Abstract
p63 is a recently described p53 homologue. It is involved in survival and differentiation of reserve/stem cells in epithelia. To obtain new insights into the role of p63 in malignant lymphomas (MLs), immunohistochemical staining for p63 and p53 was performed in 126 cases of MLs. p63 was expressed in 38 cases of MLs (30.2%) including 32/61 cases (52.5%) of diffuse large B-cell lymphoma (DLBCL), 1/8 cases (12.5%) of precursor T-lymphoblastic lymphoma (T-LBL), 4/14 cases (28.6%) of follicular lymphoma, 1/6 cases (16.7%) of T/NK cell lymphoma. Among p63 positive cases, p63 was strongly expressed in 15/32 cases of DLBCL and 1/1 case of T-LBL. p63 was not expressed in mantle cell lymphomas, peripheral T-cell lymphomas, marginal zone B-cell lymphomas, plasma cell myelomas and Hodgkin's lymphomas. p63 was coexpressed with p53 in 18/38 p63 positive cases in which only 4 cases were strongly coexpressed. All p63+/p53+ cases were DLBCL. p63 overexpression (above 30%) cases showed significant poor survival (p=0.0228) in DLBCL. However, there was no statistically significant correlation between p63 expression and IPI score on Multivariate analysis. We could speculate that p63 could act indirectly as an oncogene by inhibiting p53 functions. Stage of differentiation of neoplastic lymphocytes appears to have a correlation with p63 expression in MLs.
p63 is a member of the p53 tumor-suppressor gene family with structural homology to p53, but one that, from a functional point of view, shows both similarities and differences from p53 (1-5). In fact, the p63 gene transcript undergoes multiple alternative splicing and, in addition, can be transcribed from two different promoters, resulting in the generation of a variety of p63 isoforms, including three transactivating (TA-p63, α-β-γ) and three amino terminal-truncated proteins (ΔN-p63, α-β-γ) (1, 2, 5). Interestingly, these different molecular species can exert contrasting effects on the same molecular targets, interfering with p53 functions. TA-p63 molecules (especially TA-p63γ) have functions similar to p53 in inducing cell-cycle arrest and apoptosis. However, ΔN-p63 isoforms (especially theΔN-p63α isoform) act as a dominant-negative factor, inhibiting transcription activation by both p53 and TA-p63 isoforms (1, 2, 6). When abnormally over-expressed as a result of gene amplification, these latter p63 isoforms are thought to behave as oncogenic molecules (1, 5, 7-9).
Recently, p63 has been proposed to be a specific marker of precursor/stem cells in many epithelial tissues and to represent a candidate marker for exploring thymic stem cells (5, 10-12). The fine-tuning of different p63 isoforms in the basal and differentiating compartments is necessary to maintain the regenerative quality of epithelial stem cells, as well as the regulation of epidermal mesenchyme interactions, replicative senescence, and angiogenesis (13-15). Therefore p63 is essential during embryonic life for the correct development of limb craniofacial, epithelial differentiation and proliferation rather than tumor suppression (16). However, the final designation of p63 as an oncogene or a tumor suppressor gene is still under debate (6). In contrast, p53 is a well-known tumor suppressor gene located on chromosome 17p13.1 and encoding a nuclear phosphoprotein of 53 kDa (17). It is believed to induce cell cycle arrest in the presence of damaged DNA, finally leading cells to apoptosis. Regarding malignant lymphomas (MLs), p53 overexpression has been found in 33.3% (18) and 41.9% (19) of cases and has been related to disease-specific survival (18). Recently, alterations and loss of p63 expression in advanced stages of human bladder carcinoma have been described (20-22) but their clinical significance still has to be defined. Information regarding p63 expression in malignant lymphoma (ML) is scanty, and few data are available regarding ML. Starting from these grounds, we have investigated the expression of p63 in reactive hyperplasias (RHs) and in a series of MLs using immunohistochemistry.
The study group consisted of 10 RHs and 126 previously untreated MLs, classified according to World Health Organization (WHO) criteria (23). All tissue samples were fixed in 10% formalin and paraffin embedded following routine procedures. The ML series included: 61 diffuse large B-cell lymphoma (DLBCL), 14 follicular lymphoma (FL), 22 peripheral T-cell lymphoma (PTCL), 8 precursor T-lymphoblastic lymphoma (T-LBL), 6 T/NK cell lymphoma (T/NKL), 3 mantle cell lymphoma (MCL), 3 Burkitt's lymphoma (BL), 5 Hodgkin's lymphoma (HL), 2 marginal zone B-cell lymphoma (MZBCL), 1 primary mediastinal large B-cell lymphoma (PMLBCL), 1 plasmacytoma. Control tissues included tonsil obtained from children during tonsillectomy. Tissue microarray (TMA) blocks were created from 72 cases of MLs and 10 cases of RHs.
The antibody panel for characterizing lymphomas included CD20 (clone L26; Dako, Glostrup, Denmark), CD3 (clone PS1; Novocastra, Newcastle, U.K.), CD45RO (Immunotech, Marseille, France), terminal-deoxynucleotidyl transferase (TdT, rabbit antibody; Dako), CD56 (Dako), CD5 (clone 4C7; Novocastra), CD10 (Dako), cyclin D1 (Novocastra), bcl2 (Dako), CD15 (Immunotech) and CD30 (Dako). For the TMA, hematoxylin and eosin-stained sections from each paraffin-embedded, formalin-fixed block were used to define diagnostic areas, and 2 to 5 (average 4) random, representative 0.6-mm cores were obtained from each case and inserted in a grid pattern into a recipient paraffin block using a tissue arrayer (Beecher Instruments, Silver Spring, MD, U.S.A.). Sections (5 µm) were cut from each TMA and paraffin blocks and mounted on adhesive-treated glass slides, rehydrated and treated for antigen retrieval (0.01 M, citrate buffer, pH 6.5, microwaved three times at 750 W for 10 min, and once for 10 min at 600 W). Immunostaining was performed using the avidin-streptavidin-peroxidase technique (Biogenex, San-Ramon, CA, U.S.A.). Consecutive sections were analyzed using p63, p53 and Ki-67 specific antibodies. Anti-p63 (Ab-1, Oncogene Research Products, Boston, MA, U.S.A.), is a mouse monoclonal antibody (clone-4A4) corresponding to a region (amino acids 1-205 of ΔN-p63 isoforms) common to six isoforms of the p63 molecule. The p53 antibody (Novocastra) is a DO-7 monoclonal antibody, which specifically detects human wild type and mutant p53. The MIB-1 antibody (Biogenex) is produced by immunized mice against recombinant Ki-67 gene products. The slides were counterstained with hematoxylin.
Only nuclear staining above 5% was interpreted as positive for p63 and p53 expression. Immunostaining results for p63, p53, and Ki-67 were semiquantitatively evaluated according to the percentage of positive tumor cells in each case. Staining intensity was graded as + (weak), ++ (moderate), and +++ (strong).
The Kaplan-Meier method was used to estimate overall survival distributions. DLBCL cases with p63 and p53 overexpression above 30% were included on survival analysis. Overall survival was calculated as the time from diagnosis to the date of death or last contact. Patients who were alive at last contact were treated as censored for overall survival analysis. The log-rank test was used to compare the clinical characteristics between the subgroups. Univariate and multivariate analysis was performed using the Cox regression method. Stepwise selection was used to determine the variables that were independent predictors of overall survival. SPSS 11.0 Statistical soft ware (U.S.A.) program was used for the data analysis.
Nuclear p63 expression was confined to basal components of squamous epithelium in tonsil. A few scattered p63 immunoreactive nuclei were observed within germinal centers. p53 and Ki-67 were randomly positive in nuclei of basal cells. The basal cells did not coexpress p63 and p53.
There was 3 Castleman's disease, 1 progressive transformation of germinal centers, and 6 reactive follicular hyperplasias. p63 and p53 were not expressed in RHs (10 cases). Ki-67 was strongly positive for activated germinal center cells and usually negative for parafollicular small lymphocytes.
There were 4 cases of mixed cellularity and 1 nodular sclerosis of HL. p63 was not expressed in 5 cases of HL. p53 was strongly expressed in Reed-Sternberg cells and its variants. p53 was not expressed in background lymphoid cells.
p63 was expressed in 38 cases of MLs studied (30.2%) including 32/61 cases (52.5%) of DLBCL, 1/8 cases (12.5%) of T-LBL, 4/14 cases (28.6%) of FL, 1/6 cases (16.7%) of T/NKL. Among p63 positive cases, p63 was diffusely and strongly expressed in 15/32 cases (46.9%) of DLBCL (Fig. 1) and 1/1 case of T-LBL (Fig. 2) when using 30% as cut off value. Remaining cases were focally and weakly expressed. p63 was not expressed in MCL (3 cases), PTCL (22cases), MZBCL (2 cases), plasmacytoma (1 case) and HL (5 cases).
CD10 was expressed in 10/52 cases (19.2%) of DLBCL when using 30% as cut off value. Among 10 cases of CD10 expression, p63 was detected in only one case (1/10, 10%). In contrast, p63 was expressed in 12/42 cases (28.6%) of CD10 negative DLBCL.
Using an arbitrary threshold of 5% positive staining, expression of p53 was detected in 50 of 119 cases (38.8%).
p53 was expressed in 27/60 DLBCL (45%), 2/8 T-LBL (25%), 8/21 PTCL (38.1%), 4/6 T/NKL (66.7%), 3/3 BL (100%), 1/13 FL (7.7%), 0/1 MZBCL (0%). There were significant correlations between p53 immunoreactivity and histologic subtypes of MLs. Diffuse strong positive immunoreactivity was the most constant finding in high grade MLs. Low grade lymphomas were p53 negative.
Among the 38 cases positive for p63, 14 cases coexpressed p53 (36.8%) when using 5% as cut off value. When using 30% as cut off value, 4/38 p63 positive cases (10.5%) coexpressed p53 strongly and diffusely. They were all DLBCL cases.
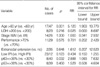
Univariate Cox proportional hazards regression analysis was performed according to following variables such as age, LDH, stage, patient's performance, extranodal extension, p63 and p53 positivity status, which are shown in Table 1. Age was the most significant factor followed by high p63 positivity. Other variables were not significant. Finally, multivariate Cox proportional hazards regression analysis according to significant variable was used (Table 2). Age was significant but there was no significance between international prognostic index and p63 expression.
Survival analysis was performed in 48 patients with a median observation period of 27 months. Cases with p63 overexpression above 30% showed significantly poor survival regardless of p53 expression (Fig. 3). On the other hand, p53 had no significance on survival analysis (Fig. 3). Survival analysis was also performed by dividing the study group with respect to p53. p53 negative cases were 48 and p53 positive cases were 8 in number. In p53 negative group, p63 positive cases had significantly poor survival but p53 positive group was too small in number (Fig. 4).
To our knowledge, this is the first study to analyze the immunoreactivity of p63 and p53 in a large number of ML specimens and to correlate p63 and p53 immunoreactivity with clinical follow-up. More recently, MLs were described as p63 immunoreactive in a survey study on human tumors (23), but relationship between p63 and p53 immunostaining in respect to patient's prognosis with ML has not yet been reported. Di Como et al. (24) examined p63 expression profiles in a number of non-Hodgkin's B-cell lymphomas, including those classified as CLL/SLL, FL, DLBCL, anaplastic largecell lymphoma, MCL, and MZBCL. They observed diffuse to intense staining in DLBCL and FL (24). Furthermore, in FL, the strongest staining was observed in grade 3 cases in the larger neoplastic cells. Higher levels of p63 protein expression were found in tumor lymphocytes compared with normal lymphoid tissues by RT-PCR (24). Chilosi et al. (25) reported that T-cell precursor lymphomas did not express p63, whereas 7 of 8 cases of PMLBCL expressed TA-p63α. But details on ML subtypes and discussions on the significance of p63 overexpression in MLs were not provided (25). In humans, heterozygous germline p63 mutations have been described in EEC syndrome, in which a single case has been described with thymic hypoplasia (26) although no lymphoid or thymic abnormalities have been described in p63-null mice (16, 27). There is also another case study examined a sporadic incident of EEC syndrome (ectrodactyly ectodermal dysplasia-clefting syndrome) of complete form of the anomaly with late onset of non-Hodgkin's lymphoma (28). Interestingly, the non-Hodgkin's lymphoma was of the diffuse large-cell type, where we observed intense p63 immunoreactivity. Our results of study are consistent with those of previous studies (24, 28). In this study p63 was expressed in 38 cases of MLs studied (30.2%) including 32/61 cases (52.5%) of DLBCL, 1/8 cases (12.5%) of T-LBL, 4/14 cases (28.6%) of FL, 1/6 cases (16.7%) of T/NKL. Among p63 positive cases, p63 was diffusely and strongly expressed in 15/32 cases of DLBCL and 1/1 case of T-LBL. Remaining cases were focally and weakly expressed. p63 was not expressed in MCL, PTCL, MZBCL, plasmacytoma and HL. p63 and p53 were not expressed in RHs.
Recently, DLBCL tends to be divided according to CD10 immunoreactivity. So, we also analyzed p63 expression according to CD10 immunoreactivity in 52 DLBCL cases. In the present study, CD10 was expressed in 10/52 cases (19.2%) of DLBCL. Among 10 cases of CD10 expression, p63 was detected in only one case (1/10, 10%). In contrast, p63 was expressed in 12/42 cases (28.6%) of CD10 negative DLBCL. Although there is no statistical significance between p63 and CD10 expression, p63 showed a tendency to increase its expression in CD10 negative DLBCL comparing with in CD10 positive DLBCL.
There are no clear explanations why p63 is overexpressed in DLBCL. Yang et al. (1) speculated that because p63 lies close to the translocation break point found in some DLBCLs, genomic instability in this area may lead to the dysregulation of p63. However, this does not explain why TA isoforms are predominant in the small group of MLs by use of RT-PCR (24).
In contrast to p53, a protypical tumor suppressor gene, somatic mutations of the TP 63 gene are very rare, whereas germline mutations in TP 63 have been reported for patients with limb mammary syndrome, split-hand/split-foot malformation, ankyloblepharon-ectodermal dysplasia-clefting syndrome, and EEC syndrome (29-32). Therefore, it might be that alterations of TP 63 are epigenetic in nature. A number of studies have investigated the role of p63 in neoplastic transformation and tumor progression including squamous cell carcinomas (SCCs) of different organs (7, 8, 33, 34), invasive ductal carcinomas of the breast (35), transitional cell carcinomas (6, 36), and thymomas (25). SCCs from different organs express high levels of ΔN-p63 (7, 8, 34). The p63 gene may be the target of 3q27-29 gains common in SCC (1, 8).
In this context, we might speculate that when certain p63 isoforms are expressed, such as dominant-negative ΔN-p63, they could bind to and inhibit transactivation by p53 and TA-p63 (1). Alternatively, these ΔN-p63 isoforms, by binding to specific promoter elements, could block the transcription of otherwise critical genes, such as those involved in the apoptotic response. Rather than inactivating tumor suppressor activities (e.g., p53), altered patterns of p63 expression could be driving the transcription of oncogenic proteins, such as hMDM2, a target reported for TA-p63γ (37, 38). Further studies, integrating mechanistic approaches, are needed to elucidate the role of p63 in human cancer.
Regarding the prognostic importance of p63 expression in various types of human carcinomas, the results are controversible. Some authors reported an inverse correlation between p63 overexpression and advanced tumor stage and poor prognosis (6, 36). In thymomas, p63 expression was not correlated with clinical aggressiveness (24, 25) although others have reported a correlation between p53 expression and malignancy in thymomas. In this study, p63 expression appears to be related to poor survival in DLBCL. However, as shown in previous study (36), multivariate analysis failed to prove either p53 or p63 as an independent prognostic parameter in this study. Age was the only stastically significant independent prognostic factor.
In conclusion, p63 was overexpressed in specific histologic types of MLs such as T-LBL and DLBCL. In FL, p63 was weakly expressed in small numbers. The number of cells containing p63 and their distribution tend to depend on the degree of differentiation of lymphocytes. p63 was rarely coexpressed with p53. p63 expression appears to be related to poor survival although it was not stastically significant on multivariate analysis. Therefore, we could speculate that p63 could act indirectly as an oncogene by inhibiting p53 functions. Stage of differentiation of neoplastic lymphocytes appears to have correlation with p63 expression in MLs. Molecular study regarding different p63 isoform expression and p63 mutation could contribute to understanding the heterogeneity of DLBCL and progression of ML.
Figures and Tables
Fig. 1
Histologic findings of a case of diffuse large B-cell lymphoma (DLBCL) (H&E stain, ×400) (A). The tumor cells show high Ki-67 index (B) and strong p63 expression (C) devoid of p53 expression (D).

Fig. 2
Histologic findings of a case of precursor T-lymphoblastic lymphoma (T-LBL) developing in a 15-yr-old boy (A). p63 is diffusely and strongly positive (B). In contrast, p53 is negative (C).

Fig. 3
Kaplan-Meier survival analysis in DLBCL according to p63 (A) and p53 expression (B). Cases with p63 overexpression above 30% show significantly poor survival regardless of p53 expression. On the other hand, cases with p53 overexpression above 30% show no significance on survival.

Fig. 4
Survival analysis of DLBCL cases with p63 overexpression above 30% according to p53 expression. In p53 negative group (less than 30%), cases with p63 overexpression above 30% show significant poor survival (A) but p53 positive group (more than 30%) is too small in number (B).

References
1. Yang A, Kaghad M, Wang Y, Gillett E, Fleming MD, Dotsch V, Andrews NC, Caput D, Mckeon F. p63, a p53 homolog at 3q27-29, encodes multiple products with transactivating, death-inducing, and dominant-negative activities. Mol Cell. 1998. 2:305–316.

4. Shimada A, Kato S, Enjo K, Osada M, Ikawa Y, Kohno K, Obinata M, Kanamaru R, Ikawa S, Ishioka C. The transcriptional activities of p53 and its homologue p51/p63: similarities and differences. Cancer Res. 1999. 59:2781–2786.
5. Yang A, Mckeon F. P63 and p73: p53 mimics, menaces and more. Nat Rev Mol Cell Biol. 2000. 1:199–207.

6. Urist MJ, Di Como CJ, Lu ML, Charytonowics E, Verbel D, Crum CP, Ince TA, Mckeon FD, Cordon-Cardo C. Loss of p63 expression is associated with tumor progression in bladder cancer. Am J Pathol. 2002. 161:1199–1206.

7. Crook T, Nicholls JM, Brooks L, O'Nions J, Allday MJ. High level expression of deltaN-p63: a mechanism for the inactivation of p53 in undifferentiated nasopharyngeal carcinoma (NPC). Oncogene. 2000. 19:3439–3444.
8. Hibi K, Trink B, Patturajan M, Westra WH, Caballero OL, Hill DE, Ratovitski EA, Jen J, Sidransky D. AIS is an oncogene amplified in squamous cell carcinoma. Proc Natl Acad Sci USA. 2000. 97:5462–5467.

9. Hibi K, Nakayama H, Taguchi M, Kasai Y, Ito K, Akiyama S, Nakao A. AIS overexpression in advanced esophageal cancer. Clin Cancer Res. 2001. 7:469–472.
10. Chilosi M, Doglioni C. Constitutive p63 expression in airway basal cells. A molecular target in diffuse lung diseases. Sarcoidosis Vasc Diffuse Lung Dis. 2001. 18:23–26.
11. Glickman JN, Yang A, Shahsafaei A, Mckeon F, Odze RD. Expression of p53-related protein p63 in the gastrointestinal tract and in esophageal metaplastic and neoplastic disorders. Hum Pathol. 2001. 32:1157–1165.

12. Pellegrini G, Dellambra E, Golisano O, Martinelli E, Fantozzi I, Bondanza S, Ponzin D, McKeon F, De Luca M. p63 identifies keratinocyte stem cells. Proc Natl Acad Sci USA. 2001. 98:3156–3161.

13. De Laurenzi V, Rossi A, Terrinoni A, Barcaroli D, Levrero M, Costanzo A, Knight RA, Guerrieri P, Melino G. p63 and p73 transactivate differentiation gene promoters in human keratinocytes. Biochem Biophys Res Commun. 2000. 273:342–346.

14. Djelloul S, Tarunina M, Barnouin K, Mackay A, Jat PS. Differential protein expression, DNA binding and interaction with SV40 large tumor antigen implicate the p63-family of proteins in replicative senescence. Oncogene. 2002. 21:981–989.
15. Senoo M, Matsumura Y, Habu S. TAp63 gamma (p51A) and ΔNp63-alpha (p73L), two major isoforms of the p63 gene, exert opposite effects on the vascular endothelial growth factor (VEGF) gene expression. Oncogene. 2002. 21:2455–2465.
16. Yang A, Schweitzer R, Sun D, Kaghad M, Walker N, Bronson RT, Tabin C, Sharpe A, Caput D, Crum C, Mckeon F. p63 is essential for regenerative proliferation in limb, craniofacial, and epithelial development. Nature. 1999. 398:714–718.

17. Levin AJ, Momand J, Finlay CA. The p53 tumor suppressor gene. Nature. 1991. 351:453–456.
18. Ahn MJ, Kim H, Kim IS, Park JK, Ki MR, Park CK. P53 protein expression and its prognostic importance in patients with nodal non-Hodgkin's lymphoma. J Korean Med Sci. 2000. 15:59–64.

19. Park CK, Lee JD. Immunohistochemical and SSCP analysis of p53 in malignant lymphomas. J Korean Med Sci. 1998. 13:361–368.

20. Hall PA, Campbell SJ, O'Neill M, Royston DJ, Nylander K, Carey FA, Kernohan NM. Expression of the p53 homologue p63alpha and deltaNp63alpha in normal and neoplastic cells. Carcinogenesis. 2000. 21:153–160.
21. Park BJ, Lee SJ, Kim JI, Lee CH, Chang SG, Park JH, Chi SG. Frequent alteration of p63 expression in human primary bladder carcinomas. Cancer Res. 2000. 60:3370–3374.
22. Koga F, Kawakami S, Kumagai J, Takizawa T, Ando N, Arai G, Kageyama T, Kihara L. Impaired Delta Np63 expression associates with reduced beta catenin and aggressive phenotypes of urothelial neoplasms. Br J Cancer. 2003. 88:740–747.
23. Jaffe ES, Harris NL, Stein H, Vardiman JW. Tumors of hematopoietic and lymphoid tissues, Pathology & Genetics, World Health Organization Classification of Tumors. 2001. Lyon IARC Press;127–130.
24. Di Como CJ, Urist MJ, Babayan I, Drobnjak M, Hedvat CV, Teruya-Feldstein J, Pohar K, Hoos A, Cordon-Cardo C. p63 expression profiles in human normal and tumor tissues. Clin Cancer Res. 2002. 8:494–501.
25. Chilosi M, Zamo A, Brighenti A, Malpeli G, Montagna L, Piccoli P, Pedron S, Lestani M, Inghirami G, Scarpa A, Doglioni C, Menestrina F. Constitutive expression of ΔNp63α isoform in human thymus and thymic epithelial tumors. Virchows Arch. 2003. 443:175–183.
26. Frick H, Munger DM, Fauchere JC, Stallmach T. Hypoplastic thymus and T-cell reduction in EECUT syndrome. Am J Med Genet. 1997. 69:65–68.

27. Mills AA, Zheng B, Wang XJ, Vogel H, Roop DR, Bradley A. p63 is a p53 homologue required for limb and epidermal morphogenesis. Nature. 1999. 398:708–713.

28. Ogutcen-Toller M, Gulen O, Okten G, Elbistan M. Non-Hodgkin's lymphoma in a patient with ectrodactyly ectodermal dysplasia-clefting syndrome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000. 90:124–125.
29. Celli J, Duijf P, Hamel BC, Bamshad M, Kramer B, Smits AP, Newbury-Ecob R, Hennekam RC, Van Buggenhout G, van Haeringen A, Woods CG, van Essen AJ, de Waal R, Vriend G, Haber DA, Yang A, McKeon F, Brunner HG, van Bokhoven H. Heterozygous germline mutations in the p53 homolog p63 are the cause of EEC syndrome. Cell. 1999. 99:143–153.

30. Ianakiev P, Kilpatrick MW, Toudjarska I, Basel D, Beighton P, Tsipouras P. Split-hand/split-foot malformation is caused by mutations in the p63 gene on 3q27. Am J Hum Genet. 2000. 67:59–66.

31. McGrath JA, Duijf PH, Doetsch V, Irvine AD, de Waal R, Vanmolkot KR, Wessagowit V, Kelly A, Atherton DJ, Griffiths WA, Orlow SJ, van Haeringen A, Ausems MG, Yang A, McKeon F, Bamshad MA, Brunner HG, Hamel BC, van Bokhoven H. Hay-Wells syndrome is caused by heterozygous missense mutations in the SAM domain of p63. Hum Mol Genet. 2001. 10:221–229.

32. Wessagowit V, Mellerio JE, Pembroke AC, McGrath JA. Heterozygous germline missense mutation in the p63 gene underlying EEC syndrome. Clin Exp Dermatol. 2000. 25:441–443.

33. Parsa R, Yang A, Mckeon F, Green H. Association of p63 with proliferative potential in normal and neoplastic human keratinocytes. J Invest Dermatol. 1999. 113:1099–1105.

34. Yamaguchi K, Wu L, Caballero OL, Hibi K, Trink B, Resto V, Cairns P, Okami K, Koon WM, Sidransky D, Jen J. Frequent gain of the p40/p51/p63 gene locus in primary head and neck squamous cell carcinoma. Int J Cancer. 2000. 86:684–689.
35. Ribeiro-Silva A, Zambelli Ramalho LN, Britto Garcia S, Zucoloto S. The relationship between p63 and p53 expression in normal and neoplastic breast tissue. Arch Pathol Lab Med. 2003. 127:336–340.

36. Zigeuner R, Tsybrovskyy O, Ratschek M, Rehak P, Lipsky K, Langner C. Prognostic impact of p63 and p53 expression in upper urinary tract transitional cell carcinoma. Urology. 2004. 63:1079–1083.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download