Abstract
Although discal cysts are a rare cause of low back pain and radiculopathy. Currently, surgical excision is usually the first-line treatment for discal cysts. However, alternative treatment methods have been suggested, as in some cases symptoms have improved with interventional therapies. A 27-year-old man presented with an acute onset of severe pain, and was found to have a discal cyst after an open discectomy. The patient underwent cyst aspiration and steroid injection through the facet joint under C-arm guidance. After the procedure, the patient's pain improved to NRS 0-1. On outpatient physical examination 1 week, and 1 and 3 months later, no abnormal neurological symptoms were present, and pain did not persist; thus, follow-up observation was terminated. When a discal cyst is diagnosed, it is more appropriate to consider interventional management instead of surgery as a first-line treatment, while planning for surgical resection if the symptoms do not improve or accompanying neurologic deficits progress.
Discal cysts were first described in 2001 [1]. Although the pathogenesis of discal cysts has not been clearly defined, the primary symptoms of chronic low back pain and radiculopathy are the same as for a herniated intervertebral disc (HIVD), which has a higher prevalence. Accordingly, it is necessary to distinguish between these conditions. Surgical excision is usually the first-line treatment for discal cysts [12345]. However, alternative treatment methods like computed tomography (CT)-guided aspiration and steroid injection or transforaminal epidural injection have been suggested; in some cases symptoms have improved with alternative treatments [678].
Using C-arm guided aspiration and steroid injection, the authors effectively treated a discal cyst occurring in the same area where open discectomy had been performed previously. The case is reported with a review of the literature.
A 27-year-old man (height, 181 cm; weight, 76 kg) visited the outpatient orthopedic department with a chief complaint of low back pain. He had received medication treatment 8 years previously due to the same symptoms. Since then, he had experienced pain rated as 3-4 on an 0-10 numeric rating scale (NRS) when bending and straightening at the waist, but had not received any other treatment. Without any specific inciting event, the pain had begun to worsen 2 years ago. In the past 4 months, the severity of the pain had increased, with the patient reporting severe low back pain reaching 8 on the 0-10 NRS, and numbness extending to the right leg. On lumbar spine magnetic resonance imaging (MRI), indications of HIVD and cauda equina compression were found at the 4th and 5th lumbar intervertebral disc levels (Fig. 1). Consequently, an emergency open discectomy was performed. There was no pattern of disc sequestration, but a huge mass compressing the right 5th lumbar vertebral (L5) nerve root was revealed. The surgery was completed with excision of the mass only. On postoperative day 2, the 0-10 NRS severity of the low back pain had decreased to 4. Although the right leg numbness persisted, the patient was discharged with plans for outpatient follow-up. At postoperative week 2, a physical examination performed at the orthopedics department showed no abnormalities of motor function, and the patient reported improvement in his symptoms, with only mild numbness remaining in the right leg. However, two days after that outpatient visit, the patient's low back pain began to gradually worsen. After one week, the patient was admitted to our emergency room with a chief complaint of pain severe enough to prevent ambulation. At that time, the extent intensity of his low back pain was 9-10 on the NRS. Physical examination in the emergency room revealed numbness along the L5 dermatome; the motor examination revealed only a slightly reduced extensor proprius hallucis muscle strength reduced slightly to 4/5, with an abnormal finding of 1-2 seconds of right ankle clonus.
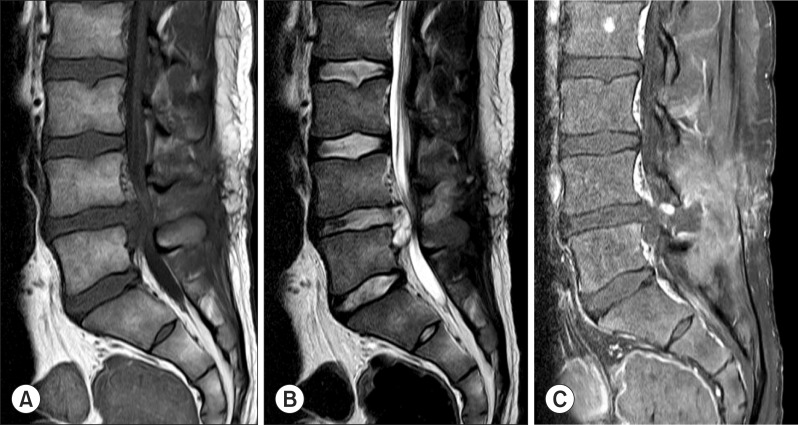
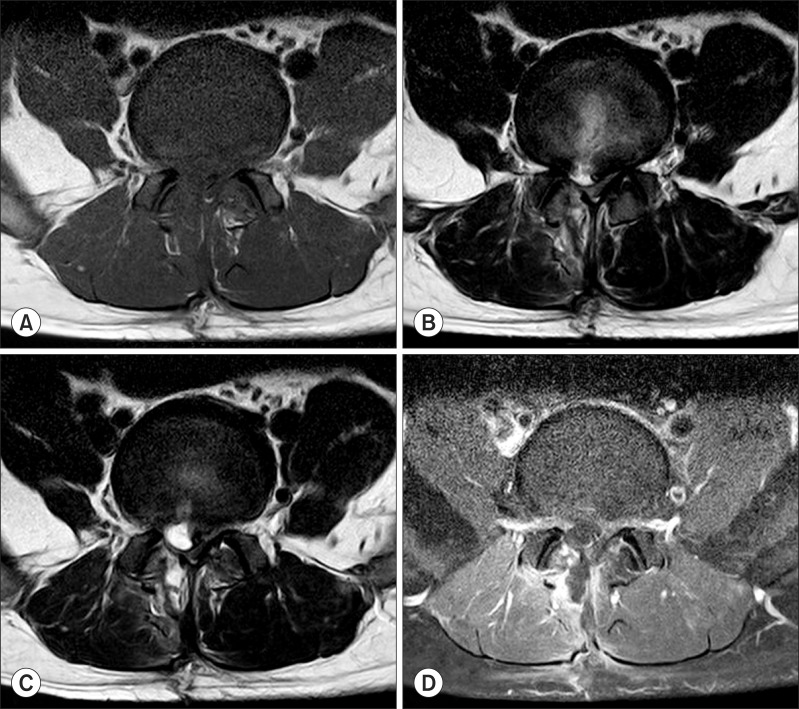
The emergency lumbar spine MRI showed L5 nerve root compression by a 1.2 × 2 cm sized cystic lesion appearing in the area where the surgery had been performed, with concurrent cauda equina compression (Figs. 2, 3). This lesion was radiologically diagnosed as a discal cyst with a connecting channel to the 4th lumbar and 5th lumbar intervertebral disc observed on the MRI. Because the patient refused re-operation, the case was referred to the department of anesthesiology for non-surgical intervention therapy.
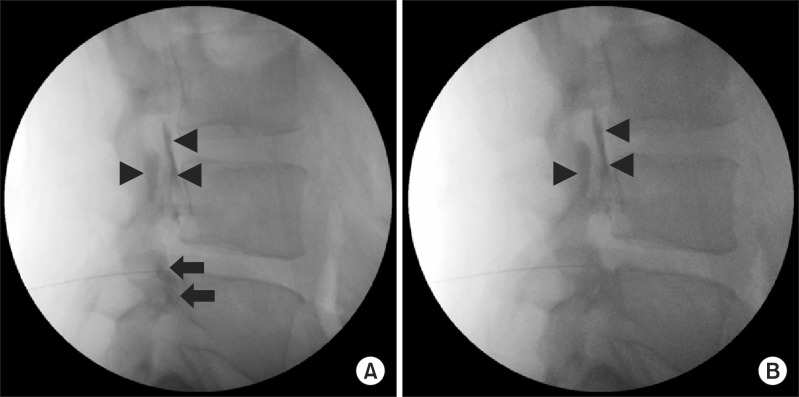
The emergency MRI showed that the discal cyst was located just anterior to the right L4-5 facet joint, so the decision was made to perform a C-arm guided needle aspiration and steroid injection through the facet joint. Informed consent was obtained from the patient and his guardian. The procedure was performed on postoperative day 22. The patient was placed in the prone position and lumbar lordosis was reduced with a pillow placed under the lower abdomen. The cyst was approached through the superior aspect of the right L4-5 facet joint using a 25G spinal needle with a C-arm guide. However, because the patient complained of paresthesia in the right L5 dermatome, the needle was moved backward, rotated 180 degrees, and then re-advanced. Because the patient complained of paresthesia again, the needle was removed. Another approach was attempted inferiorly using a 22G spinal needle. After placement in the patient's right L4-5 facet joint space, the needle was advanced through the right L4-5 facet joint until the achievement of the "pop" sensation while the lateral image of the C-arm and the patient's symptoms were monitored. After injection of 0.5 ml contrast medium to confirm that the needle was inside the cyst, 1.2 ml of cystic fluid (Fig. 4) was aspirated. The procedure was completed with the injection of 10 mg of triamcinolone (Fig. 5). After the procedure, the patient remained in the supine position under observation in the pain clinic. After 1 hour, the patient's pain improved to NRS 0-1. There were no other neurological abnormalities, and the patient was transferred to the general ward. Following 2 days of monitoring in the general ward, the patient was discharged, since the symptoms had not recurred and improvement had been maintained. The cystic fluid showed a red blood cell count of 512,000/µl and white blood cell count of 1,500/µl (differential count: polymorphonuclear cells 85%, and mononuclear cells 15%), while a culture showed no abnormal findings (no bacteria and no growth).
During outpatient physical examinations 1 week, 1 month, and 3 months later, no abnormal neurological symptoms were present, and the pain did not persist. Thus, follow-up observation was terminated.
Discal cysts are defined as intraspinal extradural cysts with a distinct communication with the corresponding intervertebral discs [14]. Younger men are more susceptible to discal cysts compared to degenerative lumbar HIVD patients [9]. They are also reportedly more prevalent in Asians [10].
The pathogenesis of discal cysts remains unknown, with two possible hypotheses suggested. Toyama et al. [11] and Chiba et al. [1] proposed that when disc herniation or disc injury occurs, an epidural hematoma is formed as a result of hemorrhage in the epidural venous plexus. An unknown mechanism that hinders the absorption of the hematoma may play a role at this point, such as mucous degeneration at the surface of the hematoma, which may encapsulate the hematoma leading to the later formation of the cysts [1]. The second hypothesis was suggested by Kono et al. [12]. They proposed that the process by which discal cysts occur is similar to that of meniscal cysts in the knees and synovial cysts in the facet joints. They hypothesized that focal degeneration of an intervertebral disc results in a herniated disc and subsequent extrusion and stagnation of fluid content from the herniated disc. This extruded fluid from disc material incites an inflammatory response, leading to reactive pseudomembrane formation and the development of the discal cyst.
The discal cyst that occurred in the present case may have developed from a pseudomembrane in a hematoma, resulting from delayed hemorrhage at the discectomy site.
Whatever the pathogenesis may be, the intraspinal cyst that communicates with the corresponding disc is responsible for the development of the symptoms, low back pain, and radiculopathy. Cystic lesions that can be found in the spinal canal are include perineural cysts, synovial cysts, and extradural arachnoid cysts. These lesions can cause low back pain and radiculopathies. Perineural cysts frequently present as multiple cystic lesions of the nerve root sheath in the lower lumbar spine, and are typically located at the junction of the dorsal root ganglion and the posterior nerve root [13]. Intraspinal synovial cysts are associated with degenerative lumbosacral spine disease, and communicate with the facet joints [14]. Extradural arachnoid cysts may communicate with the subarachnoid space. These cysts are located on the posterior or posterolateral aspect of the dural sac and usually in the lower thoracic spine [15]. Postoperative fluid collection in the operative bed may include seromas, cerebrospinal fluid collection, hematomas, or abscesses, and can cause symptoms by compression of the thecal sac or nerve roots [16]. Chung et al. [17] reported symptomatic a postoperative discal pseudocyst (PDP) after lumbar discectomy. A PDP has been described as a cystic lesion that is attached to a disc that has undergone operation. PDP is similar to our case. However, in histologic evaluation, a PDP demonstrates no evidence of a hematoma and communication with the intervertebral disc is not necessary for PDP diagnosis. Because the cyst in our case showed communication with the intervertebral disc on MRI and the aspirated fluid showed characteristics of a hematoma, our case is different from a PDP. Lee et al. [18] documented the MRI features of discal cysts. The authors reported that the discal cyst did not cross the midline. This phenomenon may occur because the central posterior longitudinal ligament prevents crossing the midline. However, in our case, the discal cyst spanned the midline of the intervertebral disc space, because the posterior longitudinal ligament might have been damaged during the operation.
In general, MRI is the preferred radiological test for diagnosing a discal cyst. Typically, a discal cyst appears as a spherical mass with clear boundaries on MRI, evident as low intensities on T1-weighted images and high signal intensities on T2-weighted images [1819]. In addition, in contrast-enhanced MRI, the rim of the cyst is well-enhanced [18]. However, review of the radiologic findings of discal cysts demonstrated that these signal intensities may not be the rule [10]. CT discography clearly shows the connection between a disc and a discal cyst, by demonstrating flow of contrast into the cyst. This characteristic of a discal cyst distinguishes it from a herniated disc and other cystic lesions [1820].
Chiba et al. [1], who first described discal cysts, removed a symptomatic cyst via microscopic resection. Since then, additional cases of surgical resection have been reported [23518,21]. After surgical resection of the cyst, most patients show significant improvement in symptoms, but recurrence of a discal cyst was reported in one case [18]. Koga et al. [6] reported positive outcomes with CT-guided puncture and steroid injection, as well as with surgical treatment. Demaerel et al. [22] also reported cyst regression without surgery or other interventional therapy, while Chou et al. [8] reported spontaneous regression of a discal cyst during observation for symptomatic improvement after an epidural injection and selective nerve root block. Furthermore, a case in Korea also reported demonstrated dramatic improvement in discal cyst-related symptoms after a transforaminal epidural injection [7]. Because the natural history of discal cysts remains unknown, it is best to determine the treatment options on a case-by-case basis, with consideration of the patient's symptoms, rather than by performing surgery or a procedure immediately after diagnosis.
The authors in this case performed C-arm guided aspiration and steroid injection, with a very satisfactory outcome. The patient's radiculopathy completely resolved, and his pain also dramatically improved to a score of NRS 0-1 within 1 hour after the procedure. In this case, the cyst was located just anterior to a facet joint. This enabled an approach under C-arm guidance, with no damage to a nerve root or spinal nerve. Dasenbrock et al. [23] reported significant regression of a discal cyst after aspiration of a small amount of fluid. Although the aspirated volume was small, rupturing the cyst with a needle allowed the size to be successfully reduced.
A limitation of this case study was that the degree to which the cyst regressed was not confirmed because the patient refused to undergo follow-up MRI. However, since the patient's symptoms improved immediately after the procedure, we thought that the discal cyst was effectively regressed. In addition, long-term follow-up observation was terminated due to improvement in symptoms, which made it difficult to assess any long-term effects.
For patients who experience radiculopathy, MRI is recommended at the initial examination to rule out the possibility of disc disorders and cystic lesions, such as a discal cyst, however rare the likelihood. When a discal cyst is diagnosed, it is more appropriate to consider interventional management instead of surgery as first-line treatment, with plans for surgical resection if the symptoms do not improve or if the accompanying neurologic deficits progress. Moreover, since there have been only case reports on the treatment of discal cysts to date, additional studies to establish a standardized treatment are needed.
References
1. Chiba K, Toyama Y, Matsumoto M, Maruiwa H, Watanabe M, Nishizawa T. Intraspinal cyst communicating with the intervertebral disc in the lumbar spine: discal cyst. Spine (Phila Pa 1976). 2001; 26:2112–2118. PMID: 11698889.

2. Coscia MF, Broshears JR. Lumbar spine intracanalicular discal cysts: two case reports. J Spinal Disord Tech. 2002; 15:431–435. PMID: 12394670.

3. Ishii K, Matsumoto M, Watanabe K, Nakamura M, Chiba K, Toyama Y. Endoscopic resection of cystic lesions in the lumbar spinal canal: a report of two cases. Minim Invasive Neurosurg. 2005; 48:240–243. PMID: 16172971.

4. Nabeta M, Yoshimoto H, Sato S, Hyakumachi T, Yanagibashi Y, Masuda T. Discal cysts of the lumbar spine. Report of five cases. J Neurosurg Spine. 2007; 6:85–89. PMID: 17233299.
5. Murata K, Ikenaga M, Tanaka C, Kanoe H, Okuaaira S. Discal cysts of the lumbar spine: a case report. J Orthop Surg (Hong Kong). 2007; 15:376–379. PMID: 18162691.

6. Koga H, Yone K, Yamamoto T, Komiya S. Percutaneous CT-guided puncture and steroid injection for the treatment of lumbar discal cyst: a case report. Spine (Phila Pa 1976). 2003; 28:E212–E216. PMID: 12782997.

8. Chou D, Smith JS, Chin CT. Spontaneous regression of a discal cyst. Case report. J Neurosurg Spine. 2007; 6:81–84. PMID: 17233298.
9. Jeong GK, Bendo JA. Lumbar intervertebral disc cyst as a cause of radiculopathy. Spine J. 2003; 3:242–246. PMID: 14589206.

10. Aydin S, Abuzayed B, Yildirim H, Bozkus H, Vural M. Discal cysts of the lumbar spine: report of five cases and review of the literature. Eur Spine J. 2010; 19:1621–1626. PMID: 20364391.

11. Toyama Y, Kamata N, Matsumoto M, Nishizawa T, Koyanagi T, Suzuki N, et al. Pathogenesis and diagnostic title of intraspinal cyst communicating with intervertebral disk in the lumbar spine. Rinsho Seikei Geka. 1997; 32:393–400.
12. Kono K, Nakamura H, Inoue Y, Okamura T, Shakudo M, Yamada R. Intraspinal extradural cysts communicating with adjacent herniated disks: imaging characteristics and possible pathogenesis. AJNR Am J Neuroradiol. 1999; 20:1373–1377. PMID: 10473000.
13. Lucantoni C, Than KD, Wang AC, Valdivia-Valdivia JM, Maher CO, La Marca F, et al. Tarlov cysts: a controversial lesion of the sacral spine. Neurosurg Focus. 2011; 31:E14. PMID: 22133181.

14. Liu SS, Williams KD, Drayer BP, Spetzler RF, Sonntag VK. Synovial cysts of the lumbosacral spine: diagnosis by MR imaging. AJNR Am J Neuroradiol. 1989; 10:1239–1242. PMID: 2512789.

15. Rimmelin A, Clouet PL, Salatino S, Kehrli P, Maitrot D, Stephan M, et al. Imaging of thoracic and lumbar spinal extradural arachnoid cysts: report of two cases. Neuroradiology. 1997; 39:203–206. PMID: 9106295.

16. Malhotra A, Kalra VB, Wu X, Grant R, Bronen RA, Abbed KM. Imaging of lumbar spinal surgery complications. Insights Imaging. 2015; 6:579–590. PMID: 26432098.

17. Chung D, Cho DC, Sung JK, Choi E, Bae KJ, Park SY. Retrospective report of symptomatic postoperative discal pseudocyst after lumbar discectomy. Acta Neurochir (Wien). 2012; 154:715–722. PMID: 22223287.

18. Lee HK, Lee DH, Choi CG, Kim SJ, Suh DC, Kahng SK, et al. Discal cyst of the lumbar spine: MR imaging features. Clin Imaging. 2006; 30:326–330. PMID: 16919553.

19. Tokunaga M, Aizawa T, Hyodo H, Sasaki H, Tanaka Y, Sato T. Lumbar discal cyst followed by intervertebral disc herniation: MRI findings of two cases. J Orthop Sci. 2006; 11:81–84. PMID: 16437354.

20. Hwang JH, Park IS, Kang DH, Jung JM. Discal cyst of the lumbar spine. J Korean Neurosurg Soc. 2008; 44:262–264. PMID: 19096689.

21. Ha SW, Ju CI, Kim SW, Lee S, Kim YH, Kim HS. Clinical outcomes of percutaneous endoscopic surgery for lumbar discal cyst. J Korean Neurosurg Soc. 2012; 51:208–214. PMID: 22737300.

22. Demaerel P, Eerens I, Goffin J, Wilms G. Spontaneous regression of an intraspinal disc cyst. Eur Radiol. 2001; 11:2317–2318. PMID: 11702179.

23. Dasenbrock HH, Kathuria S, Witham TF, Gokaslan ZL, Bydon A. Successful treatment of a symptomatic L5/S1 discal cyst by percutaneous CT-guided aspiration. Surg Neurol Int. 2010; 1:41. PMID: 20847922.

Fig. 1
MRI of the lumbar spine. Sagittal (A) and axial (B) T1-weighted MRI of the lumbar spine. The images show an L4-5 HIVD. Sagittal (C) and axial (D) T2-weighted MRI of the lumbar spine. The images show an L4-5 HIVD.
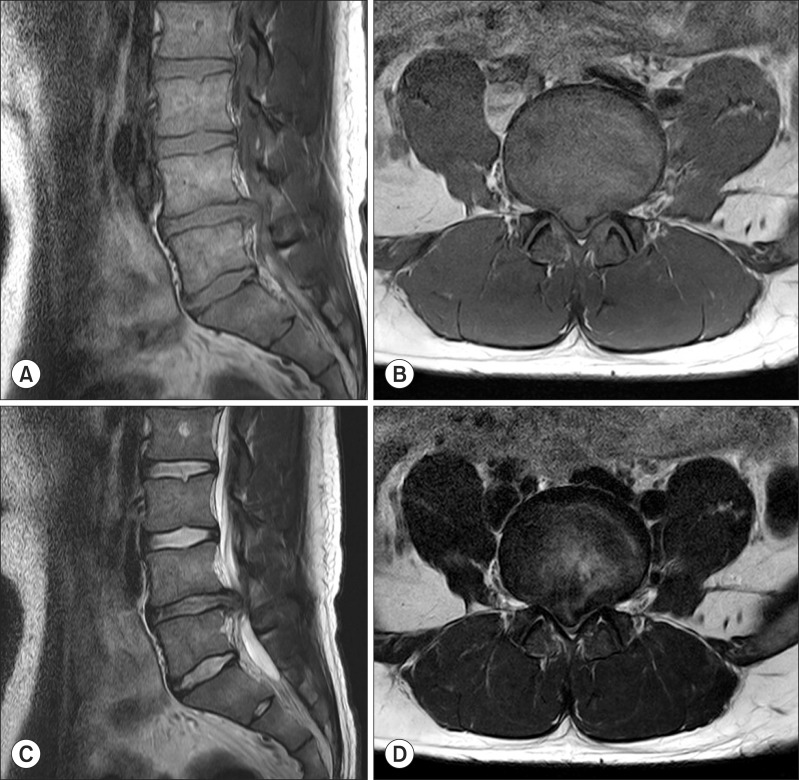
Fig. 2
Sagittal MRI of a discal cyst. (A) The cystic mass in the L4-5 level intraspinal space shows low signal intensity on the T1-weighted image. (B) The cystic mass in the L4-5 level intraspinal space shows high signal intensity on the T2-weighted image. (C) Discal cyst on short tau inversion recovery (STIR) imaging.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download