Abstract
To obtain the low birth weight (LBW) rate, the very low birth weight (VLBW) rate, and gestational age (GA)-specific birth weight distribution based on a large population in Korea, we collected and analyzed the birth data of 108,486 live births with GA greater than 23 weeks for 1 yr from 1 January to 31 December 2001, from 75 hospitals and clinics located in Korea. These data included birth weight, GA, gender of the infants, delivery type, maternal age, and the presence of multiple pregnancy. The mean birth weight and GA of a crude population are 3,188±518 g and 38.7±2.1 weeks, respectively. The LBW and the VLBW rates are 7.2% and 1.4%, respectively. The preterm birth rate (less than 37 completed weeks of gestation) is 8.4% and the very preterm birth rate (less than 32 completed weeks of gestation) is 0.7%. The mean birth weights for female infants, multiple births, and births delivered by cesarean section were lower than those for male, singletons, and births delivered vaginally. The risk of delivering LBW or VLBW infant was higher for the teenagers and the older women (aged 35 yr and more). We have also obtained the percentile distribution of GA-specific birth weight in infants over 23 weeks of gestation.
Birth weight is known to be the most important determining factor of neonatal mortality (1). The infant morbidity or mortality of a community or a country is reported to be closely associated with the distribution of birth weight in that population. An increase in low birth weight (LBW) infants or premature infants causes an increase in neonatal morbidity and mortality and infant mortality (2-5).
Although there have been several studies on neonatal birth weight distribution and very low birth weight (VLBW) infant survival rates in Korea (6-17), the populations in these studies are small or limited to general hospitals and university hospitals. In effect, there is a shortage of large-scale or nation-wide studies of birth weight or other factors associated with infant morbidity and mortality in Korea.
Therefore the authors have selected as big a population as possible in Korea and collected data on birth weight and the perinatal factors, to find out the incidence of LBW infants and VLBW infants, and also the gestational age (GA)-specific birth weight distribution.
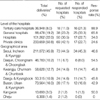
Data was collected on 118,538 live-born infants who were born in Korea between 1 January 2001 and 31 December 2001 at a GA over 23 weeks. Copies of the delivery room records were requested to 164 hospitals including general hospitals and obstetric private clinics where more than 1,000 deliveries were recorded per year as well as university hospitals in all parts of the country. The delivery records were received from 75 hospitals across the nation including 16 of 18 tertiary care hospitals (88.9%), 25 of 38 general hospitals (65.8%) and 17 of 50 hospitals (34%) and 17 of 69 obstetric clinics (24.6%) (Table 1). The registers of all live-born infants who were born after 23 weeks of GA were collected through mail. Birth weight, GA, sex, mode of delivery, maternal age and the presence of multiple pregnancy of the data were entered into the database.
Of the data collected, 7,883 infants with uncertain birth weight or GA were excluded. After obtaining the distribution of GA-specific birth weight, the data above the 99th percentile or below the 1st percentile were excluded to remove typing errors during database input. However, all the definite typing errors such as '6,500 g for 24 weeks of gestation' could not be eliminated. Therefore 2,169 infants, whose birth weights were over the 95th percentile or under the 5th percentile for GA, were excluded to eliminate typing errors. The total number of neonates included in this study was 108,486.
To obtain the distribution of birth weight, first the frequency of LBW infants (birth weight <2,500 g) and VLBW infants (birth weight <1,500 g) were determined, then percentiles of GA-specific birth weight were deduced. To eliminate risk factors that could affect birth weight, only singleton infants born to mothers who were between 20 and 34 yr of age were selected. In addition, to compensate for errors in estimating GA by last menstrual period, using the same method used by Williams et al. (18), we divided the group by birth weight into 250 g intervals and excluded those with GA above the 99th percentile or below the 1st percentile for each group. Consequently the GA-specific percentile distribution of birth weight was obtained from 77,192 infants.
Data were expressed as the mean±standard deviation, 95% confidence interval and proportion (%). Student t-test was used to compare the means of each group and chi-square test to compare incidence or proportion. Statistical procedures were performed using SPSS ver. 10.0 (SPSS, Inc., Chicago, IL). A p-value below 0.05 was considered statistically significant.
Mean birth weight and mean GA for the entire groups were 3,188±518 g and 38.7±2.1 weeks respectively. The LBW rate and the VLBW rate were 7.2% and 1.4% respectively, and the birth rate of premature infants under 37 weeks of GA was 8.4%. Birth rates of extremely low birth weight (ELBW) infants under 1,000 g and premature infants under 32 weeks of GA were 0.7% and 1.7% respectively. Postmature rate over 42 weeks of GA was 0.9% (Table 2).
Of all the subjects in the study, 52.0% was male, 2.6% was multiple pregnancies, and 31.4% was delivered via cesarean section. Maternal age distribution was as follows: 1.4% under 20 yr of age, 73.9% between 20 and 34, 7.3% between 35 and 39, 1.4% over 40. Birth weight of male infants was heavier than female infants by 85 g, twins were lighter than singletons by 829 g, and infants delivered by cesarean section were 99 g lighter than those delivered vaginally. Birth weights of infants grouped by maternal age were significantly different between groups. Infants born to mothers between 20 and 34 yr of age were heavier than those with maternal age below 20 yr or over 35 yr of age (Table 3).
Although there was no difference in VLBW rate between male and female infants, LBW rate was higher for female infants by 0.9% (p<0.001). LBW rate, VLBW rate, ELBW rate of twins were 52.9%, 6.9%, and 2.5%, which were significantly higher than those of singletons, 5.9%, 1.3%, and 0.6% respectively, and these rates were even higher in higher-number multiple pregnancies than those of singletons (p<0.001). LBW rate and VLBW rate in infants with cesarean delivery were more than two times higher than those of infants delivered vaginally (11.0% vs. 4.7%, and 1.8% vs. 0.8%, respectively). In infants born to teenage mothers, LBW, VLBW, ELBW rates were 18.6%, 3.2%, 1.7%, respectively, which were about two times higher than those of infants with maternal age between 20 and 34 yr, 7.2%, 1.4%, and 0.7% (p<0.001). Infants whose mothers aged 35 yr and more also showed higher LBW, VLBW, ELBW rates than those of infants with maternal age between 20 and 34 yr (p<0.001) (Table 4).
GA-specific birth weight for GA between 23 weeks and 42 weeks, are shown on Table 5.
Neonatal morbidity and mortality are affected by the quality of perinatal care (1, 2, 19). Neonatal mortality rate was markedly reduced by the progress of neonatal intensive care in last 2 decades in Korea (19). None the less, the lower birth weight newborn infants showed, the lower possibility of survival they had (2-4, 19). A rise of LBW rate in a country increases neonatal mortality and also infant mortality rate, which is an important indicator of the level of public health in the country (2). Therefore the first step to reduce infant or neonatal mortality rate is the reduction of LBW rate, and basic data on LBW rate and VLBW rate must be gathered. Unfortunately, nationwide governmental surveillance of birth rate and neonatal mortality is not adequate in Korea. There is insufficient data on perinatal indices, including birth weight. In general, the LBW and the VLBW rates are estimated to be 6-8% and 1.0-1.5%, respectively in Korea (9). In the most recent study on birth weight and LBW rate in Korea in 1996, data were gathered nationwide from 64 hospitals and the results were: LBW rate 9.8%, VLBW rate 1.7%, ELBW rate 0.5% (8). The results from that study could show higher LBW rate and VLBW rate than the real rates, since the survey was conducted mainly in general hospitals or university hospitals where proportion of high risk pregnancy was probably higher than that of private obstetric clinics (8).
The number of the newborn infants included in this study was 108,486. This constituted 19.5% of the 557,228 infants born in 2001 according to Korean National Statistical Office report (20). Although it is also insufficient to represent the trends in the whole country of Korea, this study could reflect the national trend more accurately than the previous studies, because private obstetric clinics were also included. The LBW rate and the VLBW rate, according to the Korean National Statistical Office report (20), were 3.55% and 0.24% in 2000 and 3.59% and 0.36% in 2001, which differ considerably from the results of our study and the National Vital Statistics Report of the United States (21, 22). This discrepancy can be caused by two factors, one of which may be the omission of VLBW and LBW infants from the record of the national statistics, since it was based on the birth registration and birth certificate does not need to be filed if the infant has died soon after birth. The other reason could be the overestimation of LBW or VLBW rate in our study due to the higher response rate in the tertiary care hospitals and general hospitals than hospitals and private obstetric clinics. According to the report from Health Insurance Review Agency, nearly half of total deliveries were conducted at local private clinics and only 8% were conducted at the tertiary care hospitals (23). Therefore, data from tertiary care hospitals which contains more high risk pregnancies could increase the LBW and VLBW rates. In spite of even in possibility of omission and overestimation, the difference is too great and it should be reevaluated in the future studies.
According to the recent National Vital Statistics Report of the United States, the LBW rate was 7.7%, the VLBW rate was 1.44% (21). The LBW rate and the VLBW rate were similar to the ones in our study. However, the LBW and VLBW rates in singletons in our study were 5.9% and 1.3% respectively, which were higher than those of non-Hispanic singletons in the United States by about 1% and 0.5%. The rate of premature infants under 37 weeks of gestation was 11.9%, and that of very premature infants under 32 weeks was 1.95% in the United States, which were higher than those in this study. This means that the rate of high risk infants in Korea is not significantly lower than those of other western developed countries, and also, the data obtained from this study could be considered in the planning and organization of the perinatal care in Korea.
The factors influencing birth weight include biological and medical factors such as gender of the neonate, genetic factors, maternal age, birth order, twin or multiple pregnancy, maternal morbidity, nutritional status and obstetrical complications, and socioeconomic factors such as race, education, financial ability, the extent of prenatal examination, marital status, teenage pregnancy, social and psychological stress (1, 2, 24-28). However, as the data on biological, socioeconomic, demographic factors that could affect birth weight were not collected in this study, the analyses on those factors were not included in this study.
For all that, our data showed significant differences in birth weight and low birth weight rate in relation to maternal age, multiple pregnancy and the gender of the neonate. Of these factors, the maternal age has a close correlation with the birth weight. Infants born to mothers in their teens and those born to mothers aged 35 yr and more have shown LBW rate of 18.6% and 10.6% respectively, which were higher than those of infants born to mothers who were between 20 and 34 yr of age by 11.4% and 3.4%. In addition, the recent small, but steady increase in LBW rate and VLBW rate in the United States was attributed to the increase in multiple pregnancies (21, 22), and in our study we have also found that mean birth weight of twins was lighter than that of singletons by more than 800-1,000 g, and that VLBW rate and LBW rate were also 5 times and 10 times higher than those of singletons. Increase in maternal age and multiple pregnancies could be the cause of increase in LBW and VLBW rates in the future.
There were several previous studies on the distribution of birth weight regarding to the GA in the newborn infants (13-17), but those were hospital-based studies on the newborn infants only who were born at their own hospitals. And there were also a few studies on Koreans living in the United States (29-32), but the number of neonates in the study was quite limited.
To obtain the percentile distribution of birth weight of a group, all the factors mentioned above must be considered, but we were able to control only the maternal age and presence of multiple pregnancy. Therefore, we could not compare our data with those from other countries.
Despite these shortcomings, the data acquired in our study could be the starting point for similar studies in the future, which must be a more thorough study with all the biological, socio-demographic factors put into consideration. In conclusion, we were able to obtain data on LBW rate and VLBW rate, birth weight distribution in a large population in Korea, and we consider that the results from this study would be a great help for future studies on birth weight, frequency of high risk infants, neonatal morbidity and mortality, and perinatal risk factors.
Figures and Tables
Table 1
Distribution of hospitals by the level and geographical area
*Number of deliveries in 2001 reported by the Health Insurance Review Agency (23).
ACKNOWLEDGMENT
The authors wish to express deep gratitude to the neonatologists and obstetricians who are working at the following hospitals for their assistance in this study. Names of the participating hospitals are Ajou University Hospital, Andong Sungso Hospital, Areum Hospital, Asea Hospital, Asan Medical Center of University of Ulsan, Busan Adventist Hospital, Changwon Fatima Hospital, Cheil Hospital, Chonbuk National University Hospital, CL Obstetrics and Gynecology Clinic, Daegu Catholic University Medical Center, Daejeon St. Mary's Hospital of the Catholic University of Korea, Daejin Medical Center Bundang Jesaeng Hospital, Dr. Kim's Ob & Gyn Clinic, Eden Hospital, Ehwa Womans University Mokdong Hospital, Eulji General Hospital, Eulji University Hospital, Eun Hospital, Gachon Medical School Gil Medical Center, Gayajamo Hospital, Geo Je Hospital, Good Moonhwa Hospital, Good Samsun Hospital, Green Hospital, Guri Jang's Obstetrics and Gynecology Clinic, Handong University Good Samaritan Hospital, Hanmaeum Obstetrics and Gynecology Clinic, Hansarang Hospital, Hanyang University Hospital, Hosan Women's Hospital, Hwamyung Ilsin Christian Hospital, Hyekyung Women's Clinic, Hyosung Woman's Medical Center, Hyundai Hospital, Ilsin Christian Hospital, Inje University Sanggye Paik Hospital, Injung Hospital, Jang's Women's Hospital, Jeon-Ju Jesus Hospital, Kangnam Sacred Heart Hospital of Hallym University, Kangnam St. Mary's Hospital of the Catholic University of Korea, Kayang Women's Clinic, Keimyung University Dongsan Medical Center, Konyang University Hospital, Kwangju Christian Hospital, Kyunghee University Hospital, Major Woman's Care Center, Masan Samsung Hospital of Sungkyunkwan University, Min Byung Yul Obstetrics and Gynecology Clinic, Mirae and Heemang Ob and Gyn Clinic, Miz Medi Hospital, Moa Obstetrics and Gynecology Clinic, Moonhwa Obstetrics and Gynecology Clinic, No Won Jae Ob and Gyn Clinic, Our Lady of Mercy Hospital of the Catholic University of Korea, Park Women's Clinic, Pochon Cha University Hospital, Samsung Cheil Hospital of Sungkyunkwan University, Seoul Adventist Hospital, Seoul National University Hospital, Seoul Obstetrics and Gynecology Clinic, Seoul Yale Women's Hospital, Severance Hospital of Yonsei University, Shin Se Gae Women's Hospital, Soonchunhyang Gumi Hospital, Soon Chun Hyang University Cheonan Hospital, Soon Chun Hyang University Hospital, St. Mary's Hospital of the Catholic University of Korea, Sung Ae Hospital, Sungse Hospital, The Catholic University of Korea Holy Family Hospital, Wonju Christian Hospital of Yonsei University, Yiyeon Women's Hospital, and Yoon Obstetrics and Gynecology Clinic.
References
1. Lubchenco LO, Searls DT, Brazie JV. Neonatal mortality rate: relationship to birth weight and gestational age. J Pediatr. 1972. 81:814–822.

2. Lee KS, Paneth N, Gartner LM, Pearlman M. The very low-birth-weight rate: Principal predictor of neonatal mortality in industrialized populations. J Pediatr. 1980. 97:759–764.

3. Stevenson DK, Wright LL, Lemons JA, Oh W, Korones SB, Papile LA, Bauer CR, Stoll BJ, Tyson JE, Shankaran S, Fanaroff AA, Donovan EF, Ehrenkranz RA, Verter J. Very low birth weight outcomes of the National Institute of Child Health and Human Development Neonatal Research Network, January 1993 through December 1994. Am J Obstet Gynecol. 1998. 179:1632–1639.

4. Lemons JA, Bauer CR, Oh W, Korones SB, Papile L, Stoll BJ, Verter J, Temprosa M, Wright LL, Ehrenkranz RA, Fanaroff AA, Stark A, Carlo W, Tyson JE, Donovan EF, Shankaran S, Stevenson DK. Very low birth weight outcomes of the National Institute of Child Health and Human Development Neonatal Research Network, January 1995 through December 1996. Pediatrics. 2001. 107:e1.

5. Horbar JD, Badger GJ, Carpenter JH, Fanaroff AA, Kilpatrick S, LaCorte M, Phibbs R, Soll RF. Members of the Vermont Oxford Network. Trends in mortality and morbidity for very low birth weight infants, 1991-1999. Pediatrics. 2002. 110:143–151.

6. Kim SJ, Namgung R, Lee C, Han DG. The result of intensive care on the very low birth weight infants (1,001-1,500 gm). Korean J Pediatr. 1988. 31:29–39.
7. Jeon SS, Lee WM, Choi YS, Seo SS. Clinical survey of very low birth weight infants. Korean J Pediatr. 1988. 31:1120–1125.
8. Bae CW, Kim MH, Chun CS, Lee C, Moon SJ, Yoo BH, Lim BK, Lee SG, Choi YY, Byun SH, Choi AH, Pi SY, Han DG, Cho SH, Yun CK. Neonatal Statistics of Korea in 1996: Collective results of live-births, neonatal mortality, and incidence of discharge against medical advice at 64 hospitals. J Korean Soc Neonatol. 1997. 4:153–169.
9. Bae CW. Neonatal viability, morbidity, mortality and outcome of very low birth weight infant. Korean J Pediatr. 2000. 43:1–12.
10. Kim SS, Kim MH, Shim JW, Ko SY, Lee EK, Chang YS, Kang IS, Park WS, Lee MH, Lee SI, Lee HJ. Changes in the outcomes of very low birth weight infants. Korean J Pediatr. 2002. 45:828–835.
11. Ma TH, Lee YK, Kim KA, Ko SY, Kim MJ, Shin SM. Outcome of very low birth weight infants in past 2 years at Samsung Cheil Hospital. J Korean Soc Neonatol. 2003. 10:7–13.
12. Kim YO, Kim SH, Cho CY, Choi YY, Kook JH, Hwang TJ. Changes in incidence, survival rate and mortality of very low birth weight infants. Korean J Pediatr. 2003. 46:769–776.
13. Kim YH, Han DG. A study on intrauterine growth standard. Korean J Pediatr. 1984. 27:531–542.
14. Hwang SG, Park JJ, Nam JH, Chung JK. Birth weight percentiles and growth pattern at 21 to 44 weeks of gestation. J Korean Med Assoc. 1987. 30:885–895.
15. Seo K, Park YW, Park TK. Birth weight distribution by gestational age and constructing cut-off value for fetal growth retardation (FGR): their statistical consideration. Korean J Obstet Gynecol. 1989. 32:530–540.
16. Park NH, Yoon BH, Shin HC, Kim SW. Growth pattern of the newborn infants by gestational age. Korean J Obstet Gynecol. 1991. 34:322–330.
17. Lee GH, Kim YW, Lee KB, Seo EJ, Son MS, Ahn HG, Seok EW, Choi YJ, Kim GJ, Kim SY, Hwang BC, Choi YD, Kim SY, Sohn SJ. Change of birth weight -gestational age table. Korean J Obstet Gynecol. 2001. 44:1851–1856.
18. Williams RL, Creasy RK, Cunningham GC, Hawes WE, Norris FD, Tashiro M. Fetal growth and perinatal viability in California. Obstet Gynecol. 1982. 59:624–632.
19. Bae YM, Bae CW. The changes in the mortality rates of low birth weight infant and very low birth weight infant in Korea over the past 40 years. J Korean Med Sci. 2004. 19:27–31.

20. Korea statistical information system. Accessed march 2, 2004. URL: http://kosis.nso.go.kr.
21. Martin JA, Hamilton BE, Ventura SJ, Menacker F, Park MM, Sutton PD. Births: final data for 2001. Natl Vital Stat Rep. 2002. 51:1–102.
22. Martin JA, Hamilton BE, Ventura SJ, Menacker F, Park MM. Births: final data for 2000. Natl Vital Stat Rep. 2002. 50:1–101.
23. Health Insurance Review Agency. A report on the appropriateness of health insurance reimbursement on cesarean section. Health Insurance Review Agency. 2002. 22–36.
24. Gould JB, LeRoy S. Socioeconomic status and low birth weight: a racial comparison. Pediatrics. 1988. 82:896–904.
25. Savitz DA, Blackmore CA, Thorp JM. Epidemiologic characteristics of preterm delivery: etiologic heterogeneity. Am J Obstet Gynecol. 1991. 164:467–471.

26. Sumits T, Bennett R, Gould J. Maternal risks for very low birth weight infant mortality. Pediatrics. 1996. 98:236–241.
27. Gould JB, Madan A, Qin C, Chavez G. Perinatal outcomes in two dissimilar immigrant populations in the United States: a dual epidemiologic paradox. Pediatrics. 2003. 111:e676–e682.

28. Kitchen WH, Ryan MM, Rickards A, Astbury J, Ford G, Lissenden JV, Keith CG, Keir EH. Changing outcome over 13 years of very low birthweight infants. Semin Perinatol. 1982. 6:373–389.
29. Mor JM, Alexander GR, Kieffer EC, Baruffi G. Birth outcomes of Korean women in Hawaii. Public Health Rep. 1993. 108:500–505.
30. Singh GK, Yu SM. Birthweight differentials among Asian Americans. Am J Public Health. 1994. 84:1444–1449.

31. Wang X, Guyer B, Paige DM. Differences in gestational age-specific birthweight among Chinese, Japanese and white Americans. Int J Epidemiol. 1994. 23:119–128.

32. Shiono PH, Rauh VA, Park M, Lederman SA, Zuskar D. Ethnic differences in birth weight: the role of lifestyle and other factors. Am J Public Health. 1997. 87:787–793.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download