Abstract
A 19-year-old male patient presented with facial hemi-atrophy with unilateral spasms of the masseter and temporalis muscles. Ultrasound therapy and Transcutaneous Electric Nerve Stimulation therapy, known as combination therapy, were given on alternate days for 2 weeks. At the end of 2 weeks of combination therapy the patient reported a drastic reduction in the number of episodes of muscle spasm. The visual analog scale score for tenderness of the masseter and temporalis was also markedly reduced. No one has previously used combination therapy for the treatment of facial hemi-atrophy with hemi-facial spasms. The encouraging results of the combination therapy has prompted us to document this study.
Hemi-facial atrophy (HFA) is a degenerative condition characterized by slow and progressive atrophy of the face including the muscles, bones, and skin affecting one side of face [1]. It was first reported by Parry in 1815 and described by Romberg in 1846 [2]. Wartenberg [3] proposed that progressive hemi-facial atrophy is a heredo-degenerative disease, but its etiology is still not established.
The prevalence rate of HFA is said to be 1 in 700,000 in the general population [4]. The incidence of HFA is higher in women. The left side is commonly affected [5]. Disturbance in fat metabolism, endocrine disturbances, autoimmunity, heredity, and local facial trauma are believed to be associated with its pathogenesis. Some inherent relationship between HFA and the disorder of malformation or disturbed migration of neural crest cells might also be associated [5]. This syndrome mostly onsets in the first and second decades of life, with the atrophy progressing gradually and then stabilizing on its own [2]. The salient features of HFA have been described by Wartenbergand Nader [25]. HFA may overlap with various clinical entities like atrophy of the tongue, hemi-facial/hemi-masticatory spasm (HMS), linear scleroderma, vitiligo, and hyperpigmentation [6].
HMS in patients with HFA is a challenge for the clinician. Treatment with pharmacotherapy, like carbamazepine or phenytoin therapy, has been of little advantage in patients suffering from HMS. Botulinum toxin A (BTX) injections into the affected muscles has been a treatment option but the procedure is invasive, traumatic and temporary. In this case report, we have used a conservative non-invasive modality, TENS with ultrasound therapy, also known as combination therapy, which has given us encouraging results.
A 19-year-old male patient reported to the department of oral medicine and radiology with a chief complaint of pain on the left side of his face for the previous 7 months and a reduction in size of the left side of his face over the past 5 years (Fig. 1).
It started with a taut feeling on the left side that was followed by increased pigmentation in that area, and after few months the patient noticed that the left side of his face looked smaller than the right. The reduction in size was first noticed on the forehead. The patient also complained of a reduction in the hair present on the involved area. Over the previous 2 years, the patient was concerned about periodic and intense sharp painful spasms on the left side of the face, which interfered with mastication and speech. The spasm (3–4 episodes per day) lasted for 7–8 minutes each. Past medical history suggested maternal anemia during pregnancy. No history of trauma or infections was given.
The patient's vital signs were within normal limits, he was 6 feet tall and weighed 105 kg. Extra-oral inspection revealed gross facial asymmetry with marked atrophy on the left side of the face. A linear depression extending 2 cm from the hairline on the scalp involving the forehead (coup de sabre) till the glabella was noted. The left zygomatic arch, malar process, supra and infra-orbital rim were noticeably smaller when compared to the right side. Obliteration of the naso-labial fold with slight deviation of mouth and chin were also present on the left side. Skin on the left side of the face was hyper-pigmented. On palpation, the masseter and temporalis muscles were taut and had multiple tender points. The VAS score was 8. The temporo-mandibular joint also was tender, showed asynchronous movements of the condyles, with aggravated movements on the left side. Mouth opening was 4.5 cm. When the trigeminal and facial nerves were examined clinically, there was no detectable abnormality present.
Intraoral examination showed a retained left deciduous molar. The patient had Angles class 1 malocclusion, which means “The mesio-buccal cusp of the maxillary first permanent molar articulates in the mesio-buccal groove of the mandibular first permanent molar.” [7]. He also had a posterior open bite on the left side and cross bite, i.e. the left mandibular central incisor overlapped the left maxillary central incisor. Electrocardiogram and cone beam computed tomography (CBCT) were advised. The ECG was normal. The CBCT scan showed that the dimensions of the entire maxilla on the left side was smaller when compared to the right side along with a hypoplastic malar process (Fig. 2). A provisional diagnosis of left hemi-facial atrophy with spasm of the masseter muscle was made which was also confirmed by a neuro physician.
The patient was advised to take ultrasound therapy and TENS therapy on alternate days for 2 weeks. Ultrasound therapy was given with a frequency of .8 watt/cm2 on pulsed mode for 7 minutes, followed by TENS which was given on high TENS mode with a frequency of 80 Hz for 12 minutes. The electrodes were kept on the left masseter and temporalis.
At the end of 2 weeks of combination therapy, the patient reported a drastic reduction in the number of episodes of muscle spasm from 3-4 episodes per day to 1 per day. The VAS score for tenderness in the masseter and temporalis was also markedly reduced to 5 from 8 on the VAS. The pain which was initially intense and sharp now became dull and did not interfere much in his daily activities like speech or mastication.
HFA is an irreversible phenomenon. It may be treated with topical steroids and immune suppressants (methotrexate, azathioprine). Ultraviolet A irradiation can be used to arrest the disease development. Several aesthetic measures, like injections of calcium hydroxyl apatite locally, have been useful in hemi-facial atrophy. Silicone implantation, reconstructive or microvascular surgery, fat grafts and dermis grafts, muscle grafts, bone grafts, injections of fat cells (lipo-injection or lipo-filling), orthognathic surgery, allografts, and autologous fat cell transplantation have been useful in rectifications of facial atrophy [8].
HMS is paroxysmal uncontrolled contractions of the unilateral jaw-closing muscles. Kim mentioned that deep changes in tissue due to facial hemi-atrophy causes the trigeminal neuropathy. The temporalis and masseter muscles are supplied by the trigeminal nerve, which runs in a restricted area between the lateral pterygoid muscle and the skull. Here it can be stretched or compressed by changes in the tissues resulting in focal demyelination [9].
Although there are numerous reported cases of HFA in the literature, on conducting a computerized database search in Pubmed, we found only 10 cases that reported HFA with HMS (Table 1).
HMS treatment is a challenge to the clinician. Pharmacotherapy, which includes carbamazepine or phenytoin, does not provide much benefit in most patients with HMS [6].
BTX has been a choice of treatment for HMS. BTX paralyses the muscles by blocking the cholinergic signal transmission irreversibly at the presynaptic nerve endings [101112]. There is moderate improvement of symptoms in most patients [12]. Injection with BTX results in decreased muscle activity for three to four months [13]. The drawback is the repetition of the injection after every 3–4 months. Other adverse effects of BTX include double vision, temporary facial nerve paralysis, and ptosis [14]. This treatment is symptomatic, and patients have reported a decline in the efficiency of BTX after a few years [12].
In this case we used TENS and ultrasound therapy as a treatment modality which is a non-pharmacological pain control method. The use of two modalities simultaneously, and at the same site, is reported in the literature and described as “combination therapy”.
Previous studies have confirmed the TENS utility in the treatment of trigger points. Ultrasound is also a helpful means of inactivating trigger points [15].
TENS primarily works on gate control and the endogenous opioid theory [16]. Ultrasound derives therapeutic results from its non-thermal and thermal properties [17]. Ultrasound interrupts scar tissue formation, improving local circulation and relaxing the muscle [18]. It was found that a combination of TENS and ultrasound therapy proved effective in treating active trigger points [15]. A study concluded that combination therapy is effective to relieve trigger points and pain for the acute stage of trapezitis [19].
No one has previously used combination therapy for the treatment of facial hemi-atrophy with hemi-facial spasms. It proved to be effective in reducing the episodes of spasm from 2–3 in a day to 1 in 2 per day, and also in relieving the pain of the patient from the VAS score of 8 to 5. The encouraging results of this combination therapy have prompted us to document this study. Treating facial hemi-atrophy with hemi-facial spasms has been challenging for the clinicians reporting this early case. We encourage more readers to use this therapy, from which greater evidence can be acquired.
References
1. Pinheiro TP, Silva CC, Silveira CS, Botelho PC, Pinheiro Md, Pinheiro Jde J. Progressive hemifacial atrophy--case report. Med Oral Patol Oral Cir Bucal. 2006; 11:E112–E114. PMID: 16505785.
2. Patel H, Thakkar C, Patel K. Parry-Romberg syndrome: a rare entity. J Maxillofac Oral Surg. 2010; 9:247–250. PMID: 22190798.

4. Sande A, Risbud M, Kshar A, Paranjpe AO. Progressive hemifacial atrophy. Dent Res J (Isfahan). 2013; 10:108–111. PMID: 23878573.
5. Al-Aizari NA, Azzeghaiby SN, Al-Shamiri HM, Darwish S, Tarakji B. Oral manifestations of Parry-Romberg syndrome: a review of literature. Avicenna J Med. 2015; 5:25–28. PMID: 25878963.

6. Panda AK, Gopinath G, Singh S. Parry-Romberg syndrome with hemimasticatory spasm in pregnancy; a dystonia mimic. J Neurosci Rural Pract. 2014; 5:184–186. PMID: 24966565.

7. Goyal S, Goyal S. Pattern of dental malocclusion in orthodontic patients in rwanda: a retrospective hospital based study. Rwanda Med J. 2012; 69:13–18.
8. Ebersbach G, Kabus C, Schelosky L, Terstegge L, Poewe W. Hemimasticatory spasm in hemifacial atrophy: diagnostic and therapeutic aspects in two patients. Mov Disord. 1995; 10:504–507. PMID: 7565834.

9. Kim HJ, Jeon BS, Lee KW. Hemimasticatory spasm associated with localized scleroderma and facial hemiatrophy. Arch Neurol. 2000; 57:576–580. PMID: 10768634.

10. Cersósimo MG, Bertoti A, Roca CU, Micheli F. Botulinum toxin in a case of hemimasticatory spasm with severe worsening during pregnancy. Clin Neuropharmacol. 2004; 27:6–8. PMID: 15090929.

11. Teive HA, Piovesan EJ, Germiniani FM, Camargo CH, Sa D, Scola RH, et al. Hemimasticatory spasm treated with botulinum toxin: case report. Arq Neuropsiquiatr. 2002; 60:288–289. PMID: 12068362.

12. Rosenstengel C, Matthes M, Baldauf J, Fleck S, Schroeder H. Hemifacial spasm: conservative and surgical treatment options. Dtsch Arztebl Int. 2012; 109:667–673. PMID: 23264807.
13. Nayyar P, Kumar P, Nayyar PV, Singh A. BOTOX: broadening the horizon of dentistry. J Clin Diagn Res. 2014; 8:ZE25–ZE29.
14. Wang A, Jankovic J. Hemifacial spasm: clinical findings and treatment. Muscle Nerve. 1998; 21:1740–1747. PMID: 9843077.

15. Mukkannavar PB. Effect of combination therapy [TENS & ultrasound] and ischemic compression in the treatment of active myofascial trigger points. J Exerc Sci Physiother. 2008; 4:95–103.
16. Kasat V, Gupta A, Ladda R, Kathariya M, Saluja H, Farooqui AA. Transcutaneous electric nerve stimulation (TENS) in dentistry: a review. J Clin Exp Dent. 2014; 6:e562–e568. PMID: 25674327.

17. Singh R, Rao K, Anap D, Iyer C, Khatri S. The short term effect of TheraBite® on temporomandibular dysfunction: a case study. Int J Phys Med Rehabil. 2013; 1:102.

18. Pal US, Kumar L, Mehta G, Singh N, Singh G, Singh M, et al. Trends in management of myofacial pain. Natl J Maxillofac Surg. 2014; 5:109–116. PMID: 25937719.

19. Rajalakshmi A, Sathish KM, Ivvala AS, Mahalakshmi R. Effect of transcutaneous electrical nerve stimulation in trapezitis. Int J Physiother Res. 2013; 1:205–207.
Fig. 2
Hypoplastic malar process. Cone beam computed tomography shows hypoplastic malar process of the left face.

Table 1
Hemi-facial Atrophy with Muscle Spasm
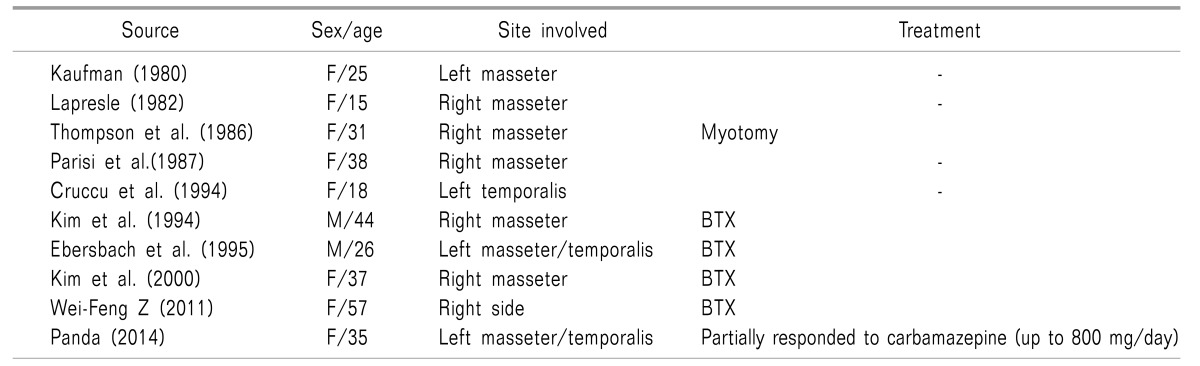
In the Pubmed search, only 10 cases were documented in the literature of hemi-facial atrophy with muscle spasm. The table shows the summary of treatment modalities documented in cases of hemi-facial atrophy with spasm reported from 1980 to 2015, with age, the sex of the patients, and the muscle or site involved with the treatment modalities.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download