Abstract
Thoracotomy is a surgical technique used to reach the thoracic cavity. Management of pain due to thoracotomy is important in order to protect the operative respiratory reserves and decrease complications. For thoracotomy pain, blocks (such as thoracic epidural, paravertebral, etc.) and pleural catheterization and intravenous drugs (such as nonsteroidal anti-inflammatory drugs [NSAIDs], and opioids, etc., can be used. We performed a serratus anterior plane (SAP) block followed by catheterization for thoracotomy pain. We used 20 ml 0.25% bupivacaine for analgesia in a patient who underwent wedge resection for a lung malignancy. We provided analgesia for a period of close to seven hours for the patient, whose postoperative VAS (visual analog scale) scores were recorded. We believe that an SAP block is effective and efficient for the management of pain after thoracotomy.
Posterolateral thoracotomy is the most frequently performed method for exploring the thoracic cavity. Pain can develop through sensory afferent nerves originating from the incision and drainage sites, the mediastinal pleura, and the ipsilateral shoulder following the thoracotomy. Because there is no analgesic technique that can block various pain afferents at once, multimodal analgesia is required [1].
Ideal analgesia techniques include the administration of intravenous (IV) drugs (opioids, nonsteroidal anti-inflammatory drugs [NSAIDs], etc.), local anesthetic injections to the wound site, and nerve blocks (NBs). Thoracic epidural block, paravertebral block, intercostal nerve block (ICNB), and intra/extrapleural block are among the NBs that may be utilized [1]. The use of ultrasonography (US) in NB has increased the use of novel techniques for NB such as the pectoral nerves (PECS) block and transversus abdominis plane (TAP) block [23]. Serratus anterior plane (SAP) block, which may be a suitable approach for analgesia in thoracic surgery, is one of the new field blocks that provides analgesia at the level of T2-T9 [4].
In this report, we present the case of a patient who underwent posterior thoracotomy, an SAP block and catheterization in the same field. The patient received 20 ml of 0.25% bupivacaine, and the visual analog scale (VAS) scores of the patient were recorded.
We will discuss the case of a patient, who required additional analgesics at the seventh postoperative hour and was administered both local anesthetics and IV analgesics through a catheter.
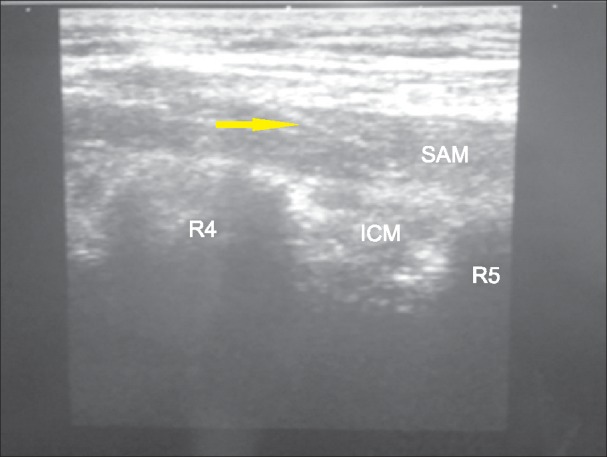
A 63-year-old female patient weighing 80 kg with a height of 155 cm underwent wedge resection via thoracotomy for a lung malignancy. We offered the SAP block to the patient and explained the procedure in detail. She agreed to undergo the procedure, and following the patient's provision of informed consent, we described the VAS to the patient (VAS; 0: no pain, 10: maximal pain). Standard monitoring was performed, an IV vascular access was introduced, and an infusion of NaCl 0.9% was started. After induction of anesthesia, the patient was intubated and mechanical ventilation was initiated. Subsequent to the termination of the operation, skin closure, and appropriate field cleansing, linear ultrasound (USG) scanning was performed by orienting the probe in the sagittal plane while the patient was positioned in the lateral decubitus position. The fifth rib in the mid-axillary line was detected and the probe directed in a horizontal manner. The serratus anterior, latissimus dorsi, and the intercostal muscles were identified in the fourth and fifth intercostal levels with a linear probe (10-12 Hz). A 20 G 100 mm US-visible peripheral nerve block needle was placed under the serratus anterior and intercostal muscles. Bupivacaine 20 ml in a concentration of 0.25% was administered under the serratus muscle after a test dose of 1 ml using an in-plane technique (Fig. 1). A dilution (0.25%) of local anesthetic (LA) was titrated with special monitoring to prevent paralysis of the respiratory muscles and to avoid additional motor blocks. A catheter was placed subsequently (Fig. 2).
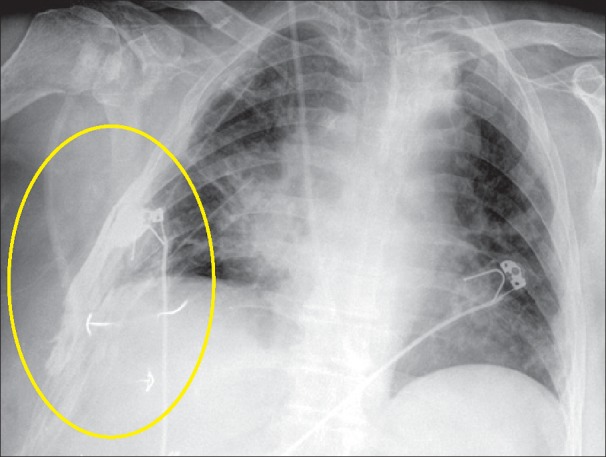
The patient was extubated and transferred to the intensive care unit. During the control posterioanterior (PA) chest x-ray performed in the first hour postoperative, 10 ml of contrast material (iohexol) was injected through the catheter concomitantly. Contrast material was seen to spread on the costae at the lateral thorax starting at the fourth intercostal level and extending to the ninth intercostal level, lateral to the right lung (Fig. 3). The patient was administered 20 ml bupivacaine in a concentration of 0.25% through the catheter for analgesia at the seventh hour postoperative, at which time the patient's VAS score was 4/10. An NSAID was administered through the IV route since the VAS score increased again to 4/10 during the follow-up. Subsequent VAS scores were around 2/10, and the patient was transferred to the ward at the 18th hour postoperative.
In thoracic surgery, postoperative analgesia is important to prevent respiratory problems and chronic pain. Sensory afferent nerves involved at the sites of pain following thoracotomy are carried by intercostal nerves (T4-T6) at the incision site, intercostal nerves (T7-T8) at the sites of thoracic drains, the vagus nerve in the mediastinal pleura, the phrenic nerve (C3-C5) at the central diaphragmatic pleura, and the brachial plexus at the ipsilateral shoulder [1].
Epidural analgesia is accepted as the gold standard for thoracotomy pain [1]. The paravertebral block is another option to be used for analgesia. This provides a level of analgesia similar to the epidural block and have a lower rate of side effects [5]. Analgesia could be provided using a multi-level ICNB through the administration of local analgesics through intra/extrapleural catheters [1]. ICNB and IV routes could also be used in the management of thoracotomy pain [1]. For thoracotomy pain, a wide space should be blocked and long-term analgesia should be required. In ICNB, a limited space is blocked by a single injection. Therefore, the use of ICNB is limited due to the necessity of multiple injections and the requirement of frequent repeats of these blocks. On the other hand, drugs that are administered solely intravenously are effective in pain control, but higher doses of opioids are needed to relieve the pain that is aggravated with coughing and respiration [1]. The side effects of thoracic epidural injections such as neuraxial hematomas, hypotension, vomiting, and urinary retention are higher in frequency compared to the paravertebral block [5]. Nevertheless, the paravertebral block also has complications (such as total spinal block, pneumothorax, and neural damage) which are reported in between 2.6% and 5.7% of cases [6]. An intrapleural block, however, has some limitations since the spreading of the drug is uncontrollable and there is a risk of toxicity [7]. For this reason, we used an SAP block for pain control with a posterolateral thoracotomy. We consider that its application is easier and SAP block might be associated with a lower incidence of complications, as well.
In the SAP block, a local anesthetic agent is injected under or above the serratus muscle with US guidance and thus the lateral cutaneous branches of the ICN are blocked and paresthesia is provided in the dermatomes of T2 and T9 [4].
The SAP block was defined in four volunteers by Blanco et al. [4] They injected a mixture of levobupivacaine 0.125% at a dose of 0.4 ml kg-1 and gadolinium (contrast material) under US guidance in two separate fields of the serratus anterior muscle, the superficial and deep parts. Following the superficial blockage, the duration of the block was 752 min and 502 min in the ICN and motor nerves, respectively. The respective values were 386 min and 502 min following the deep injection, respectively. The duration of analgesia was limited to the levels of T2 and T9 [4].
In this present case, we provided paresthesia at the dermatomes of T2 and T10 by injection of bupivacaine. In the PA chest x-ray that was obtained following an injection of 10 ml of contrast material, a spreading type diffusion of the contrast material through the fourth and ninth intercostal areas in the lateral thorax was observed. Twenty ml of bupivacaine 0.25% was injected through the catheter at the seventh postoperative hour (approximately at the 420th minute) since the VAS score of the patient was 4/10. An NSAID was administered intravenously since the VAS scores were around 4/10 at the eighth postoperative hour. The VAS scores were then found to be at 1-2/10.
Paresthesia at the levels T2-T10 and a duration of analgesia of approximately 420 min following the block were compatible with the literature results. The explanation for analgesia being at an inadequate level via the local anesthetic injection after the seventh hour postoperative was attributed to the migration of the catheter that was placed under the serratus muscle and the presence of sensory afferents originating outside the block area [4].
In one of the two case reports presenting cases with SAP blocks, López-Matamala et al. [8] applied an SAP blocks in two patients with respiratory failure using 20 ml levobupivacaine. They reported that weaning was successful following infusion of a levobupivacaine 0.625% through the catheter. In another case report, Kunhabdulla et al. [9]
provided pain palliation in a patient with a rib fracture using an injection of 20 mg levobupivacaine (at a concentration of 0.125%) followed by an infusion at a concentration of 0.0625% and a dose of 7-12 ml/hour. Since the patient in their case was obese and had a high likelihood of experiencing complications with thoracic epidural application, and since the ICNB required repetitive applications, the authors found it more appropriate to use the SAP block [9].
The easier application of the SAP block compared to the present methods in the management of thoracotomy pain, that require multimodal analgesia, as well as fewer potential side effects, seem to be the advantages of the SAP block. We suggest that controlled studies should be carried out to investigate the effectiveness of the SAP block.
References
1. Slinger PD, Campos JH. Anesthesia for thoracic surgery. In : Miller RD, editor. Miller's anesthesia. 8th ed. Philadelphia (PA): Elsevier Saunders;2015. p. 1942–2006.
2. Blanco R. The 'pecs block': a novel technique for providing analgesia after breast surgery. Anaesthesia. 2011; 66:847–848. PMID: 21831090.

3. Gharaei H, Imani F, Almasi F, Solimani M. The effect of ultrasound-guided TAPB on pain management after total abdominal hysterectomy. Korean J Pain. 2013; 26:374–378. PMID: 24156004.

4. Blanco R, Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013; 68:1107–1113. PMID: 23923989.

5. Gulbahar G, Kocer B, Muratli SN, Yildirim E, Gulbahar O, Dural K, et al. A comparison of epidural and paravertebral catheterisation techniques in post-thoracotomy pain management. Eur J Cardiothorac Surg. 2010; 37:467–472. PMID: 19709893.

6. Lönnqvist PA, MacKenzie J, Soni AK, Conacher ID. Paravertebral blockade. Failure rate and complications. Anaesthesia. 1995; 50:813–815. PMID: 7573876.
7. Schneider RF, Villamena PC, Harvey J, Surick BG, Surick IW, Beattie EJ. Lack of efficacy of intrapleural bupivacaine for postoperative analgesia following thoracotomy. Chest. 1993; 103:414–416. PMID: 8432129.

8. López-Matamala B, Fajardo M, Estébanez-Montiel B, Blancas R, Alfaro P, Chana M. A new thoracic interfascial plane block as anesthesia for difficult weaning due to ribcage pain in critically ill patients. Med Intensiva. 2014; 38:463–465. PMID: 24289954.

9. Kunhabdulla NP, Agarwal A, Gaur A, Gautam SK, Gupta R, Agarwal A. Serratus anterior plane block for multiple rib fractures. Pain Physician. 2014; 17:E651–E653. PMID: 25247916.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download