Abstract
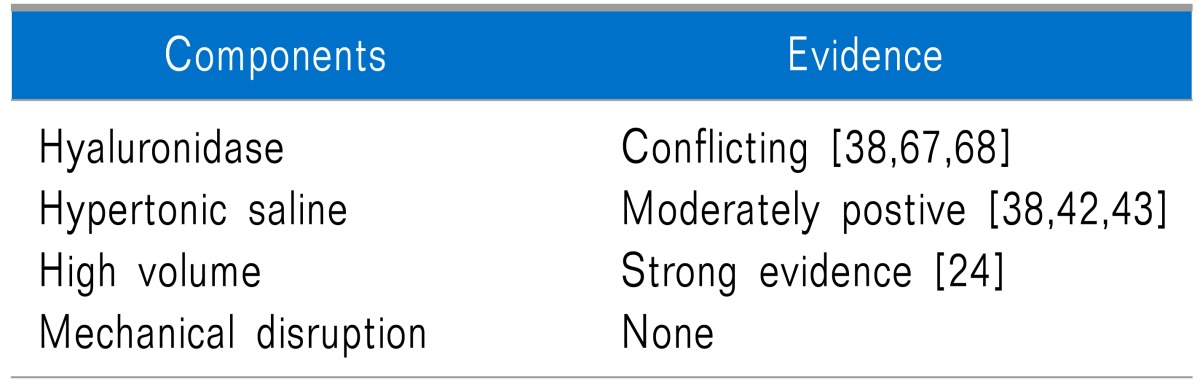
As our population ages and the rate of spine surgery continues to rise, the use epidural lysis of adhesions (LOA) has emerged as a popular treatment to treat spinal stenosis and failed back surgery syndrome. There is moderate evidence that percutaneous LOA is more effective than conventional ESI for both failed back surgery syndrome, spinal stenosis, and lumbar radiculopathy. For cervical HNP, cervical stenosis and mechanical pain not associated with nerve root involvement, the evidence is anecdotal. The benefits of LOA stem from a combination of factors to include the high volumes administered and the use of hypertonic saline. Hyaluronidase has been shown in most, but not all studies to improve treatment outcomes. Although infrequent, complications are more likely to occur after epidural LOA than after conventional epidural steroid injections.
Epidural lysis of adhesions (LOA) represents an important part of the interventional repertoire for the treatment of low back pain that is refractory to more conventional treatments such as epidural steroid injections (ESI). Although not as frequently performed or as controversial as ESI [1-3], in part because the rise in utilization and reimbursement has not been nearly as steep [4], LOA is a commonly performed procedure for treatment of back pain secondary to failed back surgery syndrome (FBSS) and spinal stenosis (SS). In contrast to the socioeconomic burden of the indicated conditions, the breadth of literature related to epidural LOA is minimal. The purpose of this article is to provide an overview of epidural LOA, and to provide an evidence-based review of the mechanisms of action, efficacy and effectiveness, and factors associated with treatment outcome.
MEDLINE and Embase databases were searched between 1970 and 2013 using the search terms 'adhesiolysis', 'lysis of adhesions', 'epiduroscopy', 'epidural neuroplasty', 'epidural adhesions' and 'epidural scar tissue' to identify articles relevant for this review. Clinical trials, observational studies, retrospective studies, animal studies, review articles, case series and reports, and guidelines were all considered. The reference sections of prime articles were then searched to obtain additional references.
FBSS and SS are the two main indications for epidural LOA. FBSS is defined as persistent or recurrent back and/or leg pain following an anatomically successful back surgery. Commonly cited prevalence rates of FBSS from past studies of heterogeneous populations provide a wide range, varying 10% to over 40% [5]. If spine surgical volume continues to increase at a rate similar to the past two decades, the prevalence of FBSS is also likely to increase, especially in the United States [6,7]. The diagnosis of SS is less ambiguous than FBSS, being defined as anatomical narrowing of either the central canal, lateral recesses, or foramina. Although somewhat arbitrary, some past studies have used <12 mm for "relative" stenosis and <10 mm for "absolute" stenosis to define lumbar SS in image-based techniques [8-10]. Some non-cancerous causes of SS include congenitally short pedicles, overgrowth of bony (i.e. osteophytes) and ligamentous tissue, hypertrophic arthritic changes in the facet joints, spondylolisthesis, and bulging or herniated discs. Defining the prevalence of SS, however, has been a challenge due to the lack of universally accepted diagnostic criteria. Commonly cited prevalence rates in the general population typically range between 1.7% and 13.1% [11-13]. In the elderly, the prevalence rates increase substantially. In an ancillary study to the Framingham Study, the prevalence of acquired SS in the 60-69 year old age group ranged from 19.4-47.2% [14].
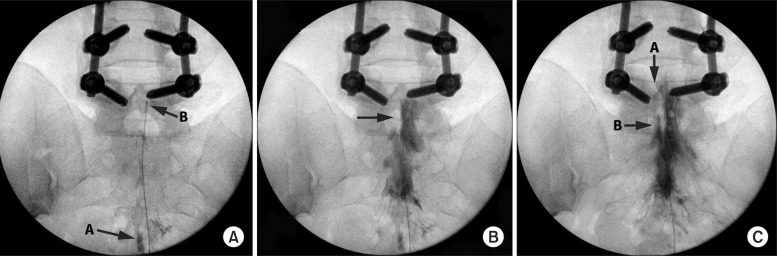
Epidural LOA, also known as epidural neuroplasty and epidural adhesiolysis, is a minimally invasive technique for the treatment of axial spine or radicular pain when conservative therapy has failed. Although many variations of this procedure exist, most LOA performed today are based on the technique developed at Texas Tech Health Sciences Pain Center, published in 1989 [15]. The technique typically involves accessing the epidural space via the sacral hiatus using a large gauge needle and inserting a catheter. The catheter is then advanced to the site of adhesions where epidurography is used to map out the adhesions, and adhesiolysis via the high-volume administration of saline and medications is performed. The original procedure required that the catheter remain in the epidural space for three days, with the injection of different medications on each of the days. The technique was subsequently modified to become an ambulatory procedure similar to a traditional ESI, but involving a catheter that is removed immediately following the injection of a combination of a steroid, local anesthetics, and sometimes hyaluronidase and hypertonic saline (Fig. 1) [16,17].
Regardless of whether the epidural scar tissue was created by a surgical procedure or a non-surgical phenomenon, the common premise for treating FBSS and SS with LOA is that the presence of epidural fibrosis can both cause pain and prevent delivery of medications for relief. The relationship between the presence of scar tissue and pain has been examined by multiple studies, and is still being debated. Among the first to describe this relationship were Kulisch et al, who used progressive local anesthetics during a laminectomy to describe pain sensitive structures in the spinal canal, especially in nerve roots restricted by scar tissues [18]. A frequently sited study by Ross et al. showed that the presence of scar tissue surrounding nerve roots was 3.2 times more likely to cause radicular pain than the absence of scar tissue [19]. In a randomized, controlled, double-blind multicenter trial to test the effectiveness of ACON-L, a scar inhibiting gel, there was a statistically significant correlation between the presence of peridural scar tissue and persistent low back pain [20]. Not all studies, however, have found a correlation between the degree of epidural fibrosis and the intensity of postsurgical pain [21,22]. The dilemma involved in establishing a cause-and-effect relationship between pathology and pain is that the specificity of anatomical abnormalities is low, with many patients having pathology in the absence of pain [23].
Another proposed mechanism of action for epidural LOA is the wash out of inflammatory cytokines from the affected area. A systemic review examined the relationship between the amount of volume injected during ESI and relief of radicular pain [24]. The study found that the larger amount of volume injected, the greater the magnitude of pain relief. The proposed mechanisms of added volume not only include adhesiolysis and washout of inflammatory cytokines, but also lavage of the epidural space, suppression of ectopic discharge from injured nerves, and enhancing blood flow to ischemic nerve roots.
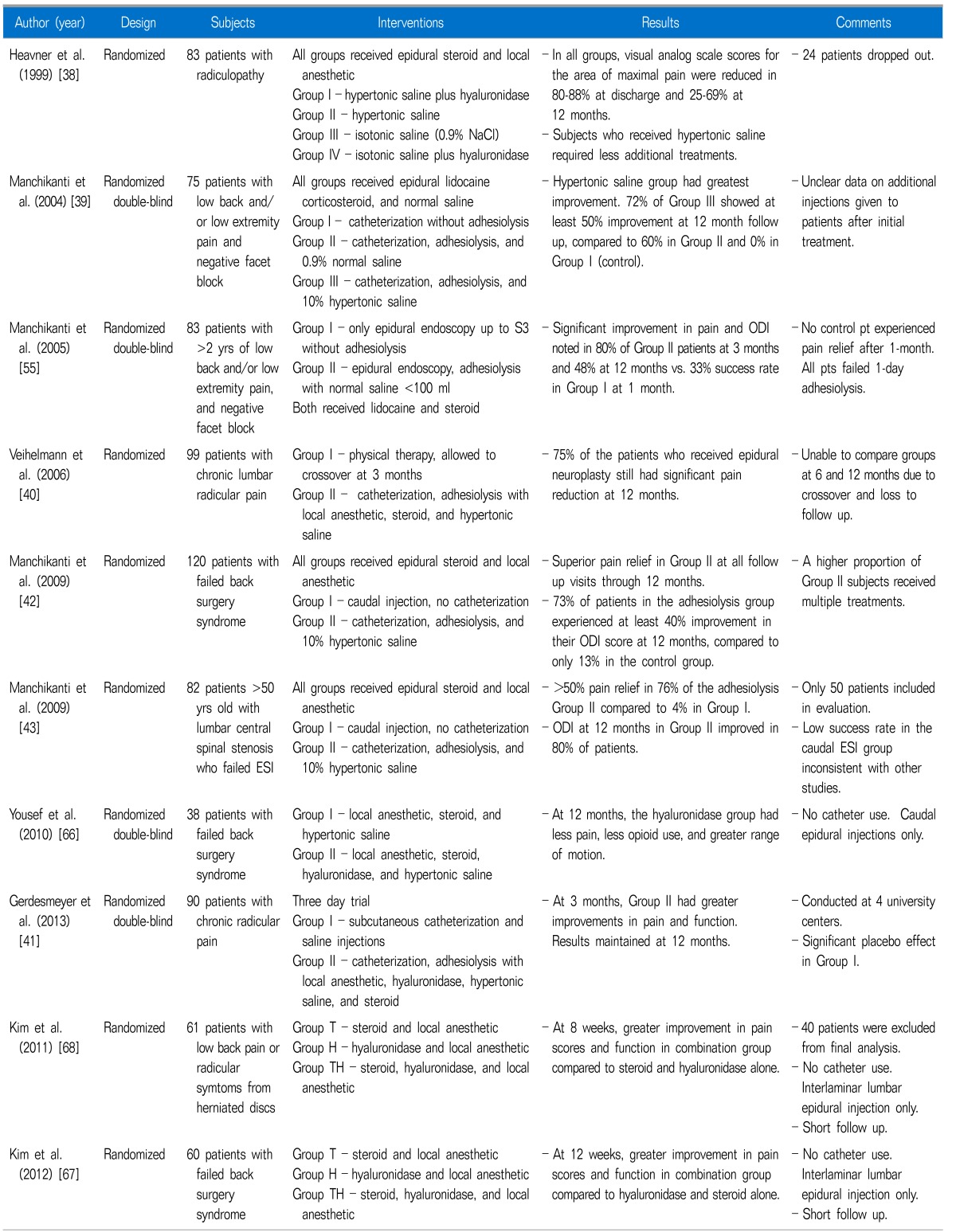
Multiple systematic reviews have been conducted in an attempt to elucidate the possible benefits of epidural lysis of adhesion (LOA) in managing pain due to spinal stenosis and post lumbar surgery syndrome [25-30]. The results of these reviews have been mixed but generally positive, with the evidence of benefit ranging from strong [28] to fair [30]. Additionally, epidural LOA receives mention in multiple practice guidelines and broad reviews of spine interventions [31-37]. Although these systematic reviews and clinical guidelines are generally favorable, they are all based on a small number of randomized studies. To some extent, the variability in conclusions in these reviews stems from different inclusion criteria and outcome measures (Table 1).
The 1999 randomized trial by Heavner, Racz and Raj [38] utilized the group's 3-day adhesiolysis protocol as originally reported in 1989. Patients with low-back pain and radiculopathy were randomized to one of four groups: (1) hypertonic saline plus hyaluronidase, (2) hypertonic saline, (3) isotonic (0.9%) saline or (4) isotonic saline plus hyaluronidase. All groups received similar doses of corticosteroid and local anesthetic. Fifty-nine patients ultimately completed the trial and were followed for one year post-adhesiolysis by collecting visual analog scale (VAS) pain scores and Short Form McGill (SFM) questionnaires. The percentage of patients showing improvement in both VAS and SFM was highest at discharge (80-88%) in all groups and ranged from 25-60% at the 12-month mark, with no statistical differences between groups. A non-statistically significant trend was noted in which patients who received hypertonic saline required less additional treatments.
A 2004 trial by Manchikanti et al. studied the effects of a modified, one-day adhesiolysis protocol in patients with chronic back and/or leg pain [39]. A total of 75 patients without a large disc herniation or compressive radiculopathy were randomized to one of three groups, with all groups receiving a caudally placed epidural catheter and injections of lidocaine, corticosteroid and normal saline. Group I was considered the control and did not receive targeted adhesiolysis guided by epidurography. Groups II and III received targeted adhesiolysis, which was accomplished with 0.9% normal saline in Group II and 10% hypertonic saline in Group III. The greatest improvement in results was noted with the use of targeted hypertonic saline, as 72% of patients in Group III showed at least 50% improvement at 12-month follow-up, compared to 60% in the saline group and 0% in the control group.
Adhesiolysis was compared to physical therapy in a 2006 study by Veihelmann et al. [40]. Ninety-nine patients with chronic lumbar radicular pain either with or without back pain were randomized to receive either physical therapy or a 3-day adhesiolysis protocol that included local anesthetic, steroid and hypertonic saline infused over 30 minutes. They showed statistically significant greater reductions in VAS pain scores for both back and leg pain at 3, 6 and 12 months in the treatment group compared to the control group. Patients in the physical therapy group were allowed to crossover at 3 months and twelve patients opted to do this. A potential weakness of the paper is that they were unable to statistically compare the groups at 6 and 12 months due to crossover, losses to follow-up and surgery. Additionally, the type and frequency of physical therapy sessions were not described.
A later multi-center randomized, double-blind study performed for the same indication compared epidural adhesiolysis to placebo treatment in 90 patients with lumbar radiculopathy [41]. A 3-day protocol was instituted whereby the treatment group received local anesthetic, hyaluronidase, normal saline and hypertonic saline through an epidural catheter. The control group received 10 ml of normal saline through a subcutaneous catheter over the course of 3 days. Both groups received physical therapy after the procedure. Three months post-procedure, the mean VAS pain score improved from 6.7 to 2.9 in the treatment group, and from 6.7 to 4.8 in the control group. Similar benefit favoring the adhesiolysis group was noted for Oswestry Disability Index (ODI) scores. The statistically significant benefit favoring the treatment group was maintained throughout the 12-month follow-up.
Given the presumed mechanism by which LOA provides relief, several recent studies have investigated the potential benefits in post-laminectomy and spinal stenosis patients. A 2009 study by Manchikanti et al. randomized 120 patients with a history of lumbar spine surgery and chronic back pain to one of two groups [42]. Group I functioned as the control and received a caudal injection of local anesthetic, corticosteroid and 0.9% saline. Group II received a targeted ambulatory adhesiolysis treatment with local anesthetic, corticosteroid and 10% saline. The total volume of injectate was held constant between the two groups. Benefit as measured via VAS pain and ODI scores was superior in Group II at 3, 6, and 12 months follow-up; however, the protocol did allow for a significant confounding factor, the ability of subjects to receive repeat procedures if requested. A higher proportion in Group II received multiple treatments (3.5 +/- 1.0 per year compared to 2.2 +/- 1.1 in the control group), which significantly biased the results to benefit the adhesiolysis group outcomes. The proportion of patients with at least 50% improvement in VAS pain score was greater at all time periods in Group II (90% vs. 35% at 3 months, 85% vs. 18% at 6 months, 73% vs. 12% at 12 months). Additionally, 73% of patients in the adhesiolysis group experienced at least 40% improvement in their ODI score at 12 months, compared to only 13% in the control group. The study was further weakened by multiple treatment variable differences between control and treatment groups. Groups differed in the use of a catheter to deliver medications (targeting) and the medications that were administered (0.9% vs 10% saline), thereby preventing more definitive conclusions from being drawn.
A later study by the same group investigated the role of LOA in patients with spinal stenosis [43]. Similar to the previous study, an ambulatory adhesiolysis procedure was compared to a control group that underwent a caudal ESI done without catheter-based adhesiolysis. 25 patients were randomized to each limb of the study. The results at one year follow-up revealed that significant pain relief (≥50%) was reported by 76% of patients in the adhesiolysis group, which favorably compared to a 4% success rate in the control group. Assessment with ODI at 12 months was also markedly in favor of adhesiolysis, with 80% of patients reporting at least 40% improvement, compared with 0% in the control group. A smaller number of procedures were performed in the control group (1.8 +/- 0.85) than in the adhesiolysis group (3.5 +/- 1.0). It is notable that the abysmally low success rate in the caudal group is inconsistent with other studies in similar cohorts [44], and the study suffers from the same design flaw, repeat procedures and multiple different interventions, as the earlier study [42] by the same group.
Generally positive results have also been noted in non-randomized studies. A large retrospective trial by Manchikanti et al. [17] conducted both ambulatory and two-day adhesiolysis protocols in a total of 129 patients. Results of the two protocols were compared to each other and to previously reported results with Racz's three-day protocol. Both treatments were associated with good short-term relief with no differences noted between protocols, though only 13% reported significant benefit at 12-month follow-up. Prospective studies that included patients with spinal stenosis [45], post-lumbar surgery pain [46], and those with radiculopathy of any etiology [47] have also reported good, long-term benefit.
Overall, a discrepancy exists among systematic reviews regarding the strength of the evidence for performing percutaneous adhesiolysis for either spinal stenosis or post-lumbar surgery pain [28,30]. As discussed in the most recent review [30], the overall evidence is fair for both spinal stenosis and post-lumbar pain using a 3-day or ambulatory protocol, though the strength of the conclusions and recommendations is hampered by the paucity of high-quality randomized studies and the lack of trials performed by a diversity of clinician investigators.
The efficacy of epidural LOA in the cervical region has recently been the subject of several studies, but randomized trials are lacking. Compared to procedures at the caudal or lumbar level, interventions performed in the cervical spine are associated with a higher complication rate [48,49], with the use of epidural catheters for adhesiolysis conferring possible additional risks [50].
A recent prospective study by Park et al. [51] details the performance of cervical LOA in 39 patients with central cervical stenosis. All patients had a reinforced navigable catheter inserted at T1-2 and advanced cephalad. The patients then received an initial 5 ml of a solution that contained local anesthetic, hyaluronidase and corticosteroid. One hour later, 6 ml of 10% saline was infused over 30 minutes and the catheter was removed. Follow-up was at 2 weeks and 6 months, and the sole outcome measure was a Roland 5-point patient satisfaction scale where 0 indicated no pain and 5 indicated unbearable pain. The results demonstrated improvement (no, little, or moderate pain) in 30 of 39 patients (77%) at 2 weeks and in 28 of 39 patients at 6 months. Three patients elected to have spinal surgery during the follow-up period. A significant weakness in this exploratory study is that baseline data was not reported, making it difficult to interpret follow-up data.
A retrospective study by Park et al. [52] evaluated the outcome of cervical LOA in 128 patients with cervical disc herniation. Inclusion criteria included the presence of refractory radicular pain, with patients who had a prior history of surgery excluded. Radiopaque epidural catheters were placed in all patients and advanced cephalad to the level of disc herniation. Adhesiolysis was then performed with an initial injection of 5 ml Hyaluronidase solution, followed by delivery of 5 ml of 0.2% ropivacaine with 5 mg of dexamethasone. Follow-up visits were performed through 12 months post-treatment. Twelve patients whose pain score remained greater than 50/100 received a cervical epidural steroid injection one month after adhesiolysis. Overall results showed significant improvement at all time periods for both arm (73.0 at baseline, 8.3 at 12 months) and neck pain (77.0 at baseline, 4.1 at 12 months). Functional improvement was also noted, with mean neck disability scores decreasing from a baseline of 17.5 to 2.3 at 12 month follow-up. No serious complications were reported at any time point. Although the evidence is weak, the available data suggests that some patients with spinal stenosis and disc herniation who have failed conservative therapy may benefit from cervical LOA.
A variant of LOA involves the use of a flexible spinal endoscope, or "epiduroscope", to deliver medication and mechanically lyse adhesions. Reported benefits of epiduroscopy include the ability to directly visualize epidural fibrosis [53], and determine the level of nerve root impingement [54] with greater accuracy than MRI. In theory these diagnostic attributes make epiduoscopy an ideal vehicle for adhesiolysis, but available evidence is primarily in the form of uncontrolled prospective studies.
A 2005 trial by Manchikanti et al. is the lone randomized controlled study dedicated to adhesiolysis via an endoscope [55]. The investigators randomized 50 patients with refractory low-back and leg pain into two groups: group 1 served as a control and received spinal endoscopy to the S3 level without adhesiolysis, and group 2 received spinal endoscopy with targeted adhesiolysis as cephalad as the L4 level. Provocative manipulation via the epiduroscope was used to confirm the affected spinal level. Adhesiolysis was then performed through the scope with normal saline of a volume less than 100 ml. Both groups received injection of 1% lidocaine (10 ml in group 1, 4-8 ml in group 2) and corticosteroid (1-2 ml of either betamethasone or methylprednisolone in each group). Follow-up at 3, 6, and 12 month included assessments of pain scores, functional capacity in the form of the ODI, work status and opioid intake. A significantly higher percentage of patients in the treatment group reported at least 50% pain relief at all time periods (90% vs. 33% at 1 mo, 48% vs. 0% at 12 months). Secondary measures including ODI and work status were also significantly improved in the treatment group at 12 month follow-up. Although this study showed superior benefit for adhesiolysis via an endoscope compared to caudal ESI, it did not compare adhesiolysis with and without epiduroscopy, and the results are similar to those obtained by this same group in their catheter-based adhesiolysis studies [42,43].
This comparison was made in an earlier 1999 retrospective trial by the same group that examined the outcomes of 120 patients with post-laminectomy pain who underwent adhesiolysis either without (group 1) or with (group 2) an epiduroscope [46]. Non-endoscopic adhesiolysis was performed via a catheter and involved targeted injection of local anesthetic, corticosteroid and 6 ml of normal saline. Endoscopic adhesiolysis added visualization and provocative confirmation of an affected nerve root, after which adhesiolysis was performed with normal saline (volume unspecified), corticosteroid and local anesthetic. Follow-up was obtained at 1, 3, 6, and 12 months. Overall, pain relief was shown to be superior in the endoscopic group, with more patients reporting at least 50% pain relief at all time periods (97% versus 72% at one month, 22% versus 7% at 12 months). Repeat procedures were allowed, and were more frequent in Group 1. Although retrospective, the study did demonstrate benefit for the use of endoscopy, although health-care costs were significantly higher with use of the scope and it suffers from the same methodological weakness as previous studies [42,43].
Adhesiolysis is mentioned briefly in the 2005 randomized trial by Dashfield et al. [56]. Although designed to compare caudal epidural steroid injections to targeted injections via epiduroscopy, it was a stated goal that adhesions encountered in the course of endoscopy would be broken down by saline or physical manipulation of the scope. Ultimately, adhesiolysis was performed in only 3 of the 27 patients in the epiduroscopy limb of the study, with no benefit noted with use of endoscopy.
Several smaller prospective studies have shown positive results and a lack of serious complications [57-60]. One study utilized an interlaminar approach and is notable for dural puncture in 4 of 19 patients (21.1%), one of whom required hospitalization [61].
The available evidence supports the safety of performing adhesiolysis via an endoscope. Regarding efficacy, there are no randomized studies comparing LOA with and without an endoscope, making it difficult to recommend in light of the increased cost and risks.
The results of trials that have examined the effectiveness of epidural LOA have been mixed, and strongly suggest there is a need for better patient selection and improved study design. Yet, few studies have examined the factors associated with outcomes of epidural LOA. In a large retrospective analysis by Hsu et al. conducted in 115 patients who underwent epidural LOA, the one variable that was most consistently associated with successful response in both univariate and multivariate analysis was age greater than 81 years [62]. A numeric rating score (NRS) <9 was also associated with a positive outcome. Paradoxically, patients seeking disability or worker's compensation were more likely to obtain a positive outcome in univariate analysis, while those with NRS pain scores >9 and in the age group between 41-50 years were more likely to experience a negative outcome. In clinical studies evaluating the influence secondary gain has on treatment outcomes for back pain in general, most but not all studies have found a negative effect [63]. No benefit was noted for either the use of a reinforced navigable catheter or the addition of hyaluronidase. In two retrospective studies evaluating the effectiveness of percutaneous adhesiolysis by Lee et al., a poor outcome was more common in patients with previous surgery, spondylolisthesis, herniated disc, and lumbosacral and foraminal stenosis [64,65]. An observational study by Park et al. performed in 66 patients with clinical spinal stenosis found no association between LOA outcome and the anatomical degree of stenosis [45].
Several studies have sought to determine whether epidural administration of hyaluronidase or hypertonic saline improves outcomes. One of the first studies to examine this was by Heavner et al., whereby 83 patients were assigned to receive hypertonic saline, normal saline, normal saline and hyaluronidase, or hypertonic saline and hyaluronidase [38]. All groups received local anesthetic and steroid during the epidural LOA. The authors found that although all groups experienced comparable improvement in pain, the 2 groups that received hypertonic saline required less number of treatments. Limitations in this study include a high percentage of dropouts (n = 24) and baseline differences between groups. The beneficial role of hyaluronidase in this study was unclear.
Another study reached different conclusions regarding the use of hyaluronidase. A small randomized study by Al-Maksoud Yousef et al. compared treatment outcomes in 38 subjects who received either fluoroscopically-guided caudal injections of 10 ml of 0.25% bupivacaine, 30 ml of 3% hypertonic saline and 80 mg of methyl-prednisolone, or the same mixture with 1,500 units of hyaluronidase added [66]. Although significant improvements in pain and functional were noted in both groups through 3-month follow-up, only those patients who received hyaluronidase continued to experience benefit at 6 and 12-months post-procedure. Two randomized studies conducted by the same group of investigators in patients with FBSS [67] and sciatica [68] compared high-volume interlaminar epidural injections with 5 ml 0.25% bupivacaine and 80 mg of triamcinolone; 5 ml of 0.25 % bupivacaine and 1,500 units of hyaluronidase; or a combination group that received bupivacaine, steroids and hyaluronidase. In both studies, greater improvement was noted in the group that received hyaluronidase and steroids than in those who received either drug alone. In summary, there is moderate evidence supporting the use of hypertonic saline in epidural lysis of adhesions, and weak positive evidence in favor of using hyaluronidase.
Although the question has not been formally addressed in randomized studies, there is evidence that a significant portion of the benefit for epidural LOA can be attributed to the high volumes injected. In a systematic review by Rabinovitch et al. [24], the investigators found a strong correlation between the volume of epidural injectate and pain relief irrespective of steroid dose in the immediate (≤6 weeks; r = 0.80, P = 0.002) and intermediate-term (3 months-1 year; r = 0.95; P = 0.014), and a trend towards significance in the short-term (6 weeks-3 months; r = 0.50; P = 0.17). The authors also found that when different volumes were injected in the 'control' and treatment arms, the effect size for ESI was 0.81, which was considerably larger than the effect size when the same volume was administered (0.07; P = 0.001). However, in two other studies [42,43], the injectate volume was kept constant and a significant difference between catheter adhesiolysis and a control, high-volume ESI was reported, suggesting a benefit related to either the use of a catheter, hypertonic saline or both interventions. The beneficial effect volume confers is likely constrained by a ceiling effect, as Hsu et al. found no differences in mean volumes injected in those subjects who experienced a positive results (mean 20.8 ml) and those with a negative outcome (20.2 ml) (Table 2) [62].
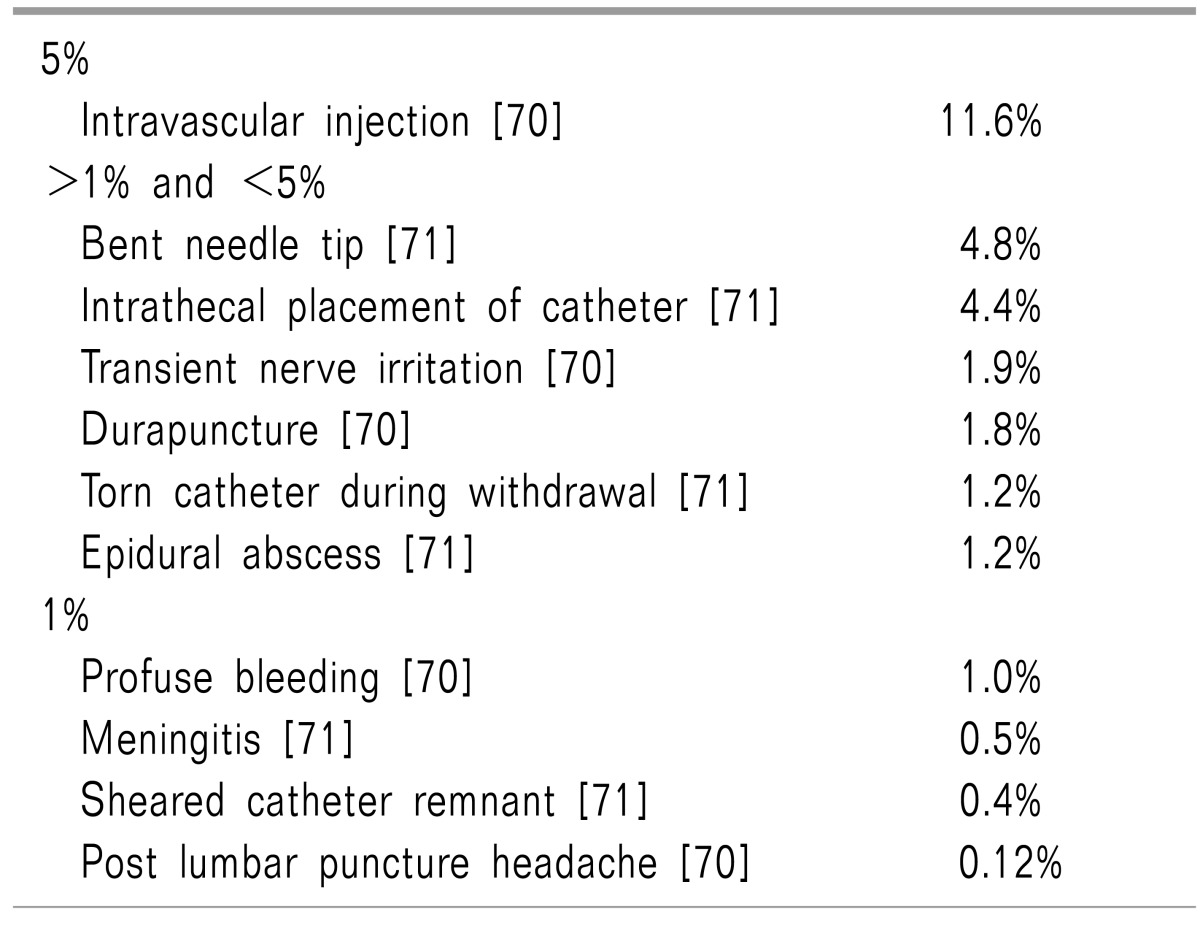
As for any procedural intervention, bleeding, infection, and nerve damage are some of the general complications associated with epidural LOA. The added risks associated with entering the epidural space include cerebral spinal fluid leakage and subsequent post-dural puncture headache, and neurological sequelae resulting from a hematoma or compression from large volume injectate administration. Entering the epidural space at the sacrococcygeal ligament and advancing a catheter up towards the area of pathology should theoretically reduce the incidence of inadvertent dural puncture. Although this has yet to be formally examined, it is likely that the development and risk of serious neurological complications resulting from hematoma formation may be less with a fluoroscopically-guided caudal approach, as the entry point into the epidural space is more superficial; the area is more compressible than in the lumbar and cervical spinal regions; and the nerve roots that innervate the lower extremities and most of the bowel and bladder are located more cephalad [69,70].
A number of large studies have examined the complications associated with epidural LOA. One retrospective review of 250 patients who underwent epidural neuroplasty revealed a variety of different complications such as a bent needle tip (4.8%), torn catheters during withdrawal (1.2%), sheared catheter remnant (0.4%), intrathecal placement of catheter (4.4%), and epidural abscess (1.2%) [71]. In another large study, a prospective evaluation of 10,000 epidural injections found that in the 839 patients who underwent adhesiolysis, the rates of intravascular injection (11.6%), transient nerve irritation (1.9%), and dural puncture (1.8%) were significantly higher than for conventional ESI [70]. The differences are likely related to the volume administered, needle size, catheter insertion and manipulation, since patients who received caudal epidural injections without adhesiolysis experienced much lower complication rates: intravascular injection (3.1%), transient nerve irritation (0.0%), and dural puncture (0.0%).
Smaller studies and case reports describing complications with epidural LOA are also worthy of mention. One case report from Germany described a case of severe meningitis, as well as a detailed review of other previously noted complications [72]. Another case report described a sheered and retained catheter after adhesiolysis [73]. The patient presented three months after the procedure with new onset radiculopathy documented by EMG. In a small prospective trial (N = 47), 15 patients developed transient sensory deficits including radicular numbness in the leg(s) [40]. The large volumes administered in a contained and often stenotic space during adhesiolysis theoretically increase the risk for cauda equina syndrome and other neurological sequelae stemming from nerve root compression, as was described in a case report on a patient who developed acute monoplegia that resolved after 5 days [74]. Endoscopic adhesiolysis has also been associated with development of neurogenic bladder [75].
An in-vitro study by Birkenmaier et al. examined the toxicity of commonly used injectates during epidural LOA [76]. The investigators employed an in-vitro fibroblast culture to simulate connective tissue and administered bupivacaine, hyaluronidase, triamcinolone, and hypertonic saline into the epidural space. The authors found that hypertonic saline and bupivacaine had time and concentration-dependent cytotoxic effects on fibroblasts at dosages well below what is normally injected during an epidural LOA. Steroids had a retarding effect on fibroblast proliferation, while hyaluronidase had no notable effect. Other toxicity studies also suggest a possible toxic effect for hypertonic saline when injected around neural tissue and other cell types [77,78]. Although these results cannot readily be extrapolated to clinical practice, they suggest that further toxicity studies should be conducted to better elucidate the long-term effects of adhesiolytic injectates (Table 3).
The evidence surrounding epidural LOA is still controversial. Although randomized studies seem to indicate that LOA is superior to conventional ESI and conservative therapy, many of these studies were conducted by the same groups of investigators and suffer from significant methodological flaws. Studies support ambulatory epidural LOA for FBSS, SS and radiculopathy refractory to less invasive procedures, with no randomized studies comparing percutaneous and endoscopic LOA.
One potential confounding factor is that the anatomical relationship between scar tissue and pain symptoms is not clear, with some, but not all studies demonstrating an association. The mechanisms of action for epidural LOA probably include the dissolution of scar tissue, the washout of inflammatory cytokines by high volume injectates, and the suppression of ectopic discharge from injured nerves.
Very little has been studied about the factors associated with outcomes for epidural LOA. Currently, the literature suggests that adhesion-targeting by high-volume injections and hypertonic saline may contribute to the beneficial effect of adhesiolysis, with weaker, conflicting evidence supporting hyaluronidase. Identifying the ideal patients and technique for epidural LOA is important, as larger, more methodologically sound studies that compare adhesiolysis to placebo, and to other treatments (i.e. comparative-effectiveness studies) are needed to better determine effectiveness.
ACKNOWLEDGEMENTS
Funded in part by the Centers for Rehabilitation Sciences Research, Uniformed Services University of the Health Sciences.
References
1. Nallegowda M, Chiravuri S. Re: Radcliff K, Kepler C, Hilibrand A, et al. Epidural steroid injections are associated with less improvement in patients with lumbar spinal stenosis: a subgroup analysis of the spine patient outcomes research trial. Spine (Phila Pa 1976). 2013;38:279-91. Spine (Phila Pa 1976). 2013; 38:1521. PMID: 23900112.
2. Cohen SP, Bicket MC, Jamison D, Wilkinson I, Rathmell JP. Epidural steroids: a comprehensive, evidence-based review. Reg Anesth Pain Med. 2013; 38:175–200. PMID: 23598728.
3. Pinto RZ, Maher CG, Ferreira ML, Hancock M, Oliveira VC, McLachlan AJ, et al. Epidural corticosteroid injections in the management of sciatica: a systematic review and meta-analysis. Ann Intern Med. 2012; 157:865–877. PMID: 23362516.

4. Manchikanti L, Pampati V, Falco FJ, Hirsch JA. Growth of spinal interventional pain management techniques: analysis of utilization trends and Medicare expenditures 2000 to 2008. Spine (Phila Pa 1976). 2013; 38:157–168. PMID: 22781007.
7. Wang MC, Kreuter W, Wolfla CE, Maiman DJ, Deyo RA. Trends and variations in cervical spine surgery in the United States: Medicare beneficiaries, 1992 to 2005. Spine (Phila Pa 1976). 2009; 34:955–961. PMID: 19352223.
8. Verbiest H. Pathomorphologic aspects of developmental lumbar stenosis. Orthop Clin North Am. 1975; 6:177–196. PMID: 1113966.

9. Bolender NF, Schönström NS, Spengler DM. Role of computed tomography and myelography in the diagnosis of central spinal stenosis. J Bone Joint Surg Am. 1985; 67:240–246. PMID: 3968115.

10. Verbiest H. The significance and principles of computerized axial tomography in idiopathic developmental stenosis of the bony lumbar vertebral canal. Spine (Phila Pa 1976). 1979; 4:369–378. PMID: 483044.

11. De Villiers PD, Booysen EL. Fibrous spinal stenosis. A report on 850 myelograms with a water-soluble contrast medium. Clin Orthop Relat Res. 1976; (115):140–144. PMID: 1253477.
12. Roberson GH, Llewellyn HJ, Taveras JM. The narrow lumbar spinal canal syndrome. Radiology. 1973; 107:89–97. PMID: 4689450.

13. Fanuele JC, Birkmeyer NJ, Abdu WA, Tosteson TD, Weinstein JN. The impact of spinal problems on the health status of patients: have we underestimated the effect? Spine (Phila Pa 1976). 2000; 25:1509–1514. PMID: 10851099.
14. Kalichman L, Cole R, Kim DH, Li L, Suri P, Guermazi A, et al. Spinal stenosis prevalence and association with symptoms: the Framingham Study. Spine J. 2009; 9:545–550. PMID: 19398386.

15. Racz GB, Holubec JT. Lysis of adhesions in the epidural space. In : Racz GB, editor. Techniques of neurolysis. Boston (MA): Kluwer Academic;1989. p. 57–72.
16. Racz GB, Heavner JE, Diede JH. Lysis of epidural adhesions utilizing the epidural approach. In : Waldman SD, Winnie AP, editors. Interventional pain management. Philadelphia (PA): WB Saunders;1996. p. 339–351.
17. Manchikanti L, Pakanati RR, Bakhit CE, Pampati V. Role of adhesiolysis and hypertonic saline neurolysis in management of low back pain: evaluation of modification of the Racz protocol. Pain Dig. 1999; 9:91–96.
18. Kuslich SD, Ulstrom CL, Michael CJ. The tissue origin of low back pain and sciatica: a report of pain response to tissue stimulation during operations on the lumbar spine using local anesthesia. Orthop Clin North Am. 1991; 22:181–187. PMID: 1826546.
19. Ross JS, Robertson JT, Frederickson RC, Petrie JL, Obuchowski N, Modic MT, et al. ADCON-L European Study Group. Association between peridural scar and recurrent radicular pain after lumbar discectomy: magnetic resonance evaluation. Neurosurgery. 1996; 38:855–861. PMID: 8692415.

20. Maroon JC, Abla A, Bost J. Association between peridural scar and persistent low back pain after lumbar discectomy. Neurol Res. 1999; 21(Suppl 1):S43–S46. PMID: 10214571.

21. Almeida DB, Prandini MN, Awamura Y, Vitola ML, Simião MP, Milano JB, et al. Outcome following lumbar disc surgery: the role of fibrosis. Acta Neurochir (Wien). 2008; 150:1167–1176. PMID: 18936878.

22. Rönnberg K, Lind B, Zoega B, Gadeholt-Göthlin G, Halldin K, Gellerstedt M, et al. Peridural scar and its relation to clinical outcome: a randomised study on surgically treated lumbar disc herniation patients. Eur Spine J. 2008; 17:1714–1720. PMID: 18946688.

23. Jarvik JG, Deyo RA. Diagnostic evaluation of low back pain with emphasis on imaging. Ann Intern Med. 2002; 137:586–597. PMID: 12353946.

24. Rabinovitch DL, Peliowski A, Furlan AD. Influence of lumbar epidural injection volume on pain relief for radicular leg pain and/or low back pain. Spine J. 2009; 9:509–517. PMID: 19398387.

25. Trescot AM, Chopra P, Abdi S, Datta S, Schultz DM. Systematic review of effectiveness and complications of adhesiolysis in the management of chronic spinal pain: an update. Pain Physician. 2007; 10:129–146. PMID: 17256027.
26. Chopra P, Smith HS, Deer TR, Bowman RC. Role of adhesiolysis in the management of chronic spinal pain: a systematic review of effectiveness and complications. Pain Physician. 2005; 8:87–100. PMID: 16850047.
27. Racz GB, Heavner JE, Trescot A. Percutaneous lysis of epidural adhesions--evidence for safety and efficacy. Pain Pract. 2008; 8:277–286. PMID: 18503627.

28. Epter RS, Helm S 2nd, Hayek SM, Benyamin RM, Smith HS, Abdi S. Systematic review of percutaneous adhesiolysis and management of chronic low back pain in post lumbar surgery syndrome. Pain Physician. 2009; 12:361–378. PMID: 19305485.
29. Belozer M, Wang G. Epidural adhesiolysis for the treatment of back pain: health technology assessment. Olympia (WA): Washington State Department of Labor & Industries;2004.
30. Helm Ii S, Benyamin RM, Chopra P, Deer TR, Justiz R. Percutaneous adhesiolysis in the management of chronic low back pain in post lumbar surgery syndrome and spinal stenosis: a systematic review. Pain Physician. 2012; 15:E435–E462. PMID: 22828693.
31. Hegmann KT. American College of Occupational and Environmental Medicine. Occupational medicine practice guidelines: evaluation and management of common health problems and functional recovery in workers. 3rd ed. Elk Grove Village (IL): American College of Occupational and Environmental Medicine;2011.
32. Tran de QH, Duong S, Finlayson RJ. Lumbar spinal stenosis: a brief review of the nonsurgical management. Can J Anaesth. 2010; 57:694–703. PMID: 20428988.

33. Chou R, Huffman LH. Guideline for the evaluation and management of low back pain: evidence review. Glenview (IL): American Pain Society;2009.
34. Manchikanti L, Datta S, Gupta S, Munglani R, Bryce DA, Ward SP, et al. A critical review of the American Pain Society clinical practice guidelines for interventional techniques: part 2. Therapeutic interventions. Pain Physician. 2010; 13:E215–E264. PMID: 20648212.
35. Manchikanti L, Singh V, Derby R, Helm S 2nd, Trescot AM, Staats PS, et al. Review of occupational medicine practice guidelines for interventional pain management and potential implications. Pain Physician. 2008; 11:271–289. PMID: 18523500.
36. Chou R, Manchikanti L. American Pain Society (APS) low back pain guidelines: A pro/con debate. In : Presented at the American Academy of Pain Medicine's 27th Annual Meeting; 2011 Mar 24-7; National Harbor (MD). Chicago (IL): American Pain Society;2011.
37. American Society of Anesthesiologists Task Force on Chronic Pain Management. American Society of Regional Anesthesia and Pain Medicine. Practice guidelines for chronic pain management: an updated report by the American Society of Anesthesiologists Task Force on Chronic Pain Management and the American Society of Regional Anesthesia and Pain Medicine. Anesthesiology. 2010; 112:810–833. PMID: 20124882.
38. Heavner JE, Racz GB, Raj P. Percutaneous epidural neuroplasty: prospective evaluation of 0.9% NaCl versus 10% NaCl with or without hyaluronidase. Reg Anesth Pain Med. 1999; 24:202–207. PMID: 10338168.

39. Manchikanti L, Rivera JJ, Pampati V, Damron KS, McManus CD, Brandon DE, et al. One day lumbar epidural adhesiolysis and hypertonic saline neurolysis in treatment of chronic low back pain: a randomized, double-blind trial. Pain Physician. 2004; 7:177–186. PMID: 16868590.
40. Veihelmann A, Devens C, Trouillier H, Birkenmaier C, Gerdesmeyer L, Refior HJ. Epidural neuroplasty versus physiotherapy to relieve pain in patients with sciatica: a prospective randomized blinded clinical trial. J Orthop Sci. 2006; 11:365–369. PMID: 16897200.

41. Gerdesmeyer L, Wagenpfeil S, Birkenmaier C, Veihelmann A, Hauschild M, Wagner K, et al. Percutaneous epidural lysis of adhesions in chronic lumbar radicular pain: a randomized, double-blind, placebo-controlled trial. Pain Physician. 2013; 16:185–196. PMID: 23703406.
42. Manchikanti L, Singh V, Cash KA, Pampati V, Datta S. A comparative effectiveness evaluation of percutaneous adhesiolysis and epidural steroid injections in managing lumbar post surgery syndrome: a randomized, equivalence controlled trial. Pain Physician. 2009; 12:E355–E368. PMID: 19935992.
43. Manchikanti L, Cash KA, McManus CD, Pampati V, Singh V, Benyamin R. The preliminary results of a comparative effectiveness evaluation of adhesiolysis and caudal epidural injections in managing chronic low back pain secondary to spinal stenosis: a randomized, equivalence controlled trial. Pain Physician. 2009; 12:E341–E354. PMID: 19935991.
44. Manchikanti L, Cash KA, McManus CD, Pampati V, Fellows B. Results of 2-year follow-up of a randomized, double-blind, controlled trial of fluoroscopic caudal epidural injections in central spinal stenosis. Pain Physician. 2012; 15:371–384. PMID: 22996849.
45. Park CH, Lee SH, Jung JY. Dural sac cross-sectional area does not correlate with efficacy of percutaneous adhesiolysis in single level lumbar spinal stenosis. Pain Physician. 2011; 14:377–382. PMID: 21785481.
46. Manchikanti L, Pampati V, Bakhit CE, Pakanati RR. Non-endoscopic and endoscopic adhesiolysis in post-lumbar laminectomy syndrome: a one-year outcome study and cost effectiveness analysis. Pain Physician. 1999; 2:52–58. PMID: 16906216.
47. Gerdesmeyer L, Lampe R, Veihelmann A, Burgkart R, Göbel M, Gollwitzer H, et al. Chronic radiculopathy. Use of minimally invasive percutaneous epidural neurolysis according to Racz. Schmerz. 2005; 19:285–295. PMID: 15549419.
48. Brouwers PJ, Kottink EJ, Simon MA, Prevo RL. A cervical anterior spinal artery syndrome after diagnostic blockade of the right C6-nerve root. Pain. 2001; 91:397–399. PMID: 11275398.

49. Rozin L, Rozin R, Koehler SA, Shakir A, Ladham S, Barmada M, et al. Death during transforaminal epidural steroid nerve root block (C7) due to perforation of the left vertebral artery. Am J Forensic Med Pathol. 2003; 24:351–355. PMID: 14634474.

50. Asano M, Akatsuka M, Uda R, Son H, Nagano Y, Tatsumi T. Suspected migration of cervical epidural catheter into the brainstem after a difficult catheter insertion. J Anesth. 2013; [in press].

51. Park CH, Lee SH, Lee SC. Preliminary results of the clinical effectiveness of percutaneous adhesiolysis using a Racz catheter in the management of chronic pain due to cervical central stenosis. Pain Physician. 2013; 16:353–358. PMID: 23877451.
52. Park EJ, Park SY, Lee SJ, Kim NS, Koh do Y. Clinical outcomes of epidural neuroplasty for cervical disc herniation. J Korean Med Sci. 2013; 28:461–465. PMID: 23487574.

53. Bosscher HA, Heavner JE. Incidence and severity of epidural fibrosis after back surgery: an endoscopic study. Pain Pract. 2010; 10:18–24. PMID: 19735365.

54. Bosscher HA, Heavner JE. Diagnosis of the vertebral level from which low back or leg pain originates. A comparison of clinical evaluation, MRI and epiduroscopy. Pain Pract. 2012; 12:506–512. PMID: 22429715.

55. Manchikanti L, Boswell MV, Rivera JJ, Pampati VS, Damron KS, McManus CD, et al. [ISRCTN 16558617] A randomized, controlled trial of spinal endoscopic adhesiolysis in chronic refractory low back and lower extremity pain. BMC Anesthesiol. 2005; 5:10. PMID: 16000173.
56. Dashfield AK, Taylor MB, Cleaver JS, Farrow D. Comparison of caudal steroid epidural with targeted steroid placement during spinal endoscopy for chronic sciatica: a prospective, randomized, double-blind trial. Br J Anaesth. 2005; 94:514–519. PMID: 15695544.

57. Richardson J, McGurgan P, Cheema S, Prasad R, Gupta S. Spinal endoscopy in chronic low back pain with radiculopathy. A prospective case series. Anaesthesia. 2001; 56:454–460. PMID: 11350333.

58. Geurts JW, Kallewaard JW, Richardson J, Groen GJ. Targeted methylprednisolone acetate/hyaluronidase/clonidine injection after diagnostic epiduroscopy for chronic sciatica: a prospective, 1-year follow-up study. Reg Anesth Pain Med. 2002; 27:343–352. PMID: 12132057.

59. Igarashi T, Hirabayashi Y, Seo N, Saitoh K, Fukuda H, Suzuki H. Lysis of adhesions and epidural injection of steroid/local anaesthetic during epiduroscopy potentially alleviate low back and leg pain in elderly patients with lumbar spinal stenosis. Br J Anaesth. 2004; 93:181–187. PMID: 15194631.

60. Sakai T, Aoki H, Hojo M, Takada M, Murata H, Sumikawa K. Adhesiolysis and targeted steroid/local anesthetic injection during epiduroscopy alleviates pain and reduces sensory nerve dysfunction in patients with chronic sciatica. J Anesth. 2008; 22:242–247. PMID: 18685930.

61. Avellanal M, Diaz-Reganon G. Interlaminar approach for epiduroscopy in patients with failed back surgery syndrome. Br J Anaesth. 2008; 101:244–249. PMID: 18552347.

62. Hsu E, Atanelov L, Plunkett AR, Chai N, Chen Y, Cohen SP. Epidural lysis of adhesions for failed back surgery syndrome and spinal stenosis: factors associated with treatment outcome. Anesth Analg. 2014; 118:215–224. PMID: 24356168.

63. Harris I, Mulford J, Solomon M, van Gelder JM, Young J. Association between compensation status and outcome after surgery: a meta-analysis. JAMA. 2005; 293:1644–1652. PMID: 15811984.

64. Lee JH, Lee SH. Clinical effectiveness of percutaneous adhesiolysis and predictive factors of treatment efficacy in patients with lumbosacral spinal stenosis. Pain Med. 2013; [in press].

65. Lee JH, Lee SH. Clinical effectiveness of percutaneous adhesiolysis using Navicath for the management of chronic pain due to lumbosacral disc herniation. Pain Physician. 2012; 15:213–221. PMID: 22622905.
66. Yousef AA, EL-Deen AS, Al-Deeb AE. The role of adding hyaluronidase to fluoroscopically guided caudal steroid and hypertonic saline injection in patients with failed back surgery syndrome: a prospective, double-blinded, randomized study. Pain Pract. 2010; 10:548–553. PMID: 20412501.

67. Kim SB, Lee KW, Lee JH, Kim MA, An BW. The effect of hyaluronidase in interlaminar lumbar epidural injection for failed back surgery syndrome. Ann Rehabil Med. 2012; 36:466–473. PMID: 22977771.

68. Kim SB, Lee KW, Lee JH, Kim MA, Kim BH. The additional effect of hyaluronidase in lumbar interlaminar epidural injection. Ann Rehabil Med. 2011; 35:405–411. PMID: 22506151.

69. Wong GK, Arab AA, Chew SC, Naser B, Crawford MW. Major complications related to epidural analgesia in children: a 15-year audit of 3,152 epidurals. Can J Anaesth. 2013; 60:355–363. PMID: 23296493.

70. Manchikanti L, Malla Y, Wargo BW, Cash KA, Pampati V, Fellows B. A prospective evaluation of complications of 10,000 fluoroscopically directed epidural injections. Pain Physician. 2012; 15:131–140. PMID: 22430650.
71. Talu GK, Erdine S. Complications of epidural neuroplasty: a retrospective evaluation. Neuromodulation. 2003; 6:237–247. PMID: 22151070.

72. Wagner KJ, Sprenger T, Pecho C, Kochs EF, Tölle TR, Berthele A, et al. Risks and complications of epidural neurolysis -- a review with case report. Anasthesiol Intensivmed Notfallmed Schmerzther. 2006; 41:213–222. PMID: 16636945.
73. Perkins WJ, Davis DH, Huntoon MA, Horlocker TT. A retained Racz catheter fragment after epidural neurolysis: implications during magnetic resonance imaging. Anesth Analg. 2003; 96:1717–1719. PMID: 12761003.

74. Ho KY, Manghnani P. Acute monoplegia after lysis of epidural adhesions: a case report. Pain Pract. 2008; 8:404–407. PMID: 18721177.

75. Justiz R, Taylor V, Day M. Neurogenic bladder: a complication after endoscopic adhesiolysis with return of bladder function while using nitrofurantoin. Anesth Analg. 2010; 110:1496–1498. PMID: 20304983.
76. Birkenmaier C, Redeker J, Sievers B, Melcher C, Jansson V, Mayer-Wagner S. An evaluation of medications commonly used for epidural neurolysis procedures in a human fibroblast cell culture model. Reg Anesth Pain Med. 2011; 36:140–144. PMID: 21270726.

77. Pribor DB, Nara A. The effect of salt or various cryoprotective agents on frog sciatic nerves. Cryobiology. 1973; 10:33–44. PMID: 4541020.

78. Svendsen O, Edwards CN, Lauritzen B, Rasmussen AD. Intramuscular injection of hypertonic saline: in vitro and in vivo muscle tissue toxicity and spinal neurone c-fos expression. Basic Clin Pharmacol Toxicol. 2005; 97:52–57. PMID: 15943759.

Fig. 1
Sequential antero-posterior fluoroscopic images demonstrating successful epidural lysis of adhesions. (A) Arrow A illustrates the initial contrast injection demonstrating needle entry into the caudal canal. Arrow B shows the radiopaque navigable catheter inserted to the level of hardware at lumbar spine. (B) Initial contrast injection demonstrating filling defects on the left side and cephalad to the hardware, suggesting epidural adhesions. (C) Contrast reinjection after lysis of adhesions demonstrating improved spread cephalad (A) and to the left (B) of the initial injection pattern.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download