am-1:00 pm) in a quiet room by the same person who was kept unapprised of both the injected solution and the dose used. To undertake these measurements of a mechanical threshold, the rats were placed in an individual plastic cage with a wire mesh bottom. After 20 min, mechanical threshold was measured by applying a series of 8 calibrated von Frey filaments (0.40, 0.70, 1.20, 2.00, 3.63, 5.50, 8.50, and 15.1 g; Stoelting Co., Wood Dale, IL, U.S.A.) to the midplantar surface of the hindpaw ipsilateral to the nerve injury until a positive sign for pain behavior was elicited. It was held for 6 sec. A brisk withdrawal or paw flinching was considered as positive responses, in which case the next filament tested was the next lower force. In the absence of such response, the next filament tested was the next greater force. In the absence of a response at 15 g of pressure, the animals were assigned to this cutoff value. The mechanical stimulus producing a 50% likelihood of withdrawal was determined by using the up-down method (15).
Measurements were taken before and 15, 30, 45, 60, 90, 120, and 180 min after an intrathecal dose of the drug(s). Baseline threshold value for each animal at each drug trial was determined by checking responses to von Frey filaments on the same day just before drug injection. Locomotor function changes in the neuropathic rats were evaluated by rotarod testing (Acceler rota-rod for rats 7750; Ugo Basile, Comerio-Varese, Italy). Neuropathic rats were acclimated to revolving drums and habituated to handling to ameliorate stress during testing. Before the actual day of drug testing, rats were given three training trials on revolving drums having an axis diameter of 6.0 cm and a corrugated surface for 2 days. Rats were placed on the drum rotating at lowest speed of 4 rpm and the speed was increased as the rate of 0.12 rpm/sec, maximally to 40 rpm. Rats able to remain on the revolving drum for a minimum of 120 sec were selected for drug testing. The mean of 3 training runs served as a control performance time. Rotarod performance time was measured at 20, 60, 90, 120, and 180 min after intrathecal injection. Each test was performed three times at 5-min intervals, and the mean values were compared.
We graded the placing and stepping function of the hind paw as follows: 0, normal brisk placing and stepping reflex response (normal weight bearing); 1) sluggish response to dragging the dorsum of hind paw at the edge of table (weakness of the hind paws and poorly coordinated movement of the hind limbs during ambulation); and 2) no reflex (significant flaccidity and loss of weight bearing in the hindquarters).
Withdrawal threshold data from von Frey hair testing were obtained as the actual threshold in grams and were converted to %MPE using the formula: %MPE for antiallodynia=([postdrug threshold-baseline threshold]/[15 g-baseline threshold]) ×100, where postdrug threshold means the largest threshold observed after intrathecal injection. The cutoff value was defined as a stimulus intensity of 15 g for the mechanical threshold (i.e., %MPE=100). The peak drug effect was used to calculate a %MPE, and these data were used to plot a %MPE versus log dose curve. The ED50 values, slopes, and 95% confidence intervals were calculated using dose-response data. Variances and its 95% confidence intervals for the theoretical ED50 may also be calculated from the variances of each component administered alone (16). To determine whether the drug interaction is additive or synergistic, isobolographic analysis was performed. An isobologram was constructed by plotting the ED50 value for gabapentin on the x axis and the ED50 values for R-PIA on the y axis. Individual ED50 values for each agonist were resolved from the combination dose required to cause 50% MPE and were plotted on the isobologram as the experimental combination dose. The theoretical additive dose of combination was calculated. Experimental values were compared with theoretical additive values as defined by the theoretical additive line. The theoretical additive point lies on a line connecting the ED50 values of the individual drugs, and experimental values that lie below and to the left of this additive line were considered to be synergistic.
Data were expressed as mean±SEM. The difference between the theoretical additive ED50 value and the experimental ED50 value was compared using a Student's t-test. The least antagonistic effect for each pretreatment group was compared with the peak agonistic effect of the combination group using the unpaired t-test. A p value <0.05 was considered to be statistically significant.
After spinal nerve ligation, most rats displayed normal general behavior and weight gain. After catheter implantation in the animals with nerve ligation, the thresholds for evoking hindpaw withdrawal were in the range of 1-4 g for all rats.
Intrathecal gabapentin, R-PIA, and their combination resulted in a dose-dependent antiallodynic effect (Fig. 1). Although not being closely paralleled, the slope of the combination group was shifted to the left side in larger doses compared with gabapentin (3-300 μg) and R-PIA (10 μg), respectively (Fig. 1). The ED50 values and slopes (95% confidence intervals) were as follows: 10.4 (5.3-20.4) μg and 39.5 (26.4-52.6) for gabapentin, 0.2 (0.1-0.3) μg and 35.2 (25.6-44.7) for R-PIA, and 1.8 μg (1.4-2.2) and 70.7 (50.2-91.3) for their combination, respectively. The high slope value of the combination group could reflect an increased efficacy. The time-effect courses of these two agonist groups and their combination groups were similar in general (Fig. 2). The maximal effects occurred within 15-30 min and then gradually decreased up to the previous baseline level over time for all doses of each group. There was a dose-dependent increase in magnitude and duration of the effect. A somewhat longer antiallodynic time course was observed in some rats after the injections of gabapentin 100 or 300 μg and R-PIA 1, 3 or 10 μg. Intrathecal normal saline produced only a slight increase in withdrawal response, which means that vehicles do not have an effect on the action of each drug and their combination.
A synergistic effect was found in the gabapentin plus R-PIA combination group (Fig. 3). The experimentally determined gabapentin plus R-PIA combination ED50 (±SEM) was 1.7 (±0.2) μg for gabapentin and 0.03 (±0.006) μg for R-PIA. The theoretical additive ED50 was calculated to be 5.2 (±1.1) μg for gabapentin and 0.1 (±0.02) μg for R-PIA. The experimental value of the gabapentin plus R-PIA combination group was significantly smaller than the calculated theoretical additive value (p<0.05). The standard errors of these two points on the isobologram show that they do not overlap, which supports a significant synergistic interaction.
Pretreatment with DPCPX remarkably attenuated the maximal antiallodynic effect produced by the intrathecal gabapentin plus R-PIA combination after 15 min (p<0.05) (Fig. 4). In the DPCPX pretreatment group, the antiallodynic effect of both drug combination was significantly reversed during the entire experiment. DPCPX alone produced only a slight increase in %MPE (data not shown) and this suggests that DPCPX does not have an effect on antiallodynia.
Some rats showed mild-to-moderate motor weakness or sedation with the largest dose of each drug, but no severe motor weakness or sedation was observed in any rats. The incidence and magnitude of side effects were not considerably increased in the combination group. Moderate motor weakness was observed in 2 rats (1 in the gabapentin 300 μg group and 1 in the R-PIA 10 μg group). No other adverse effects were noted. The occurrence of mild-to-moderate motor weakness returned to the baseline level within 3 hr. The sedative effect also returned to the baseline level within 3 hr.
We observed no significant change in rotarod performance time at gabapentin (3-100 μg), R-PIA (0.03-10 μg), and gabapentin plus R-PIA combination. However, at a dose of gabapentin 300 μg, the locomotor function was significantly decreased from 20 to 60 min after drug administration (Fig. 5).
We found that intrathecal gabapentin, R-PIA and their combination produced a dose-dependent increase of withdrawal threshold for a spinally-mediated mechanical allodynia. In addition, we observed that gabapentin enhanced the effect of R-PIA synergistically when coadministered intrathecally.
It has already been reported that the allodynic response to mechanical stimuli could be attenuated by intrathecal administration of R-PIA in a dose-dependent manner, but there were no significant motor weakness (17, 18). It is confirmed that such an antiallodynic effect is mediated by the spinal adenosine A1 receptor subtype with administration of the selective antagonist (17). Several animal neuropathic pain models induced by sciatic chronic constriction injury and intrathecal strychnine suggest an antiallodynic effect mediated by the spinal adenosine A1 receptor (17-19). We also observed a similar result in this spinal nerve ligation model after administration of intrathecal R-PIA.
Previous studies demonstrated that both A1 and A2 receptor subtypes are concentrated in a very small area of the dorsal horn and are only localized diffusely throughout the ventral horn (20). It is reported that there was no evidence for up-regulation in spinal A1 receptors after spinal nerve ligation and that spinal cord adenosine was decreased after spinal nerve ligation (21).
Gabapentin is an anticonvulsant that was synthesized as a structural analog to gamma-aminobutyric acid (22). Intrathecal or systemic administration of gabapentin diminishes hyperalgesia in tissue injury pain models without affecting acute noxious stimuli threshold (23, 24). Furthermore, the antinociceptive effect of gabapentin is more powerful after intrathecal rather than systemic administration (25). These findings suggest that gabapentin may alter the facilitated state and the major site of action of gabapentin may be the spinal cord. Although the mechanisms of action of gabapentin are not clear, the relations to specific receptors (22, 23) or substances (26), L-amino acid transporter (27), or voltagedependent calcium channel (28) has been proposed as the site of action of gabapentin. It has been reported that gaba-pentin decreases glutamate concentrations and inhibits the release of glutamate and glutamatergic synaptic transmission presynaptically (29). Glutamate acts on the NMDA and non-NMDA receptor and shows the excitatory effect (30). Further, the AMPA-evoked neuronal response is inhibited by gabapentin (31).
In our experiments, the interaction between gabapentin and R-PIA was synergistic. We suggested that the antiallodynic effect found in the combination group was mediated by the independent receptor systems at the spinal level and there was an attenuation in dose for each drug, and we thought it was a synergistic interaction.
Although we cannot know the exact mechanism, there are two possible explanations for synergistic effect. First, it could be thought of a change in agonist affinity. An increase in slope might reflect increased efficacy. In our experiments, the slope was increased in the combination group and was shifted to the left in large doses, which may explain a synergistic interaction. Second, we could suggest the possibility of functional receptor interaction. It is anticipated that the frequency of motor weakness and sedation could be also enhanced with increase in the antiallodynic component. In our experiments, there were no siginificant changes in motor function and sedation by rotarod test, so it is hard to suggest the functional receptor interaction. However, the fact that the receptors for the sensory component are mainly located in the dorsal horn of spinal cord and that there may be an interaction of the A1 receptor with the gabapentin receptor shows the possibility of a functional receptor interaction. In animal behavioral tests, severe sedation after drug administration could decrease response to stimulations and mask the antiallodynic effect. The effect on motor performance is particularly crucial in studies of spinal A1 receptor agonists because of the possible action of a large dose of R-PIA in the motor neuron area of the spinal cord (7). Therefore, we measured rotarod performance test to examine drug-induced adverse effects, such as sedation or locomotor dysfunction. Experimental rats that adjusted to the rotarod did not show significant reduction in rotarod performance test after gabapentin and R-PIA were coadministered. Thus, we suggest that the antiallodynic effect produced by gabapentin and R-PIA was not affected by drug-induced sedation mainly because the amounts of doses of each drug were quite small. The difference in action site and receptor number and function changes after nerve injury may affect the results (32). With respect to reduced side effect and synergistic effect, a combination therapy administering a smaller dose of each drug and a target-specific treatment using R-PIA and gabapentin may be beneficial to the management of allodynia.
We performed an antagonistic study with pretreatment of DPCPX in the combination subgroup to investigate the reversal effect, and maximal antiallodynic effect was reversed. These findings may suggest that spinal gabapentin is independently necessary for the optimal function of R-PIA in producing a synergistic effect. In our experiment, we chose only the A1 antagonist DPCPX because the A1 receptor subtype was most effective in the reversal of mechanical allodynia in the nerve ligation injury model (7). Unfortunately, we could not find exact gabapentin antagonist, so we could not perform the antagonistic study of gabapentin. However, with the present experiments we cannot rule out that other mechanisms could participate in this interaction.
In conclusion, gabapentin and R-PIA produced a dose-dependent antiallodynia without severe side effects and intrathecal gabapentin produced a synergistic interaction with R-PIA in a rat model of nerve ligation injury. Thus, these results suggest that activation of adenosine A1 receptors are required for the synergistic interaction between gabapentin and R-PIA in reducing mechanical allodynia.
Figures and Tables
Fig. 1
Dose-response curves from the peak effects of percent maximal possible effect (%MPE) for antiallodynia in the gabapentin, N6-(2-phenylisopropyl)-adenosine R-(-)isomer (R-PIA), and gabapentin plus R-PIA groups. These curves show a dose-dependent antiallodynic effect. Data are expressed as mean±SEM. Doses (μg) are represented logarithmically on the x axis and peak %MPE is represented on the y axis. Asterisks indicate that the mean %MPE of each group is significant compared with the smallest dose. *p<0.05; unpaired t-test. I.T., intrathecal injection.

Fig. 2
Time course of antiallodynic effects by intrathecal injection of gabapentin (A), N6-(2-phenylisopropyl)-adenosine R-(-) isomer (R-PIA) (B), and gabapentin plus R-PIA (C). These curves show a dose-dependent antiallodynic effect in each group. Data are expressed as mean±SEM. Asterisks indicate that mean percent maximal possible effect (%MPE) of each group for antiallodynia at that time point is significant compared with baseline value. *p<0.05; one-way repeated-measures analysis of variance followed by multiple comparisons (Tukey's method). I.T., intrathecal injection.

Fig. 3
Isobologram for the intrathecal interaction of gabapentin and N6-(2-phenylisopropyl)-adenosine R-(-)isomer (R-PIA). Horizontal and vertical bars indicate SEM. The diagonal line connecting both 50% effective dose (ED50) points is the theoretical additive line. The ED50 point A is calculated from the ED50 values and 95% confidence intervals of each drug. The experimental ED50 point B lies far below the line of additivity, indicating significant synergism.
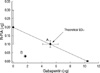
Fig. 4
Antagonism by 8-cyclopentyl-1,3-dipropylxanthine (DPCPX) pretreatment. Pretreatment with DPCPX 10 μg was performed 15 min before injection of a large dose in the gabapentin plus N6-(2-phenylisopropyl)-adenosine R-(-)isomer (R-PIA) group. Graphs show the time course of the antiallodynic effect in the combination group and pretreatment groups. Data are expressed as mean ±SEM. Maximal antagonism is seen after 30 and 45 min. Asterisks indicate that mean percent maximal possible effect (%MPE) of pretreatment groups for antiallodynia at that time point is significantly less compared with the gabapentin plus R-PIA group. *p<0.05; unpaired t-test. I.T.; intrathecal injection.

Fig. 5
Effects of intrathecal injection of gabapentin, N6-(2-phenylisopropyl)-adenosine R-(-)isomer (R-PIA), and gabapentin plus R-PIA on rotarod performance time. Rotarod performance time was measured before (baseline) and after drug administration. Rotarod performance time was not reduced by administration of gabapentin 100 μg and R-PIA 3, 10 μg, and gabapentin 5 μg plus R-PIA 0.1 μg. Rotarod performance time was significantly decreased at 20 and 60 min after the injection of gabapentin 300 μg. The results are expressed as the mean±SEM. *p<0.05 vs. baseline group by repeated-measures analysis of variance and Tukey's method. I.T., intrathecal injection.

References
1. Kim SH, Chung JM. An experimental model for peripheral neuropathy produced by segmental spinal nerve ligation in the rat. Pain. 1992. 50:355–363.
2. Kim KJ, Yoon YW, Chung JM. Comparison of three rodent neuropathic pain models. Exp Brain Res. 1997. 113:200–206.

3. Ralevic V, Burnstock G. Receptors for purines and pyrimidines. Pharmacol Rev. 1998. 50:413–492.
5. Sawynok J. Purines in pain management. Curr Opin CPNS Invest Drugs. 1999. 1:27–38.
6. Klotz KN. Adenosine receptors and their ligands. Naunyn Schmiedebergs Arch Pharmacol. 2000. 362:382–391.

7. Lee YW, Yaksh TL. Pharmacology of the spinal adenosine receptor which mediates the antiallodynic action of intrathecal adenosine agonists. J Pharmacol Exp Ther. 1996. 277:1642–1648.
8. Luo ZD, Calcutt NA, Higuera ES, Valder CR, Song YH, Svensson CI, Myers RR. Injury type-Specific calcium channel α2δ-1 subunit up-regulation in rat neuropathic pain models correlates with antiallodynic effects of gabapentin. J Pharmacol Exp Ther. 2002. 303:1199–1205.
9. Field MJ, Oles RJ, Lewis AS, McCleary S, Hughes J, Singh L. Gabapentin (neurontin) and S-(+)-3-isobutylgaba represent a novel class of selective antihyperalgesic agents. Br J Pharmacol. 1997. 121:1513–1522.

10. Eckhardt K, Ammon S, Hofmann U, Riebe A, Gugeler N, Mikus G. Gabapentin enhances the analgesic effect of morphine in healthy volunteers. Anesth Analg. 2000. 91:185–191.

11. Matthews EA, Dickenson AH. A combination of gabapentin and morphine mediates enhanced inhibitory effects on dorsal horn neuronal responses in a rat model of neuropathy. Anesthesiology. 2002. 96:633–640.

12. Gilron I, Biederman J, Jhamandas K, Hong M. Gabapentin blocks and reverses antinociceptive morphine tolerance in the rat paw-pressure and tail-flick tests. Anesthesiology. 2003. 98:1288–1292.

13. Dworkin RH, Backonja M, Rowbotham MC, Allen RR, Argoff CR, Bennett GJ, Bushnell MC, Farrar JT, Galer BS, Haythornthwaite JA, Hewitt DJ, Loeser JD, Max MB, Saltarelli M, Schmader KE, Stein C, Thompson D, Turk DC, Wallace MS, Watkins LR, Weinstein SM. Advances in neuropathic pain: diagnosis, mechanisms, and treatment recommendations. Arch Neurol. 2003. 60:1524–1534.
14. Yaksh TL, Rudy TA. Chronic catheterization of the spinal subarachnoid space. Physiol Behav. 1976. 17:1031–1036.

15. Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL. Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods. 1994. 53:55–63.

16. Tallarida RJ, Porreca F, Cowan A. Statistical analysis of drug-drug and site-site interactions with isobolograms. Life Sci. 1989. 45:947–961.

17. Cui JG, Sollevi A, Linderoth B, Meyerson BA. Adenosine receptor activation suppresses tactile hypersensitivity and potentiates spinal cord stimulation in mononeuropathic rats. Neurosci Lett. 1997. 223:173–176.

18. von Heijne M, Hao JX, Sollevi A, Xu XJ, Wiesenfeld-Hallin Z. Marked enhancement of anti-allodynic effect by combined intrathecal administration of the adenosine A1-receptor agonist R-phenylisopropyladenosine and morphine in a rat model of central pain. Acta Anaesthesiol Scand. 2000. 44:665–671.

19. Sosnowski M, Yaksh TL. Role of spinal adenosine receptors in modulating the hyperesthesia produced by spinal glycine receptor antagonism. Anesth Analg. 1989. 69:587–592.

20. Choca JI, Proudfit HK, Green RD. Identification of A1 and A2 adenosine receptors in the rat spinal cord. J Pharmacol Exp Ther. 1987. 242:905–910.
21. Bantel C, Tobin JR, Li X, Childers SR, Chen SR, Eisenach JC. Intrathecal adenosine following spinal nerve ligation in rat: short residence time in cerebrospinal fluid and no change in A(1) receptor binding. Anesthesiology. 2002. 96:103–108.
22. Taylor CP, Gee NS, Su TZ, Kocsis JD, Welty DF, Brown JP, Dooley DJ, Boden P, Singh L. A summary of mechanistic hypotheses of gabapentin pharmacology. Epilepsy Res. 1998. 29:233–249.

23. Yoon MH, Yaksh TL. The effect of intrathecal gabapentin on pain behavior and hemodynamics on the formalin test in the rat. Anesth Analg. 1999. 89:434–439.

24. Matthews EA, Dickenson AH. A combination of gabapentin and morphine mediates enhanced inhibitory effects on dorsal horn neuronal responses in a rat model of neuropathy. Anesthesiology. 2002. 96:633–640.

25. Chapman V, Suzuki R, Chamarette HL, Rygh LJ, Dickenson AH. Effects of systemic carbamazepine and gabapentin on spinal neuronal responses in spinal nerve ligated rats. Pain. 1998. 75:261–272.

26. Petroff OA, Hyder F, Rothman DL, Mattson RH. Effects of gabapentin on brain GABA, homocarnosine, and pyrrolidinone in epilepsy patients. Epilepsia. 2000. 41:675–680.

27. Su TZ, Lunney E, Campbell G, Oxender DL. Transport of gabapentin, a gamma-amino acid drug, by system L alpha-amino acid transporters: a comparative study in astrocytes, synaptosomes, and CHO cells. J Neurochem. 1995. 64:2125–2131.
28. Shimoyama M, Shimoyama N, Hori Y. Gabapentin affects glutamatergic excitatory neurotransmission in the rat dorsal horn. Pain. 2000. 85:405–414.

29. Maneuf YP, McKnight AT. Block by gabapentin of the facilitation of glutamate release from rat trigeminal nucleus following activation of protein kinase C or adenylyl cyclase. Br J Pharmacol. 2001. 134:237–240.

30. Leem JW, Choi EJ, Park ES, Paik KS. N-methyl-D-aspartate (NMDA) and non-NMDA glutamate receptor antagonists differentially suppress dorsal horn neuron responses to mechanical stimuli in rats with peripheral nerve injury. Neurosci Lett. 1996. 211:37–40.

31. Fink K, Meder W, Dooley DJ, Gothert M. Inhibition of neuronal Ca2+ influx by gabapentin and subsequent reduction of neurotransmitter release from rat neocortical slices. Br J Pharmacol. 2000. 130:900–906.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download