Abstract
To identify differences in the clinical, radiologic, and microbiologic features of pulmonary tuberculosis (TB) in the young (<64 yr) and elderly (≥65 yr), we performed a retrospective analysis of the medical charts and chest radiographs of 207 young and 119 elderly pulmonary TB patients. Hemoptysis and a febrile sense were more frequent in the young, whereas weakness, dyspnea, anorexia, and mental change were more frequent in the elderly. Elderly patients showed higher frequencies of cardiovascular and chronic lung diseases, whereas the young showed a higher proportion of underlying liver disease. In addition, chest radiography showed a significantly higher frequency of mid or lower lung involvement by TB lesions in the elderly (10.6% vs. 22.7%, p<0.05). Lesions were frequently misdiagnosed as pneumonia or lung cancer in the elderly. However, there was no difference between these two groups in terms of sputum acid-fast bacilli positivity. The elderly showed a higher frequency of adverse drug reactions (18.5% vs. 40.7%, p<0.05), and higher TB-related mortality (1.3% vs. 11.1%, p<0.05). In conclusion this study showed that young and elderly pulmonary TB patients have similar microbiologic features; however, the elderly showed higher frequencies of atypical clinical and radiologic presentations, adverse drug reactions, and higher TB-related mortality.
Although the prevalence of active pulmonary tuberculosis (TB) among Koreans above 5 yr old decreased gradually from 5.1% (1,240,000 cases) in 1965 to 1.0% (429,000 cases) in 1995, there are still many TB patients in Korea (1, 2). Even in developed countries where the overall incidence of TB is low, pulmonary TB remains common among the elderly (3). Increases in the elderly population due to prolonged life expectancy have increased the use of drugs that suppress cellular immunity, and may further increase the incidence of pulmonary TB among the elderly in the future (4). Many studies have been performed on the pulmonary TB in the elderly (5-19). Some have suggested that pulmonary TB in the elderly presents somewhat atypical symptoms (6, 7) or radiological findings (8-10) or both (11), or that the elderly are more susceptible to adverse drug reactions (12, 13) and more likely to die of the disease (6, 14). Age-related changes in the tuberculin skin reaction and a high incidence of underlying illnesses also play a role in prolonging the final diagnosis (15). Some have even suggested that pulmonary TB in the elderly should be classified as a separate entity (16).
However, many studies (17-19) have reported that TB in the young and elderly shows similar clinical, bacteriological, and radiological features. Pulmonary TB is still one of the most prevalent diseases in Korea, and accordingly most physicians and radiologists are familiar with TB, and suspect the presence of TB in cases with undiagnosed pulmonary disease. Studies in this special situation would help our understanding of the characteristic clinical features of elderly pulmonary TB in areas where TB prevalence is intermediate. We previously performed a retrospective study to elucidate differences in the clinical, microbiological, and radiological features of TB in the young and elderly (20), and the result concurred with other studies as it suggested that the elderly have atypical clinical and radiologic characteristics. However, the study population was relatively small, and some of the radiological interpretations were not made by an experienced chest radiologist. Thus to confirm our previous study results, the present study was designed to incorporate a larger study population and to incorporate more consistent radiologic interpretation by experienced chest radiologists.
Medical records and chest radiographs of active pulmonary TB patients, who visited the Seoul National University Boramae Hospital during the period January 1994 to December 2000, were reviewed. We included only pulmonary TB cases and excluded all other forms of TB, like hilar and/or mediastinal lymphadenopathy, TB pleurisy, and miliary TB to allow better data comparisons. Cases of pulmonary TB with coexistent extrapulmonary TB were also excluded from the study population. During the study period, 428 cases of active pulmonary TB were treated using anti-TB medication. Thirty-five relapsed cases, 20 multi-drug resistant TB cases, and 47 cases already diagnosed as TB at other hospital were also excluded. Finally 326 patients that satisfied the above criteria were eligible for analysis. For comparison purposes, the 326 pulmonary TB patients were divided into two groups: patients aged less than 65 yr (the young patients) and those aged 65 yr or more (the elderly patients). All patients were human immunodeficiency virus (HIV) negative.
Sputum acid-fast bacilli (AFB) smear/cultures were performed at least three times. Bronchoscopy and washing for AFB detection was performed only in selected patients; only 14 young and 15 elderly underwent bronchoscopy procedure. Active pulmonary TB was diagnosed in the presence of at least one of the following criteria; 1) a positive sputum or bronchial washing fluid AFB smear and/or positive culture for M. tuberculosis regardless of sputum or bronchial washing fluid smear results; 2) biopsy-based histologic confirmation of the lung lesion; 3) chest radiographic findings compatible with TB and a favorable response to treatment in cases without bacteriologic or histologic confirmation.
Collected data included the following: demographic characteristics, presenting symptoms and body temperature, underlying illnesses, laboratory findings (including microbiologic study at the time of diagnosis), radiological features, adverse reaction to anti-TB drugs, and mortality during treatment. Initial presenting symptoms about which patients complained, and highest body temperature measured during initial presentation were included. A body axillary temperature above 37.5℃ was defined as elevated. The location, lesion appearance on initial chest radiographs, and first clinical diagnoses were recorded. TB lesion locations were categorized as upper lobe involvement (upper alone or upper with middle or lower) and isolated middle or lower lobe involvement. The radiologic appearances of TB lesions were classified as typical fibrous nodular and/or a cavitary lesion, a pneumonia-like lesion, a mass-like lesion, or as others. This radiologic classification was made according to interpretation of initial radiographs taken when patients first visited hospital before a definite diagnosis had been made. First clinical diagnoses were classified as TB, bacterial pneumonia, lung cancer, and others. After a diagnosis of active pulmonary TB had been made and medication started, all patients were seen one week after medication start by a physician and monthly thereafter, and at these visits were questioned about drug side effects. Liver function tests were checked after one week of medication, and were monitored by complete blood count (CBC) and simple chest radiography monthly thereafter.
Patients were treated initially using the following daily regimen: isoniazid 400 mg (300 mg for patients with a body weight <50 kg), rifampicin 600 mg (450 mg for patients with a body weight <50 kg), ethambutol 800mg (600 mg for those with a body weight <50 kg), pyrazinamide 1,500 mg (1,000 mg for those with a body weight <50 kg). Pyrazinamide was medicated through the entire treatment period if patients were tolerable and no adverse reaction occurred. In patients with underlying liver disease, e.g., liver cirrhosis or active hepatitis, pyrazinamide was not prescribed from the medication regimen from the start. Non-hepatotoxic drugs like cycloserine or quinolones were prescribed in patients with significant hepatotoxicity (serum transaminase >3 times the normal upper limit). But as soon as liver function recovered or stabilized, drug therapy regimens were cautiously changed to regimens that included isoniazid and rifampin. Treatment duration was at least 6 months.
Drug adverse reactions were defined as; 1) side effects that caused medication discontinuance or change (either temporally or permanently) and/or that directly resulted in hospitalization; or 2) when some other symptomatic treatment was necessary to relieve symptoms. Drug induced hepatitis by anti-TB medication was defined as; 1) a transaminase increase to >3 times the normal upper limit; and 2) any elevation of transaminase above basal levels in the presence of icteric hepatitis. If drug induced hepatitis was suspected then isoniazid, rifampicin, and pyrazinamide were stopped, but when liver function returned to normal the drugs were sequentially reintroduced. Pyrazinamide was not reintroduced. Mild side effects tolerated by patients, or transient mild leucopenia (>3,000/µL) were not considered major drug side effects. Prognosis during treatment was evaluated by mortality during treatment.
Statistical analysis was performed using the SPSS Version 11.0 software package. Statistical differences between the clinical features of the two groups were determined with chi-square test and Yates correction except when expected values of less than 5 required the use of the Fisher exact test. The Student's t test was used when indicated for independent means.
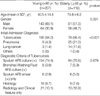
Three hundred twenty six patients who satisfied the above-mentioned inclusion criteria comprised the study population. Of these patients, 27 were transferred to other hospital after an initial diagnostic workup, and 67 dropped out during follow-up. There was no difference between the two groups in terms of transfer rate to other hospital or follow-up loss. Finally 232 patients completed their anti-TB medication, administered over a minimum of 6 months at our hospital, thus drug adverse reactions and prognosis were analyzed using their data. The clinical characteristics, initial diagnosis, and diagnostic criteria of pulmonary TB for the 326 subjects are shown in Table 1. Two hundred seven patients were allocated to the young age group and 119 to the elderly group. The mean ages of the young and elderly patients were 40.5 yr (range, 16-64 yr) and 74.8 yr (range, 65-85 yr). The young group showed a significant male predominance (p<0.001), and an initial diagnosis of active pulmonary TB was made correctly in 94.2% in the young group but in only 66.4% in the elderly group (p<0.001). Twenty-five of the 119 elderly groups were misdiagnosed as having bacterial pneumonia compared to 9 of the 207 young groups. Fourteen elderly patients but only 3 young patients were considered to have lung cancer initially. The diagnostic criteria of active pulmonary TB are presented in Table 1. No significant difference was observed between the two groups in terms of positive sputum AFB culture.
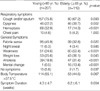
The proportions of patients with different symptoms are compared in Table 2. The data shown represent all cases. Cough was the most frequent symptom in both the young and elderly groups, without significance. However, hemoptysis was more frequent in the young, and dyspnea more frequent in the elderly. Nonspecific general symptoms like weakness, weight loss, anorexia, and mental change were more frequent in the elderly. Though a febrile sense was more frequent in the young, no significant difference was found between the two groups in terms of body temperature elevation. Fifteen of the 207 young patients were asymptomatic and presented only a chest radiographic abnormality compared to 2 of the 119 elderly (p=0.037). Symptom duration was significantly greater in the elderly.
Results are shown in Table 3. The number of active pulmonary TB patients with an underlying illness was significantly higher in the elderly group. Diabetes mellitus and liver disease (including alcoholic liver disease) composed the majority of underlying illnesses in both groups. Elderly had significantly higher frequencies of cardiovascular and chronic lung disease including pneumoconiosis and chronic obstructive lung disease, and the young had significantly higher frequencies of liver diseases. However, no statistically significant differences were found between the frequencies of other underlying diseases in the two groups.
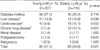
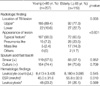
Radiological features are summarized in Table 4. In both groups, the active pulmonary TB lesion involved the upper lobe in the majority, but the elderly had a significantly higher frequency of isolated mid or lower lobe involvement. Typical fibrous nodular type with or without a cavitary lesion was more frequent in the young, whereas pneumonia or a mass like lesion were more frequent in the elderly (p<0.001).
In laboratory findings (Table 4), no differences were found between the two groups in terms of positive sputum AFB smear (57.5% vs. 57.1%, p=0.952) or culture (74.4% vs. 70.6%, p=0.679), and complete blood counts showed no significant differences between mean leukocyte counts or the incidences of leukocytosis. However, the erythrocyte sedimentation rate was higher in the elderly (p=0.010).
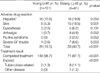
The following analysis was performed using the data of the 232 pulmonary TB patients who completed anti-TB medication at our hospital. Results are shown in Table 5. The most commonly observed side effects were liver toxicity and skin side effects in both groups. The frequency of skin side effects was statistically higher in the elderly. However, although the frequencies of drug-induced hepatitis, neurotoxicity, gastrointestinal troubles, arthralgia, and flu-like syndrome were somewhat higher in the elderly, they were without significance. The number of patients who experienced a drug adverse reaction was significantly higher in the elderly (p<0.001). TB related mortality occurred in 2 young patients and in 9 elderly. One elderly patient died due to a cerebral infarction during treatment. And thus, mortalities due to tuberculosis in the young and elderly were significantly different (p<0.001).
This study showed that symptoms like hemoptysis and a febrile sense occured more frequently in the young, whereas nonspecific symptoms like anorexia, weakness, weight loss and mental change occured more frequently in elderly pulmonary TB patients. Though the young patients complained of a febrile sense more frequently, no significant difference was observed between the two groups in terms of body temperature measures >37.5℃. This apparent anomaly may be due to a reduced perception of fever in the elderly group. The above results agree with those of others (6, 7), who found more classic respiratory symptoms in younger populations. Van den Brande et al. (15) also reported similar results, though they found that hemoptysis occurred equally in both groups. However, Umeki (8) reported that weight loss is more prevalent in elderly patients, and that more specific pulmonary symptoms such as hemoptysis and sputum, occur equally in both groups. Differences in symptom frequencies between Umeki's study and the present study may be explained by earlier pulmonary TB detection by mass survey in the former study.
Several factors may predispose the reactivation of dormant lesions in TB. These include insulin-dependent diabetes mellitus, poor nutrition, long-term corticosteroid therapy, other debilitating diseases, smoking, alcohol abuse, and waning cell-mediated immunity (4). Our study also supported the role of a reduced immune function in the development of pulmonary TB both in the young and elderly. A considerable number of patients in both groups had underlying disease, though the elderly were found to be more likely to have underlying disease. Diabetes mellitus and liver disease were the major underlying illness in both groups in the present study. In particular, the elderly had significantly higher frequencies of cardiovascular and chronic lung diseases, including pneumoconiosis, whereas the young had a significantly higher frequency of liver disease, suggesting the influence of alcoholism. These results correspond to those of Alvarez et al. (6) and Van den Brande (15) but contrast with those of Katz et al. (17) and Umeki (8), who found that malignancies and immunosuppressive drug intakes were higher in the elderly. This difference between studies may be due to a higher prevalence of TB in Korea.
There had been much debate concerning the atypical radiographic findings of TB in the elderly. Some have reported no major differences in radiologic features (18, 19), while others have reported a higher involvement of the middle and lower lung fields in the elderly (8, 9), whereas the present study shows significantly higher frequencies of isolated mid- and lower lung involvements in the elderly. The radiographic appearances were also different in these two age groups. Our findings are consistent with those of Perez (10) and Chan (11) in this respect.
Our results highlight the importance of sputum AFB smear/culture for the diagnosis of TB in the elderly. A positive sputum AFB smear was obtained in 57.1% of elderly and in 57.5% of young TB patients, and a positive AFB culture was obtained in 70.6% of the elderly and in 74.4% of the young, neither of which was significantly different. Moreover, these results compare well with other reports (7, 18, 21). Although Morris (22) previously suggested that AFB smears are not sensitive enough to diagnose non-cavitating tuberculosis in the elderly, many studies have reported that sputum AFB tests are powerful tools for the diagnosis of pulmonary TB in the elderly (4, 23). In a study by Mackay and Cole (24), sputum AFB smears yielded positive results in 45% patients with pulmonary TB, and sputum cultures were positive in 53% of elderly patients. Dahmash et al. (21) reported the detection of AFB in expectorated sputum specimens in 62.5% of patients. The reason for the somewhat higher sputum AFB detection rate of the present study is presumed to be due to patient population bias. Our hospital is a municipal hospital and many patients frequently visit physicians after the disease has progressed to an advanced stage due to a poor socioeconomic status. Thus in the present study, there is a possibility that the higher sputum AFB detection rate reflected a more advanced disease stage. The low incidence of asymptomatic patients in our study population supports this possibility.
Recently, Patel et al. (25) reported the usefulness of fiberoptic bronchoscopy in the diagnosis of TB. Fiberoptic bronchoscopy may be helpful in some elderly patients who are suspected of having TB, but who cannot expectorate adequate sputum. In the present study, only selected patients received a bronchoscopic examination, and a more aggressive bronchoscopic examination may well have revealed an advantage.
The appearance of adverse drug reactions is important when determining the effectiveness of anti-TB therapy. It has been suggested that adverse reactions to anti-TB drugs are more likely in the elderly (12, 13, 26). In the present study, the elderly did not tolerate drugs as well as the young, and experienced higher frequencies of adverse reactions. The most frequent side effects were drug-induced hepatitis and skin side effects. The incidence of reported anti-TB drug-induced hepatitis has been reported to show wide variations, which appear to be dependent on the definition of hepatotoxicity used (27-29). However, the majority of studies show that the elderly are more susceptible to anti-TB drug induced hepatotoxicity (12, 13). Using a similar definition to that used in the present study (i.e., serum transaminase >3×the normal upper limit), Fernandez-Villar et al. (30) found an 18.2% incidence of hepatotoxicity in the risk factor group (advanced age, chronic liver disease, abuse of alcohol, and others), and van den Brande et al. (31) a 22% incidence of hepatotoxicity (transaminase increase >5 times the basal level) in elderly TB patients. Sharma et al. (29) also reported a 16.2% drug-induced hepatotoxicity level in the elderly. Recently Yee et al. (13) reported that serious drug side effects, especially hepatitis and rash, is highest for pyrazinamide, and that this is associated with a female sex, an older age, birth in Asia, and HIV infection. Though we now discontinue pyrazinamide after 2 month of anti-TB medication, pyrazinamide was prescribed during the study period if it was tolerated for the entire treatment period due to the fear of drug resistance. This may partly explain the somewhat high incidence of drug-induced hepatitis observed in the present study.
Several have reported (6, 14, 24) higher TB related mortalities in elderly patients. In the present study, all young pulmonary TB patients survived except two, whereas 9 (11.1%) of the elderly patients died of TB. Some have even reported mortality rates as high as 20 to 40% in elderly TB patients (21). In the present study, differences in mortality might be partly explained by the exclusion of miliary TB. Our results confirm that mortality due to pulmonary TB is significantly higher in the elderly than in the young.
In conclusion, this study showed that elderly patients with pulmonary TB are more likely to present with non-specific symptoms and atypical radiographic findings. Moreover, we found a higher frequency of underlying disease, a higher incidence of adverse drug reactions, and higher TB-related mortality in elderly TB patients. However, no difference was observed between young and old patients with respect to sputum AFB detection rates.
Figures and Tables
Table 2
Presenting clinical symptoms and signs of the young and the elderly pulmonary tuberculosis patients
References
1. Ministry of Health and Social Affairs and Korean National Tuberculosis Association. Report on the tuberculosis prevalence survey in Korea 1965.
2. Ministry of Health and Welfare and Korean National Tuberculosis Association. Report on the seventh tuberculosis prevalence survey in Korea 1995.
5. Perez-Guzman C, Vargas MH, Torres-Cruz A, Villarreal-Velarde H. Does aging modify pulmonary tuberculosis? A meta-analytical review. Chest. 1999. 116:961–967.
7. Korzeniewska-Kosela M, Krysl J, Muller N, Black W, Allen E, Fitz-Gerald JM. Tuberculosis in young adults and the elderly. A prospective comparison study. Chest. 1994. 106:28–32.
8. Umeki S. Comparison of younger and elderly patients with pulmonary tuberculosis. Respiration. 1989. 55:75–83.

9. Liaw YS, Yang PC, Yu CJ, Wu ZG, Chang DB, Lee LN, Kuo SH, Luh KT. Clinical spectrum of tuberculosis in older patients. J Am Geriatr Soc. 1995. 43:256–260.

10. Perez-Guzman C, Torres-Cruz A, Villarreal-Velarde H, Vargas MH. Progressive age-related changes in pulmonary tuberculosis images and the effect of diabetes. Am J Respir Crit Care Med. 2000. 162:1738–1740.

11. Chan CH, Woo J, Or KK, Chan RC, Cheung W. The effect of age on the presentation of patients with tuberculosis. Tuber Lung Dis. 1995. 76:290–294.

12. Schaberg T, Rebhan K, Lode H. Risk factors for side-effects of isoniazid, rifampin and pyrazinamide in patients hospitalized for pulmonary tuberculosis. Eur Respir J. 1996. 9:2026–2030.

13. Yee D, Valiquette C, Pelletier M, Parisien I, Rocher I, Menzies D. Incidence of serious side effects from first-line antituberculosis drugs among patients treated for active tuberculosis. Am J Respir Crit Care Med. 2003. 167:1472–1477.

14. Counsell SR, Tan JS, Dittus RS. Unsuspected pulmonary tuberculosis in a community teaching hospital. Arch Intern Med. 1989. 149:1274–1278.

15. Van den Brande P, Vijgen J, Demedts M. Clinical spectrum of pulmonary tuberculosis in older patients: comparison with younger patients. J Gerontol. 1991. 46:M204–M209.

16. Morris CD. Pulmonary tuberculosis in the elderly: a different disease? Thorax. 1990. 45:912–913.

17. Katz I, Rosenthal T, Michaeli D. Undiagnosed tuberculosis in hospitalized patients. Chest. 1985. 87:770–774.

18. Rocha M, Pereira S, Barros H, Seabra J. Does pulmonary tuberculosis change with aging? Int J Tuberc Lung Dis. 1997. 1:147–151.
19. Van den Brande P, Vernies T, Verwerft J, Van Bleyenber R, Vanhoenacker F, Demedts M. Impact of age and radiographic presentation on the presumptive diagnosis of pulmonary tuberculosis. Respir Med. 2002. 96:979–983.

20. Lee JH, Hwangbo B, Yoo CG, Lee CT, Han SK, Shim YS, Chung HS. Clinical features of pulmonary tuberculosis in the elderly. Tuberc Respir Dis. 2001. 51:334–345.

21. Dahmash NS, Fayed DF, Chowdhury MN, Arora SC. Diagnostic challenge of tuberculosis of the elderly in hospital: experience at a university hospital in Saudi Arabia. J Infect. 1995. 31:93–97.

22. Morris CD. Sputum examination in the screening and diagnosis of pulmonary tuberculosis in the elderly. Q J Med. 1991. 81:999–1004.

23. Grzybowski S, Allen EA, Black WA, Chao CW, Enarson DA, Isaac-Renton JL, Peck SH, Xie HJ. Inner-city survey for tuberculosis: evaluation of diagnostic methods. Am Rev Respir Dis. 1987. 135:1311–1315.
24. Mackay AD, Cole RB. The problems of tuberculosis in the elderly. Q J Med. 1984. 53:497–510.
25. Patel YR, Mehta JB, Harvill L, Gateley K. Flexible bronchoscopy as a diagnostic tool in the evaluation of pulmonary tuberculosis in an elderly population. J Am Geriatr Soc. 1993. 41:629–632.

26. Teale C, Goldman JM, Pearson SB. The association of age with the presentation and outcome of tuberculosis: a five-year survey. Age Ageing. 1993. 22:289–293.

27. Ungo JR, Jones D, Ashkin D, Hollander ES, Bernstein D, Albanese AP, Pitchenik AE. Antituberculosis drug-induced hepatotoxicity. Am J Respir Crit Care Med. 1998. 157:1871–1876.

28. Blumberg HM, Barman WJ, Chaisson RE, Daley CL, Etkind SC, Friedman LN, Fujiwara P, Grzemska M, Hopewell PC, Iseman MD, Jasemer RM, Koppaka V, Menzies RI, O'Brien RJ, Reves RR, Rcichman LB, Simone PM, Starke JR, Verhon AA. American Thoracic Society, Centers for Disease Control and Prevention and the Infectious Diseases Society. American Thoraic Society/Centers for Disease Control and Prevention/Infections Diseases Society of American: treatment of tuberculosis. Am J Respir Crit Care Med. 2003. 167:603–662.
29. Sharma SK, Balamurugan A, Saha PK, Pandey RM, Mehra NK. Evaluation of clinical and immunogenetic risk factors for the development of hepatotoxicity during antituberculosis treatment. Am J Respir Crit Care Med. 2002. 166:916–919.

30. Fernandez-Villar A, Sopena B, Fernandez-Villar J, Vazquez-Gallardo R, Ulloa F, Leiro V, Mosteiro M, Pineiro L. The influence of risk factors on the severity of anti-tuberculosis drug-induced hepatotoxicity. Int J Tuberc Lung Dis. 2004. 8:1499–1505.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download