Abstract
Fibrovascular polyps of the esophagus and hypopharynx are benign tumors of the upper digestive tract. The majority of these polyps are located in the upper part of the esophagus but the hypopharyngeal fibrovascular polyps are only rarely seen. Most of them are surgically treated and this is usually done through a cervical incision, although some of them have been removed endoscopically. The authors report here on a case of a 63-yr-old-man with a giant fibrovascular polyp of the hypopharynx that extended into the stomach; this polyp was removed through simultaneous transcervical and transabdominal approaches because of the huge size of the polyp. The man presented with progressive dysphagia of 1 yr duration. The preoperative assessment revealed a giant polyp arising from the left arytenoid and extending into the stomach. The dimension of the polyp was about 26×10×4 cm. The complete resection of the polyp with the simultaneous transcervical and transabdominal approaches was successful, and it was diagnosed as a fibrovascular polyp. The patient has been followed up without any recurrence for 6 month postoperatively.
Fibrovascular polyps of the esophagus and hypopharynx are benign tumors of the upper digestive tract. The hypopharyngeal fibrovascular polyps are rare diseases; they can vary in size, and regurgitation of them with subsequent aspiration and asphyxia is a possibility. Most of them are usually surgically treated through a cervical incision, although some have been removed endoscopically.
This case report describes a giant fibrovascular polyp of the hypopharynx that was removed through using simultaneous transcervical and transabdominal approaches because of the huge size of the polyp.
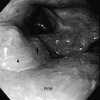
A 63-yr-old man was transferred to our hospital due to his Progressive dysphagia that he had suffered with for 1 yr. His past medical history was not significant except for his dyspepsia of 4 yr duration and also his atrial fibrillation of 2 yr duration. No specific abnormality was demonstrated on the physical examination. The esophagogram demonstrated a contrast-filling defect from the cervical esophagus to the upper body of the stomach. The computed tomography (CT) scan demonstrated a soft tissue lesion in the esophagus from the level of the cervical esophagus to the level of the upper body of the stomach. This lesion consisted of a long slender stalk and an ovoid head. The dimension of the head of polyp in the stomach was about 8×5 cm in size. The central portion of the lesion showed attenuation identical to that of subcutaneous fat (Fig. 1). Esophagogastroscopy demonstrated a whitish polyp that originated from the left arytenoid (Fig. 2). On the endoscopic biopsy done on the head of the polyp, there was no abnormality except for the acanthotic squamous epithelium. Endoscopic ultrasonogram (EUS) demonstrated a heterogeneous echogenic lesion with a central star-shaped hypoechoic area. An operation was planned under the impression of fibrovascular polyp of the hypopharynx. The laryngoscopic and esophagoscopic evaluation of the hypopharynx under general anesthesia revealed that the stalk was attached to the anterior wall of the hypopharynx from the posterior mucosa of the left arytenoid to the post-cricoid region. A trial to divide the stalk at the base with a laser was done, but the base of the polyp was too broad to be divided under the laryngoscopic operative field. After a transverse cervical incision was made, left lateral pharyngotomy was made longitudinally from the left pyriform sinus down to the upper cervical esophagus. The mucosal origin of the remnant stalk was resected and suture-closed. The resulting mucosal defect was primarily repaired with interrupted 4-0 Vicryl sutures. After upper median laparotomy and division of the stalk, the mass was removed through gastrotomy. The dimension of the polyp was about 26×10×4 cm in size. Grossly, the polyp was covered with a mucous membrane and the divided surface showed as being yellow to white-tan with a myxoid appearance (Fig. 3). There was not any abnormality except for the traumatic mucosal bruise that was due to manipulation during operation. The histological features were those of a fibrovascular polyp. The polyp was lined by squamous epithelium with focal acanthosis. The core of the polyp was composed of adipose and fibrovascular tissue. The patient has been followed up without recurrence for 6 months postoperatively.
Benign esophageal tumors are uncommon and they represent less than 1% of the esophageal neoplasms (1). Fibrovascular polyps of the esophagus and hypopharynx are benign tumors of the upper digestive tract. Fibrovascular polyps occur commonly in older men between 60 and 70 yr of age and these polyps grow slowly (2). However, Seshul et al. (3) and Paik et al. (4) have reported a case of fibrovascular polyp in an infant, respectively. The majority, about 85%, are located in the upper part of the esophagus (5). These polyps usually originate as small mucosal tumors just below the cricopharyngeus muscle sphincter, then extend into the esophageal lumen by the constant downward urge of both food and peristalsis, and they may reach into the stomach (2). In the present case, the polyp was attached to an unusual site, the anterior wall of the hypopharynx from the posterior mucosa of the left arytenoid to the post-cricoid region. The dimension of the polyp was about 26×10×4 cm in size.
Fibrovascular polyps occur frequently as solitary lesions (2). Yet Nuyens et al. have reported multiple synchronous fibrovascular polyps (6); they were collections of fibrous, vascular, and adipose tissue lined by normal squamous epithelium. Most of the patients generally complain of dysphagia and respiratory symptoms. Regurgitation of a polyp into the hypopharynx with subsequent aspiration and asphyxia is possible (1).
Fibrovascular polyps can be detected by either barium esophagogram or esophagoscopy. However, detection by esophagoscopy may be difficult or impossible because fibrovascular polyps can fill the esophageal lumen and have a composition similar to the mucosa of the esophagus (1). In our case, considering the slow growth pattern of fibrovascular polyps and the patient's history of dyspepsia for 4 yr, there was possibility that this polyp escaped detection at the previous esophagoscopy procedure.
EUS may help to assess the vessels in the pedicle, and EUS-guided fine-needle aspiration may be helpful for the histological diagnosis(7,8). In the present case, EUS demonstrated a heterogeneous echogenic lesion with a central star-shaped hypoechoic area and it was useful for the diagnosis. Even after a thorough preoperative examination including endoscopy, EUS, barium study and CT scan, fibrovascular polyps can be mistakenly diagnosed as an intramural mass. And a drastic and unnecessary surgical procedure, such as esophagectomy with colon interposition may have been resulted (9).
The surgical technique is chosen after assessing the origin, size and vascularity of the pedicle and the size of the tumor mass (2). Coexistent cancer in the overlying mucosa should be ruled out (10). Most polyps are surgically treated, although some have been removed endoscopically (1). Small polyps that are less than 2 cm in diameter with a thin pedicle may be removed by endoscopic ligation and electrocoagulation of the pedicle (11). Polyps larger than 8 cm in length or those with a thick, richly vascularized pedicle should be removed by surgical excision, and usually through a cervical incision (12). Finding the exact location of base of the stalk is essential for the surgical strategy. Oh et al. had some difficulty in resecting a fibrovascular polyp from the cervical esophagus via right thoracotomy because of the preoperative difficulty in localizing the stalk (13). The incision necessary to expose the esophagus depends on the site of the mucosal origin of the pedicle, since the pedicle has to be resected under direct visualization. The neck incision is made on the side opposite the origin of the tumor. In this case, during the laryngoscopic and esophagoscopic evaluation, the exact site of origin of the pedicle became obscure because of poor visualization, and so the left side was chosen. Because the origin of the pedicle was attached to the anterior wall of the hypopharynx from the left arytenoid to the post-cricoid region, it was not difficult to divide the stalk. In this case, the broad base of the stalk was divided by performing pharyngotomy. The size of the head of the polyp, however, was too large to be removed through the pharyngotomy. The entire polyp, therefore, was removed via gastrotomy. We could not find any report about the surgical resection of fibrovascular polyp with the biapproach in the available literature. Surgical resection of a fibrovascular polyp with this biapproach seems to be useful in cases like this.
Local excision is curative and the recurrence after resection is rare (1). Drenth et al., however, reported a case of three recurrent fibrovascular polyps that recurred within 8 yr (14).
It is noteworthy that the presence of even a large intraluminal tumor may escape detection at esophagoscopy and so this could be suspected of being an intramural tumor. As for the correct surgical approach, the accurate assessment of the origin, size and vascularity of the pedicle and the size of the tumor mass is essential for the proper treatment.
Figures and Tables
Fig. 1
Sagittal view of a chest computed tomography scan of a 63-yr-old-man with a giant fibrovascular polyp. A soft tissue lesion (arrow) in the esophagus from the level of the cervical esophagus extends to the level of the upper body of the stomach. The exact location of the polyp's origin is obscure. The dimension of the head (arrowhead) is about 8×5 cm in size. The central portion of the lesion shows attenuation identical to that of subcutaneous fat.

References
1. Rice TW, Murthy SC. Sellke FW, del Nido PJ, Swanson SJ. Surgical treatment of benign esophageal diseases. Sabiston & Spencer Surgery of the Chest. 2005. Volume I:7th ed. Philadelphia: Elsevier Saunders;583–609.

2. Shamji F, Todd TR. Pearson FG, Cooper JD, Deslauriers J, Ginsberg RJ, Hiebert CA, Patterson GA, Urschel HC, editors. Benign tumors. Esophageal Surgery. 2002. 2nd ed. Philadelphia: Churchill Livingstone;637–654.
3. Seshul MJ, Wiatrak BJ, Galliani CA, Odrezin GT. Pharyngeal fibrovascular polyp in a child. Ann Otol Rhinol Laryngol. 1998. 107:797–800.

4. Paik HC, Han JW, Jung EK, Bae KM, Lee YH. Fibrovascular polyp of the esophagus in infant. Yonsei Med J. 2001. 42:264–266.

5. Jang GC, Clouse ME, Fleischner FG. Fibrovascular polyp: a benign intraluminal tumor of the esophagus. Radiology. 1969. 92:1196–1200.
6. Nuyens MR, Bhatti NI, Flint P. Multiple synchronous fibrovascular polyps of the hypopharynx. J Otorhinolaryngol Relat Spec. 2004. 66:341–344.

7. Avezzano EA, Fleischer DE, Merida MA, Anderson DL. Giant fibrovascular polyps of the esophagus. Am J Gastroenterol. 1990. 85:299–302.
8. Devereaux BM, LeBlanc JK, Kesler K, Brooks J, Lehman GA, Sherman S, Ciaccia D. Giant fibrovascular polyp of the esophagus. Endoscopy. 2003. 35:970–972.

9. Schuhmacher C, Becker K, Dittler HJ, Hofler H, Siewert JR, Stein HJ. Fibrovascular esophageal polyp as a diagnostic challenge. Dis Esophagus. 2000. 13:324–327.

10. Marcial-Rojas RA, Suan P. Epidermoid carcinoma in mucosa overlying a pedunculated lipoma of the esophagus. J Thorac Surg. 1959. 37:427–434.

11. Tasaka Y, Makimoto K, Yamauchi M, Haebara H. Benign pedunculated intraluminal tumor of the esophagus. J Otolaryngol. 1982. 11:111–115.
12. van Lanschot JJ, Poublon RM, Zonderland HM, van Houten H. Benign pedunculated tumor of the esophagus. Neth J Surg. 1987. 39:83–85.
13. Oh SS, Shim YM. Giant fibrovascular polyp of the esophagus: a case report. Korean J Thorac Cardiovasc Surg. 1996. 29:675–680.
14. Drenth J, Wobbes T, Bonenkamp JJ, Nagengast FM. Recurrent esophageal fibrovascular polyps: case history and review of the literature. Dig Dis Sci. 2002. 47:2598–2604.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download