Abstract
Syphilis is an unexpected diagnosis in the stomach, and the reduced incidence of syphilis has made its clinical presentation less widely appreciated. We report a 43-yr-old man suffering from epigastric tenderness with an initial diagnosis of gastric carcinoma; gastric syphilis was confirmed by demonstrating spirochetes in a gastric biopsy specimen by silver impregnation. Excessive lymphoplasmacytic infiltration with diffuse thickening of gastric rugae should raise suspicion of gastric syphilis, which should be considered in the differential diagnosis of diffuse erosive gastritis and infiltrative lesions of the stomach.
Gastric involvement by syphilis usually occurs during the secondary or tertiary stages. Nonetheless, it is rarely recognizable clinically and the introduction of antibiotics has led to a dramatic reduction in its incidence. However, this relatively rare disease often presents a diagnostic dilemma because it lacks pathognomonic clinical findings and often resembles neoplastic conditions such as gastric cancer or malignant lymphoma (1,2). Recently, one study showed that the outbreak of primary and secondary syphilis among HIV-positive patients started in 2002 in Korea (3). In particular, its diagnosis based on a histologic evaluation of the gastrectomized specimen has infrequently been reported (1,4). Herein, we report a case of secondary syphilis which was diagnosed by silver staining of a gastrectomized specimen.
A 43-yr-old, apparently healthy man presented with a one month history of epigastric tenderness and anorexia. The patient visited a local clinic where he underwent an endoscopic examination with biopsy and the pathologic diagnosis was gastric adenocarcinoma. He was transferred to our hospital for further evaluation. His family history and past history were negative for any gastrointestinal disease, abdominal surgery or significant medical illness. Physical examinations were normal except minimal epigastric tenderness only. A laboratory evaluation revealed reduced hemoglobin concentration (12.8 g/dL) and hematocrit (39.1%). White blood cell count was normal but his differential count showed decreased lymphocytes (16.8%) and increased monocytes (10.4%) fraction. Total serum protein level (6.3 g/dL) was normal but his albumin level (3.3 g/dL) was relatively lower. Serum bilirubin and total liver enzymes were within normal ranges. Tumor markers including CEA, CA-19-9 and CA-72-4 were within normal ranges. His electrocardiogram and chest roentgenogram were normal. An upper gastrointestinal tract series showed an infiltrating encircling mass from the mid body to the pylorus. The mass was suspicious for duodenal bulb invasion with poor dispensability and which was believed to represent a linitis plastica-like tumor (Fig. 1). A computed tomographic scan of the abdomen with contrast revealed nonspecific mural thickening involving the prepyloric antrum and duodenal bulb with focal obliteration of the fat plane between the head of pancreas and the gastric antrum (Fig. 2). Gastroscopy showed an area of diffuse mucosal nodularity with several ulcerations with intervening hyperemic and friable gastric mucosa from the antrum to anterior side of mid-body (Fig. 3). An endoscopic gastric biopsy specimen showed the chronic inflammation with extensive lymphoplasmacytic infiltrates (Fig. 4). Extraordinary gastritis of uncertain cause or a lymphoid malignancy was included in the differential diagnosis. Lymphocyte phenotyping performed on gastric biopsy material showed no monoclonality of B cells.
An exploratory laparotomy was performed, and the gastric wall was found to be diffusely thickened. A Billroth II anastomosis was performed with biopsy of adjacent enlarged nodes. The gastric wall was diffusely thickened and the mucosal surface revealed prominent, swollen, erythematous rugal folds with erosions (Fig. 5). The histologic examination revealed a dense lymphoplasmacytic infiltration along the mucosa and submucosa in which some areas became confluent. Moreover, this infiltration was associated with a loss of glands (Fig. 6). The pathologic differential diagnoses were syphilitic gastritis, cytomegalovirus (CMV)-gastritis, tuberculosis and low possibility of lymphoma. However, an acid-fast staining and CMV immunostaining were negative. Performed IgH gene rearrangement was also negative. Warthin-Starry staining revealed myriad spirochetes infiltrating mucosal glands and vessels throughout the lamina propria (Fig. 7). Serum VDRL was positive with a titer of 1 to 64, and FTA-ABS was reactive. Antibodies to human immunodeficiency virus (HIV) were absent by ELISA. The patient was treated with penicillin but was unavailable for further clinical follow-up.
Gastric syphilis most commonly affects young adults in the second to fourth decade of life. Epigastric pain, anorexia, nausea, vomiting and weight loss are common symptoms in gastric syphilis (2), but there are no clear diagnostic criteria. The upper gastrointestinal tract series may reveal marked hourglass-like deformity of the pyloric region or the middle part of the stomach, mimicking linitis plastica, or obstruction of the gastric outlet (5). The stomach may also be fixed and contrasted with thick rugae, as was the situation in the present case.
Gastroscopy may reveal purplish ulcer margins with necrosis accompanying edematous, friable mucosa with hemorrhages and atrophic, erosive, or infiltrative gastritis (4,6). Gastric carcinoma must be considered in 85-95% of patients with gastric syphilis as in the present case.
The histologic diagnosis of syphilis is exceedingly difficult. Common histologic changes include thickened arterial walls with perivascular round cell infiltrates, and markedly thickened submucosa with diffuse infiltration of lymphocytes and plasma cells as well as endovasculitis. Chronic inflammation due to prominent plasma cells and lymphocytic infiltration suggests that syphilis be investigated as a potential cause. In present case, endovasculitis or hypertrophic arterial or venular walls were not prominent.
A fluorescent antibody test, the standard treponemal test in use today, is routinely performed to all the admissions at hospital. Serological testing is the most widely used laboratory technique for the diagnosis of syphilis. However, the VDRL test has a false-positive rate of around 1%, usually among patients with systemic lupus erythematosus or other autoimmune and connective tissue disease.
Spirochetes are not always obvious in endoscopic biopsy specimens in gastric syphilis (2). Silver stains, immunofluorescent or immunoperoxidase stains for T. pallidum are usually required to identify spirochetes (7,8). Moreover, several studies have demonstrated that syphilis, and other genitalulcer diseases, are more common in HIV-infected persons. Recently, several reports have been issued on gastric syphilis (9-11).
In summary, a high index of suspicion is important for this disease. Patients with gastric syphilis are typically young with symptoms mimicking a gastric neoplasm. Moreover, the clinical, endoscopic, and microscopic appearance of gastric syphilis may easily be confused with gastric lymphoma or linitis plastic carcinoma of the stomach. The most common symptoms of gastric syphilis are abdominal pain, nausea, vomiting, gastrointestinal bleeding, weight loss, early satiety and anorexia. The endoscopic appearance may vary from diffuse edema, erythema, friable or multiple erosions, to ulceration. Moreover, endoscopic gastric mucosal biopsies are often nonspecific histologically. If the clinician considers syphilis and obtains VDRL and FTA-ABS, a diagnosis can be confirmed. The patient may then be treated appropriately, and spared unnecessary surgery.
Figures and Tables
Fig. 1
Double-contrast radiography demonstrating an infiltrating encircling mass extending from the mid-body to the pylorus with poor dispensability.

Fig. 2
A computed tomographic scan of the abdomen shows mural thickening involving the prepyloric antrum and duodenal bulb with focal obliteration of the fat plane between the pancreas head and gastric antrum.
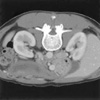
Fig. 3
Gastroscopy revealed a diffuse mucosal nodularity with several ulcerations with intervening hyperemic friability from the antrum to mid-body.

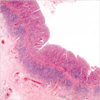
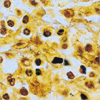
Fig. 4
Biopsy specimens revealed marked lymphoplasmacytic infiltrate with polymorphonuclear leukocytes and with destruction of gastric glandular epithelium (H&E, ×200).
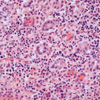
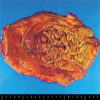
Fig. 5
The mucosa of gastric specimen shows reddish-purple, swollen, and thickened erythematous rugal folds with erosion.
ACKNOWLEDGEMENTS
The authors thank Dr. Min-Geol Lee, Department of Dermatology and Cutaneous Biology Research Institute, Yonsei University College of Medicine, Korea for his comment and kind gift of antibody.
References
1. Abdu RA, Carter K, Pomidor WJ. Gastric syphilis mimicking linitis plastica. Arch Surg. 1993. 128:103–104.

2. Long BW, Johnston JH, Wetzel W, Flowers RH 3rd, Haick A. Gastric syphilis: endoscopic and histological features mimicking lymphoma. Am J Gastroenterol. 1995. 90:1504–1507.
3. Jang HC, Cho JH, Park WB, Lee KD, Lee CS, Kim HB, Oh MD, Choe KW. Outbreak of primary and secondary syphilis among HIV sero-positive patients in Korea. Infect Chemother. 2004. 36:366–372.
4. Yoshida K, Tada S, Ueno N, Owan T, Suko H, Kamio T, Matsumoto T. Gastric syphilis. Gastrointest Endosc. 2003. 58:908–909.

5. Morin ME, Tan A. Diffuse enlargement of gastric folds as a manifestation of secondary syphilis. Am J Gastroenterol. 1980. 74:170–172.
6. de Escalante Yanguela B, Lacasa Marzo J, Carrasquer Sese JA, Oncins Torres R, Palazon Astiz R, Sampedro Feliu JA. Gastric ulcers: a rare manifestation of secondary syphilis. An Med Interna. 1993. 10:287–289.
7. Lee WS, Lee MG, Chung KY, Lee JB. Detection of Treponema pallidum in tissue: a comparative study of the avidin-biotin-peroxidase complex, indirect immunoperoxidase, FTA-ABS complement techniques and the darkfield method. Yonsei Med J. 1991. 32:335–341.

8. Besses C, Sans-Sabrafen J, Badia X, Rodriguez-Mendez F, Salord JC, Armengol JR. Ulceroinfiltrative syphilitic gastropathy: silver stain diagnosis from biopsy specimen. Am J Gastroenterol. 1987. 82:773–774.
9. Winters HA, Notar-Francesco V, Bromberg K, Rawstrom SA, Vetrano J, Prego V, Kuan J, Raufman JP. Gastric syphilis: five recent cases and a review of the literature. Ann Intern Med. 1992. 116:314–319.

10. Fyfe B, Poppiti RJ Jr, Lubin J, Robinson MJ. Gastric syphilis. Primary diagnosis by gastric biopsy: report of four cases. Arch Pathol Lab Med. 1993. 117:820–823.
11. Greenstein DB, Wilcox CM, Schwartz DA. Gastric syphilis. Report of seven cases and review of the literature. J Clin Gastroenterol. 1994. 18:4–9.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download