Abstract
Background
Nucleoplasty is a minimally invasive spinal surgery using a Coblation® technique that creates small voids within the disc. The purpose of this study was to evaluate the efficacy of cervical nucleoplasty in patients with cervical disc disorder.
Methods
Between March 2008 and December 2009, 22 patients with cervical disc disorders were treated with cervical nucleoplasty after failed conservative treatment. All procedures were performed under local anesthesia, and fluoroscopic guidance and voids were created in the disc with the Perc™ DC Spine Wand™. Clinical outcomes were evaluated by the Modified Macnab criteria and VAS score at preprocedure, postprocedure 1 month, and 6 months.
Results
Six patients had one, eight patients had two and eight patients had three discs treated; a total of 46 procedures was performed. Mean VAS reduced from 9.3 at preprocedure to 3.7 at postprocedure 1 month and to 3.4 at postprocedure 6 months. There was no significant complication related to the procedure within the first month. Outcomes were good or excellent in 17/22 (77.3%) cases. Postprocedure magnetic resonance imaging was acquired in two patients after two months showing morphologic evidence of volume reduction of protruded disc material in one patient but not in the other.
Clinically, cervical disc disorders frequently cause cervical axial pain, radiculopathy, and myelopathy. This kind of pain from the intervertebral disc is known to be caused by mechanical compression from extruded disc material, accompanying inflammatory response, and released chemical mediators [1].
Generally, for this kind of cervical disc disorder, conservative treatment such as orthosis, cervical traction, and medication are carried out first. However, if symptoms persist or increase in severity after 6-8 weeks of sufficient conservative treatment, then surgical treatment is considered. Although surgical treatment is relatively well established and known to be highly successful, it has many drawbacks such as damage to the adjacent tissue (bone, muscle, nerves, and blood vessels), chronic loading to adjacent discs which results in damage and transformation, and a long postoperative recovery period [1]. To supplement these drawbacks, MIST (Minimally Invasive Spinal Techniques) have been developed and performed for several years [1,2].
Among these, nucleopasty was developed by Arthro- Care Corporation in the United States, approved by the U.S. Food and Drug Administration in 1999, and first performed in July of 2000. At first, Nucleopasty was developed and used to treat contained lumbar disc herniation and protrusion with associated symptoms [1,2]. Sharps and Isaac [3] and Singh et al. [4] reported significant pain reduction for up to a year after percutaneous disc decompression using lumbar nucleoplasty. However, compared to other percutaneous decompression or even lumbar nucleoplasty, there is a relative lack of research on and clinical experience with cervical nucleoplasty. Cervical nucleoplasty has only limited evidence (level IV) in the literature concerning the technique like lumbar nucleoplasty, and indications are limited to contained herniation and protrusion similar to the lumbar area [1,2,5]. Therefore, the goal of this study is to evaluate on the efficacy, side effects and patient satisfaction with cervical nucleoplasty performed on patients with cervical disc disorders that were unresponsive to conservative treatments.
This study was conducted on 22 patients with cervical disc disorders who were treated with cervical nucleoplasty between March 2008 and December 2009 at our hospital. The study was approved by the hospital's medical research ethics committee, and written informed consent was obtained from all patients before the nucleoplasty.
Patients were treated with nucleoplasty after confirmation for the existence of cervical disc disorders related to the patients' subjective symptoms on the basis of systemic review, physical examination, X-ray studies and magnetic resonance imaging (MRI) examination. Physical examination including neurological examination before the surgery was carried out by the same pain physician. There were no neurological deficits, such as loss of sensory, motor or reflex in any of the patients, but they all complained of just pain. All patients had a simple radiological study and MRI examination done at least once to confirm the existence of cervical disc disorder. The mean time period from onset of symptoms to the nucleoplasty was 25 months, and there had been no improvement despite conservative pain management including medication, physical therapy, and root blocks. All nucleoplasty was conducted by the same pain physician.
Before entering the operating theater, 1,000 ml of Hartman's solution was connected after intravenous cannulation, and the patient received intravenous injection of 1.0 g of cefazolin as a prophylactic antibiotic 1 hour before the procedure after confirmation of a negative skin test. The patient was placed in supine position on the operation table, and to facilitate access to the cervical disc, a thin surgical roll was placed under the neck so that it was slightly hyperextended. The patient received the vital sign monitoring and oxygen supply at 5 L per minute via nasal prong throughout the procedure. All procedures were performed under local anesthesia, but midazolam 2-4 mg was administered for sedation if there was a patient's demand. Betadine soap and betadine solution were used to disinfect the anterior neck as well as surrounding skin, and sterilized drapes were applied on the operating area.
First, the C-arm was positioned in a lateral view of the surgical field to measure the angle of the target disc (endplate angle). Then, the C-arm was positioned in an antero-posterior (AP) view to confirm the target disc and rotated axially to align the endplate at measured angle in the prior lateral projection. Before the procedure, we measured the position and angle of the herniated part from the center of the disc with MRI examination. According to this measured angle, the C-arm was tilted obliquely on the opposite side to the patient's symptoms, and the needle entry point was marked with a surgical marker on the anterior neck relevant to the center of the disc to be treated. The paratracheal approach was used in the opposite site to the patient's symptom. After the internal carotid artery was laterally displaced with the surgeon's index and middle fingers, the needle entry site was secured. Then, the needle was introduced in the needle entry point and advanced till the anterolateral annulus fibrosus. A syringe filled with 5 ml of 2% lidocaine was connected to the needle, and the local anesthetic was administered from the disc to the skin while checking that blood was not aspirated with repeated suction and injection. Next, we used the paratracheal approach again. After the patient's internal carotid artery was displaced laterally and the needle puncture site was secured, a 19 gauge 3 inch Introducer needle (ArthroCare Co., Sunnyvale, CA, USA) was introduced in the needle entry point and advanced until it reached the annulus fibrosus. At this point, the AP and lateral views were gained to see if the introducer needle tip was in contact with the center of the disc height. Then, the oblique view was obtained to see that the introducer needle was directed toward the center of the intervertebral disc and to guide the estimated progression route. The introducer needle entry angle at the anterolateral border of annulus fibrosus was then adjusted if needed. After the introducer needle was advanced slightly deeper, C-arm fluoroscope images were obtained again to see whether the introducer needle was placed in the center of the disc according to the AP and lateral views. The stylet of the introducer needle was withdrawn, and the Perc™ DC Spine Wand™ (ArthroCare co., Sunnyvale, CA, USA) was replaced and fastened clockwise to the needle hub. In the fastened state, the Perc™ DC Spine Wand™ and introducer needle were advanced slightly more to the estimated lesion site. Here, it should not go past the imaginary line beyond that connects the posterior vertebral bodies in lateral view (Fig. 1). Next, the Perc™ DC Spine Wand™ was connected to the ArthroCare system 2000® (ArthroCare Co., Sunnyvale, CA, USA), and coagulation was tested with the radio-frequency controller set at 2' for 1-2 seconds to check that there was no movement or paresthesia in the patient's upper limbs. Coblation® was then carried out to remove the nucleus pulposus. By rotating the flange 180°, we ablated the disc material - depending on the size and hardness of the lesion - for 20-60 seconds with the radio-frequency controller set at 2'-3' of intensity. After this, the wand was slightly retreated under the C-arm fluoroscope guidance, and coagulation proceeded with controller set at 3'. When it was verified that there was no movement or paresthesia in the patient's upper extremities, the flange was rotated 180° and ablation was done for 20-60 seconds with controller set at 3' or 4'. If the patient complained of abnormal pain during the ablation, the needle tip was slightly retreated and started from coagulation stage again to check nerve stimulation. The number of voids, duration and intensity of ablation were adjusted to the size and hardness of the protruded disc material. After the procedure, the patient took an absolute bed rest in the supine position for 4 hours. And an intravenous injection of 1.0 g of cefazolin was administered again as a prophylactic antibiotic. Six hours after the procedure, systemic symptoms were checked and neurological examination was performed to make sure there were no abnormalities. When the patients' status improved, they were discharged home with the instructions outlining post-surgery precautions and contact numbers for any enquiries that they might have. Patients visited the outpatient clinic 1 month and 6 months post-op for observation.
Clinical improvement after nucleoplasty was assessed with a VAS (visual analogue scale) recorded at preprocedure, postprocedure 1 month, and 6 months. Overall patient satisfaction on clinical outcome was defined 'excellent', 'good', 'fair', 'poor', or 'worse' according to the Modified MacNab criteria. Follow up MRI examination were not performed in all patients due to financial problems. Postprocedure MRI examinations were performed at the 2 months follow up in only 2 patients who did show clinical improvement.
The statistical analyses were performed using PASW (PASW Statistics 17.0, SPSS Inc., Chicago, IL, USA). The individual data are expressed as mean ± SD. The Wilcoxon signed rank test was used to compare results of nucleoplasty at preprocedure, postprocedure 1 month, and 6 months. The level of statistical significance was set at P < 0.05.
Of the 22 patients, the gender distribution was 15 male and 7 female. The age of patients ranged from 19 to 71 years (mean 47.8 ± 11.9 years) (Table 1).
At the first presentation, 9 patients complained of a dominant radicular pain, 4 of a dominant axial pain, and 9 of similar degree of axial and radicular pain. According to the MRI reading by the radiologist, disc protrusion was demonstrated in 17 patients, extrusion in 2, and stenosis in 3. Disc disorders proven on the MRI were encountered in our study at 4 disc levels, including C3-4 (n = 6), C4-5 (n = 12), C5-6 (n = 14), and C6-7 (n = 14). For the proven disc disorders, 6 patients received the nucleoplasty treatment at 1 level, 8 at 2 levels, 8 at 3 levels; therefore, the mean number of disc that received nucleoplasty treatment was 2.1 ± 0.8 level (Table 1). The nucleoplasty was successfully carried out on all discs, and there were no abnormal side effects.
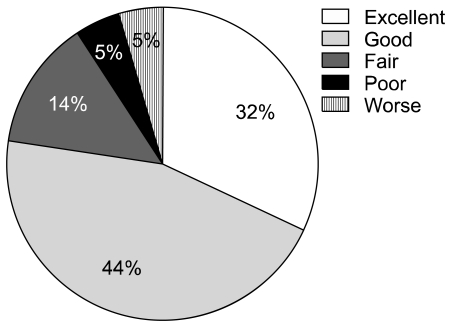
The preprocedure mean VAS score was 9.3 ± 0.9 and the mean VAS score improved to 3.7 ± 2.1 at postprocedure 1 month, and 3.4 ± 2.3 at postprocedure 6 months. There were statistically significant differences in VAS scores at preprocedure and postprocedure 1 month (P < 0.05) (Fig. 2). The clinical outcomes of the nucleoplasty according to the Modified MacNab criteria about the patient satisfaction with improvement in quality of life, pain and general symptoms were as follows: results were expressed 'excellent' or 'good' in 17 patients (76%), 'fair' in 3 (14%), 'poor' in 1 (5%), and 'worse' in 1 patient (5%). Therefore, most patients satisfied with the clinical results (Fig. 3). The patients not satisfied with the clinical results were all patients who had discs treated on more than 2 disc levels. However, from the 6 patients who had been treated on only 1 level, 3 patients expressed 'excellent' and the other 3 graded their clinical improvement as 'good'. Two months after the procedure, an MRI study was carried out in 2 patients who had shown clinical improvement. In one of them, there was significant reduction of protruded disc material, while in the other it was not significant (Fig. 4, 5).
Nucleoplasty is a percutaneous disc decompression using radiofrequency energy. Bipolar radiofrequency coagulation denaturalizes proteoglycan and changes the internal environment of the diseased nucleus pulposus; especially, the organic molecules (collagen and collagen like long chain molecules) inside the disc is changed to liquid or gaseous state, which is absorbed and removed at the target site [2]. Chen et al. proved that the decompression using Coblation® technique decreased the pressure in the disc with an experiment in a cadaveric specimen [6]. The advantage of the Coblation® technique used in nucleoplasty is that exceptionally precise and targeted removal is possible while minimizing the thermal injury to the surrounding tissue [7].
In proceeding with cervical nucleoplasty, the selection of a suitable patient is the most important. When Birnbaum's recommendations [8] and indications of lumbar nucleoplasty are considered, they are as follows [5,9,10]: 1) In the case of lateral herniation, presence of radicular/ axial pain while arm pain is severe than neck pain, MRI evidence of contained herniation, and failure of conservative treatment. 2) In the case of central herniation, presence of axial neck pain, unresponsive to 3 months of conservative treatment, MRI evidence of contained herniation, and the disc height more than 75%. Exclusion criteria include that the disc height less than 50%, extruded or sequestrated disc, spinal fracture or tumor, spinal stenosis, complete disruption of the annulus fibrosis, central myelopathy, instability from degeneration, and extrusion more than 1/3 of the spinal canal.
Nardi et al. [1] argued that patient who can be a candidate for cervical nucleoplasty must have contained herniation or focal bulging proven on MRI, but Bonaldi et al. [2] reported that the cervical nucleoplasty was performed in the patients who had a bulging, protruding, or soft extruded disc which was not sequestrated or migrated determined by MRI or CT studies. In our study, we performed cervical nucleoplasty on patients showing extrusion and stenosis in addition to protrusion on their MRI; who had no improvement from more than 3 months of conservative treatment including appropriate pain management; who keenly want non-surgical treatment over surgical treatment; and after adequate explanation on the possibility of failure, possible side-effects and costs of nucleoplasty. In MRI studies taken before the procedure, only 17 patients from the total 22 patients had disc protrusion suitable for indications, and from the 5 patients who had non-indication, 2 patients showed extrusion while the other 3 patients showed degenerative spinal stenosis. From these patients who had disc extrusion, one expressed 'excellent' according to the Modified McNab criteria after the cervical nucleoplasty and the other one was also satisfied and expressed 'good'. From the 3 patients who had degenerative spinal stenosis, one expressed 'excellent while the other 2 expressed 'fair'. Considering these results, although more clinical experience should be accumulated, nucleoplasty could be considered in disc disorders like soft disc extrusions and stenosis prior to surgical treatment if the patient wants non-surgical treatment; however, cautious application of cervical nucleoplasty should be taken after consideration of cost and possible side-effects [5].
In this study, postprocedure MRI studies were acquired in 2 patients who had shown clinical improvement after 2 months follow up. MRI study in one patient showed a morphologic evidence of volume reduction of protruded disc material but the other did not. Nardi et al. [1] had reported that regression of the herniated disc shown on the MRI has a correlation with clinical resolution, but Bonaldi et al. [2] reported that clinical improvement did not always accompany the regression of the herniated disc on MRI. Even in cases where there seems to be no regression of the herniated disc material, a minute reduction in the disc adjacent to the nerve root can cause nerve root pressure to fall below the critical point. If the postprocedure MRI had been acquired in all patients, we could have gained more information from the results. However, it was not possible due to the economic circumstances of the patients.
Few side effects concerning the cervical nucleoplasty have been reported and no serious side effects have been known. Side effects reported in the study of Bonaldi et al. [2] included 1 case of infectious discitis out of 55 patients, temporary side effects related to local anesthetic (bradycardia, Horner's syndrome, hoarseness, etc.), and retrosternal and retropharyngeal pain in patients treated on 3 levels but they responded well to conservative treatment [11,12]. There was no significant complication related to the procedure within the first month in our study.
Nardi et al. [1] and Birnbaum [8] had proven the efficacy of nucleoplasty by comparing the cervical nucleoplasty group and the conservative treatment group. Bonaldi et al. [2] performed cervical nucleoplasty on 55 patients and reported that it was successful in 85% of them. Li et al. [13] reported that 83.73% from the 126 patients treated reported 'excellent' or 'good' according to the MacNab criteria. In our study, 76% of the patients expressed satisfaction by answering 'good' or 'excellent'. These results of cervical nucleoplasty appear to be much better than the results of lumbar nucleoplasty [3,4,7]. However, the reasons that the nucleoplasty treatment may be more effective at the cervical level than at the lumbar level are not clear. One possible explanation could be anatomic: The cervical nerve root is confined to a relatively smaller space than its lumbar counterpart so the cervical nerve root respond more sensitively to even a minute reduction. For this reason, even if the pressure of the disc is reduced slightly, the decompression on the nerve root and reduction in clinical symptoms can be easily obtained. Another reason could be the topography of the lesion and direction from which it is approached for treatment. In lumbar nucleoplasty, we use a posterolateral approach from the lesion. But in cervical nucleoplasty, we use anterolateral approach to the disc, and so, the SpineWand™ could be accurately positioned in the lesion site posteriorly located. In other words, since symptomatic herniation is directed posterior, cervical nucleoplasty can effectively approach the lesion site because it uses the anterior approach [2,5].
Another benefits of cervical nucleoplasty are that it does not have any influence on the stability of the cervical vertebrae compared to surgical treatment [13]; it is minimally invasive since it uses a 19-gauge introducer needle, which is smaller compared to other percutaneous decompression; the Perc™ DC™ SpineWand that is handled by the surgeon is small and hard so it could be operated more precisely; it only takes a 10-12 minutes to treat one level of disc; and there is a markedly low possibility of damage to the surrounding tissue [5,8].
Upon retrospective examination of the medical records of the 22 patients that were treated in our hospital, clinical improvement in symptoms within a month after cervical nucleoplasty were seen in most patients. Most of the patients reported the reduced subjective symptoms, such as radicular and axial pain, and an improved quality of life. Consequently, they expressed satisfaction with the cervical nucleoplasty.
In conclusion, in the treatment of cervical disc disorders, cervical nucleoplasty is minimally invasive, easy and has fewer complications than the surgical treatment. Therefore, when there is no response to conservative treatment, cervical nucleoplasty can be considered as a suitable alternative prior to open surgical treatment. However, to obtain good clinical results, appropriate selection of patients according to the indications of nucleoplasty must precede the procedure, and more experience and research should be accumulated for other indications such as extrusion and stenosis.
References
1. Nardi PV, Cabezas D, Cesaroni A. Percutaneous cervical nucleoplasty using coblation technology. Clinical results in fifty consecutive cases. Acta Neurochir Suppl. 2005; 92:73–78. PMID: 15830972.

2. Bonaldi G, Baruzzi F, Facchinetti A, Fachinetti P, Lunghi S. Plasma radio-frequency-based diskectomy for treatment of cervical herniated nucleus pulposus: feasibility, safety, and preliminary clinical results. AJNR Am J Neuroradiol. 2006; 27:2104–2111. PMID: 17110676.
3. Sharps LS, Isaac Z. Percutaneous disc decompression using nucleoplasty. Pain Physician. 2002; 5:121–126. PMID: 16902662.

4. Singh V, Piryani C, Liao K, Nieschulz S. Percutaneous disc decompression using coblation (nucleoplasty) in the treatment of chronic discogenic pain. Pain Physician. 2002; 5:250–259. PMID: 16902650.
5. Ro JY, Oh CS, Kim OS, Kim DK, Woo NS, Shin HY. Nucleoplasty in a patient with cervical disc extrusion with radiating pain of an upper extremity. Anesth Pain Med. 2009; 4:203–207.
6. Chen YC, Lee SH, Chen D. Intradiscal pressure study of percutaneous disc decompression with nucleoplasty in human cadavers. Spine. 2003; 28:661–665. PMID: 12671352.

7. Boswell MV, Trescot AM, Datta S, Schultz DM, Hansen HC, Abdi S, et al. Interventional techniques: evidence-based practice guidelines in the management of chronic spinal pain. Pain Physician. 2007; 10:7–111. PMID: 17256025.
8. Birnbaum K. Percutaneous cervical disc decompression. Surg Radiol Anat. 2009; 31:379–387. PMID: 19190848.

9. Calisaneller T, Ozdemir O, Karadeli E, Altinors N. Six months post-operative clinical and 24 hour post-operative MRI examinations after nucleoplasty with radiofrequency energy. Acta Neurochir (Wien). 2007; 149:495–500. PMID: 17431536.

11. Bhagia SM, Slipman CW, Nirschl M, Isaac Z, El-Abd O, Sharps LS, et al. Side effects and complications after percutaneous disc decompression using coblation technology. Am J Phys Med Rehabil. 2006; 85:6–13. PMID: 16357543.

12. Oh WS, Park YO, Shim WS, Wie HW, Woo CH. Psoas abscess and discitis after intradiscal nucleoplasty. Korean J Anesthesiol. 2002; 42:844–849.

13. Li J, Yan DL, Zhang ZH. Percutaneous cervical nucleoplasty in the treatment of cervical disc herniation. Eur Spine J. 2008; 17:1664–1669. PMID: 18830638.

Fig. 1
Intraoperative fluoroscopic imaging. PercTM DC Spine WandTM placement adjacent to the lesion sites within the C5-6 intervertebral disc level during ablation. (A) Antero-posterior views. (B) Oblique views. (C) Lateral views.

Fig. 2
Pain intensity at the baseline and 1, 6 months of a follow-up period after the cervical nucleoplasty. Mean ± C.I (Confidence interval). P < 0.05.

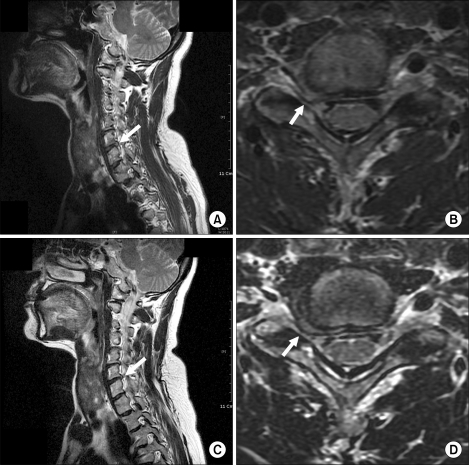
Fig. 4
Pre- and post-nucleoplasty Magnetic Resonance Imaging for a 29-year-old man. Preoperative sagittal (A) and axial (B) images show the disc protrusion with mild cord indentation at C5-6 intervertebral disc level. Postoperative sagittal (C) and axial (D) images show the volume reduction of protruded intervertebral disc segment.
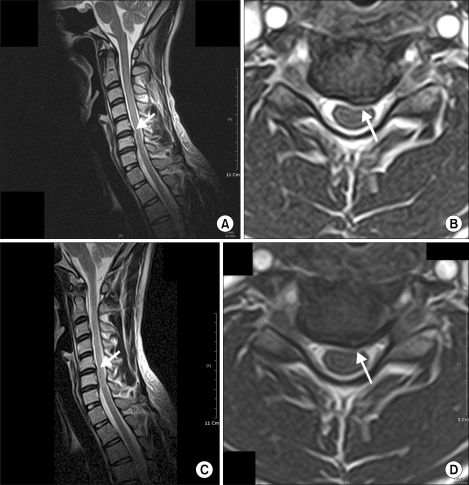
Fig. 5
Pre- and post-nucleoplasty Magnetic Resonance Imaging for a 65-year-old woman. Preoperative sagittal (A) and axial (B) images show the disc protrusion causing right neural for aminal stenosis at C6-7 intervertebral disc level. Postoperative sagittal (C) and axial (D) images do not show the evident volume reduction of protruded intervertebral disc segment.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download