Abstract
Spontaneous intracranial hypotension (SIH) is considered to be a very rare disorder. It is characterized by an orthostatic headache that is aggravated with the patient in the upright position and it is relieved by the patient assuming the supine position. SIH is caused by a spontaneous spinal cerebrospinal fluid leakage without the patient having undergone trauma, surgery or dural puncture or having any other significant medical history. An autologous epidural blood patch (EBP) is effective in relieving SIH. We report here on a case of SIH with cerebrospinal fluid leakage at the upper cervical vertebral level and the middle thoracic vertebral level. The points of leakage were identified by radionuclide cisternography, and this patient was successfully managed by injecting an EBP at each level of leakage.
Spontaneous intracranial hypotension (SIH) is a rare disease that occurs in 5 out of every 100,000 people [1]. It is characterized by an orthostatic headache in the absence of a past history of a trauma or a dural puncture [2-5]. Conservative treatment for this condition usually includes bed rest, applying a abdominal binder, hydration, and the administration of caffeine, theophylline and steroids [2,3]. However, when the patient is refractory to the conservative treatment, an epidural blood patch (EBP) is performed [2-5]. An EBP is known to be an effective treatment for SIH because it immediately alleviatives this disorder [2-6]. Berroir et al. [6] reported that performing an EBP 1-2 times cured SIH in 77% of the patients in their study. However, Lee et al. [4] saw a patient whose pain persisted even after performing an EBP 3 times because the patient had multilevel CSF leaks. Schievink [7] stated that the patients with normal MRI findings and diffuse multilevel CSF leaks have a poor prognosis of being unresponsive. We performed radionuclide cisternography (RNC) on a patient who was suffering from OH and we discovered multilevel CSF leaks in both the cervical and the thoracic levels. We will present and discuss this case for which we performed EBPs on both levels simultaneously and this successfully alleviated his pain.
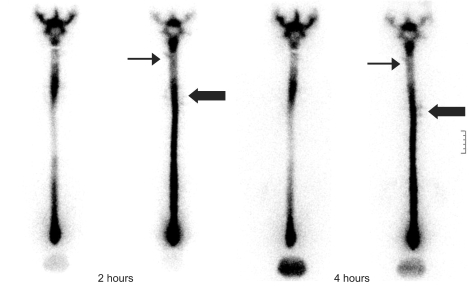
A 55-year old male patient was admitted for the occipital and frontal headaches he had suffered with for the previous 7 days before admission to the hospital. They occurred after he had lifted heavy objects. The headaches occurred when he sat or stood up, but they subsided when he was lying down. He had received no treatment for this, but 3 days before admission, his headaches had worsened. On the day he was admitted, he experienced dull pain of 8/10 on the VAS in the occipital and frontal areas, as well as in the cervical area, and this was accompanied by nausea. So he visited the department of neurosurgery as an outpatient and was admitted. There were no strange findings in his past history. He had no past history of trauma or dural puncture in the head or spine. A physical examination performed on the day he was admitted showed no strange findings either. But a brain MRI showed he had diffuse pachymeningeal enhancement and a subdural effusion (Fig. 1). A CSF study showed the CSF opening pressure in the sitting position to be 40 mmH2O, there was increased protein at 64.5 mg/dl and the glucose level was 59 mg/dl. A cytologic examination of the CSF and a bacterial culture test showed no strange findings. Spinal MRI showed a dilated epidural venous plexus. An RNC showed that the CSF leaked to the left at the cervical level and to the right at the middle thoracic level. It also showed that the radioactive tracer was quickly being excreted through the bladders and kidneys (Fig. 2). These findings were diagnosed to be a CSF leak/SIH in the cervical and thoracic levels. Conservative treatment was administered for 2 days, including liberal hydration, bed rest and the administration of NSAIDs. But when standing, his pain persisted at 8/10 on the VAS. So he was referred to the Department of Pain for consultation. On day 3 of admission, 6 ml of autologous EBP was injected under fluoroscopic guidance between C4 and C5, as well as 6 ml of autologous EBP was injected between T5 and T6. The patient experienced immediate pain relief. 8 hours after the EBP, his pain was 2/10 on the VAS. On day 4 of admission, the pain was 0/10 on the VAS. On the second brain MRI, there was little change in the pachymeningeal enhancement, but the subdural effusion had decreased. He experienced no headaches afterwards. So on day 6, he was discharged. He was still asymptomatic at the 3 month follow up, and he is still being monitored.
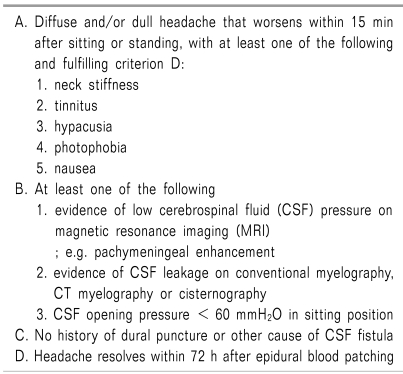
According to the International Classification of Headache Disorders II (ICHD-II), SIH is a diffuse and/or dull headache that worsens within 15 min after sitting or standing. The symptoms are neck stiffness, tinnitus, hypacusia, photophobia and nausea. It occurs in the absence of dural puncture or any cause for a CSF fistula. The brain MRI findings include at least one or more of the following: evidence of low cerebrospinal fluid pressure on magnetic resonance imaging, evidence of a CSF leak on conventional myelography, CT myelography or cisternography, or a CSF opening pressure < 60 mmH2O in the sitting position. Also, the headache resolves within 72 h after epidural blood patching (Table 1) [8].
SIH is considered to be caused by a CSF leak [2-6,,10]. A CSF leak occurs in weak areas around the dura mater and nerve root sheaths and around small defects (such as an epidural cyst or diverticulum) due to a small trauma, fall down, severe exercise or cough tearing the dura or arachnoid [4]. Schievink [7] stated that connective tissue disorders such as the Marfan syndrome, Ehlers-Danlos syndrome type 2 and autosomal dominant polycystic kidney disease play a big role in causing SIH. Hyun et al. [10] conducted a study on 30 SIH patients, and the results showed their average age was 43 and 70% of them (21/30) were women. SIH predominately occurs in women in their 40s and at the thoracic spine level and cervico-thoracic junction [2,7].
SIH is characterized by OH in the frontal and occipital areas [2-6]. It may be accompanied by symptoms of nausea, vomiting, neck stiffness, neck pain, diplopia, photophobia, anorexia, tinnitus, dizziness, facial numbness and fatigue. The headache may worsen due to laughter, cough, jugular compression and the valsalva maneuver [6,7].
The mechanism of the OH is not clear. Sagging of the brain due to decreased CSF pressure while standing causes the pain-sensitive structures to stretch in the cranial vault, such as the dura mater, the cranial nerves (vagus nerves, glossopharyngeal nerves, trigeminal nerves), the upper cervical nerves and the bridging veins. It also causes the meningeal vessels to experience compensatory dilatation [2,3].
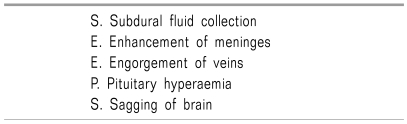
SIH can be diagnosed by taking a proper history, radiologic study and measuring the CSF pressure [8]. A brain MRI using gadolinium is the diagnostic study of choice and this allows making an early diagnosis [10]. The characteristic imaging findings of brain MRI are a subdural fluid collection, enhancement of the pachymeninges, engorgement of veins and pituitary hyperemia. They occur as compensatory mechanisms for the decreased CSF pressure.
Sagging of the brain may also occur due to the decrease in CSF buoyancy (Table 2) [11]. Enhancement of the pachymeninges was previously considered to be the most critical finding for making the diagnosis of SIH, but it has recently been discovered that 20% of SIH patients do not have this [12]. Moreover, many other diseases have been found to cause pachymeningeal enhancement such as infectious diseases (tuberculosis, fungal infection, lyme's disease, syphilis and HTLV), colleagen vascular diseases (rheumatoid arthritis, SLE and complex connective tissue diseases), neoplasia (multifocal fibrosclerosis, carcinoma, lymphoma and meningioma en plaque) and miscellaneous disorders (sarcoidosis, hemodialysis and intrathecal drug administration) [13].
When SIH is suspected on a brain MRI, the leak site can be found by performing RNC, CT myelography or spinal MRI [2,10]. The findings that are indicative of SIH on a spinal MRI are meningeal enhancement, dilatation of the epidural venous plexus and an extra-arachnoid fluid collection [9,12]. For our case, we found a dilated epidural venous plexus. Direct and indirect signs of CSF leaks can be found on RNC. A direct sign of a CSF leak is the radioactive tracer progressing into the extra-arachnoid space. An indirect sign is that the radioactive tracer can be quickly seen in the bladder and kidneys. This is because the CSF leaked through the dura mater circulates in the epidural venous plexus [10]. On the RNC that Hyun et al. [10] conducted on 30 SIH patients, 27 showed indirect signs and 24 showed direct signs. When performing RNC on patients with a CSF leak does not help to find the direct leak site, it is because the tracer's movement is limited by low CSF pressure. The CSF leak site can be more easily found when the valsalva maneuver is performed by the standing patient. When the RNC does not lead to finding the leak, CT myelography could be more helpful. Because of its higher sensitivity, performing CT myelography is better for finding CSF leaks than performing RNC and spinal MRI [12]. We were able to find the leak in the cervical and thoracic levels in our patient by performing RNC, so we did not have to perform further tests.
When SIH patients are in the sitting position, their CSF pressure is low at 60 mmH2O or below [2,12]. A CSF study may appear normal or it will show increased protein, RBCs and WBCs. This is because there is a difference in pressure between the venous sinus and arachnoid villus, and because protein, RBCs and WBCs flow from the blood vessels into the CSF through the meningeal perforation [2,4,5].
When SIH is diagnosed by performing the above mentioned tests and the CSF leak site is discovered, many different types of treatment can be performed. Complete recovery generally occurs with conservative measures such as bed rest and increasing the patient's hydration [2,3]. Bed rest decreases the pressure in the CSF leak-site, and this allows the meningeal defect to heal. Venous injection of caffeine is effective in 70% of the patients with postdural puncture headache (PDPH) because caffeine is an adenosine receptor antagonist [14]. This is also often chosen as the first treatment for SIH. As it blocks the adenosine receptors, it decreases the intracranial blood flow and venous engorgement. Second, it decreases the headache by stimulating CSF production [14]. Theophylline also has the same effect as an adenosine receptor antagonist [2]. However, EBP may be performed when conservative treatments fail [2-6]. Mokri [15] explained an EBP has two mechanisms that are involved in relieving the headache. The primary immediate headache-relief occurs when the blood inflow presses the dura mater and creates volume replacement. The secondary long-lasting relief is achieved because the blood inflow seals the leak. Schievink [7] believed that blood injected into the epidural space restricts the CSF flow and blocks CSF absorption, leading to symptomatic relief.
The amount of blood injected in SIH patients has varied in different reports. Jung et al. [16] reported on using 12-40 ml in the lumbar spine level, 11-20 ml in the thoracic spine level and 6-13 ml in the cervico-thoracic junction. However, Kim et al. [3] argued that a large amount of blood injected in the epidural space increases the potential for complications such as an epidural infection, infectious meningitis, archnoiditis and muscle weakness. Thus, using a small amount of blood very sparingly in the accurately determined CSF leak sites can decrease the possibility of complications. Performing an EBP on SIH patients for whom conservative treatment had failed has shown persistent symptomatic relief in 56-77% of the cases [6]. The success rate of an EBP for treating SIH is lower than that for PDPH treatment. This is because the CSF leak site has not been properly found, and so sometimes the EBP is performed in an inappropriate location, or the CSF leak is in the anterior aspect of the dural sac or the nerve root sleeve. Moreover, there is a structural difference between a dural puncture-caused hole and a SIH leak site [15]. Lee et al. [4] performed an EBP on a SIH patient 3 times, but the patient continued to complain of headache. So, they performed an RNC and found multilevel CSF leaks in the low lumbar spine level and the cervico-thoracic junction. After performing an 8-12 ml EBP 5 more times in the lumbar spine level, the patient experienced relief of symptoms. Park et al. [5] also performed EBPs 10 times on a patient with multilevel CSF leaks before symptomatic relief was achieved. If a patient has multilevel leaks and the sites are far apart, performing an EBP in only one site may bring symptomatic relief because of the effect of immediate fluid-replenishment. However, it will have no sealing effect on all the leak sites, so the continuous CSF leakage will cause the symptoms to recur. Therefore, the exact site of the SIH leak in the patient should be found before performing an EBP. A multilevel CSF leak may be suspected after performing an EBP 1-2 times with no symptom improvement. When an RNC shows a multilevel CSF leak, performing EBPs near each site of the leak simultaneously has proven to be effective. If the CSF leak is at the anterior aspect of the dural sac or the nerve root sleeve, performing an EBP with the transforaminal approach rather than the interlaminar approach is recommended, although further study on this is still needed.
When an EBP fails to manage the pain, percutaneous placement of fibrin sealant may be tried [17]. Surgical treatment may be performed when the patient is refractory to all attempted treatments [15], and surgical treatment is relatively safe for a CSF leak site and this can be done for treating patients with structural abnormalities [15].
For our patient with multilevel CSF leaks in both the cervical level and the thoracic level, RNC found the leak site and we then performed EPBs on them simultaneously. Using a small amount of blood was instantaneously effective. It allowed for long-lasting pain management and for treating the multilevel SIH, and all this makes our very interesting case noteworthy to share.
References
1. Schievink WI, Maya MM, Moser F, Tourje J, Torbati S. Frequency of spontaneous intracranial hypotension in the emergency department. J Headache Pain. 2007; 8:325–328. PMID: 18071632.

2. Zaatreh M, Finkel A. Spontaneous intracranial hypotension. South Med J. 2002; 95:1342–1346. PMID: 12540006.

3. Kim KS, Lee DI, Kang WJ, Shin OY, Kwon MI. A case of cervical epidural blood patch for treatment of spontaneous intracranial hypotension. Korean J Pain. 2002; 15:198–203.
4. Lee JI, Roh JH, Yoon DM, Lee YW. Spontaneous intracranial hypotension and epidural blood patch: a case report. Korean J Anesthesiol. 2005; 48:216–219.

5. Park JH, Yoon DM, Lee YC, Kim WO, Yoon KB. 10 times epidural blood patches for spontaneous intracranial hypotension: a case report. Korean J Pain. 2005; 18:60–63.

6. Berroir S, Loisel B, Ducros A, Boukobza M, Tzourio C, Valade D, et al. Early epidural blood patch in spontaneous intracranial hypotension. Neurology. 2004; 63:1950–1951. PMID: 15557521.

7. Schievink WI. Spontaneous spinal cerebrospinal fluid leaks. Cephalalgia. 2008; 28:1345–1356. PMID: 19037970.

8. Headache Classification Subcommittee of the International Headache Society. The international classification of headache disorders: 2nd edition. Cephalalgia. 2004; 24(Suppl 1):8–160. PMID: 15595989.
9. Mokri B, Posner JB. Spontaneous intracranial hypotension: the broadening clinical and imaging spectrum of CSF leaks. Neurology. 2000; 55:1771–1772. PMID: 11134370.

10. Hyun SH, Lee KH, Lee SJ, Cho YS, Lee EJ, Choi JY, et al. Potential value of radionuclide cisternography in diagnosis and management planning of spontaneous intracranial hypotension. Clin Neurol Neurosurg. 2008; 110:657–661. PMID: 18457913.

11. Schievink WI, Maya MM, Louy C. Cranial MRI predicts outcome of spontaneous intracranial hypotension. Neurology. 2005; 64:1282–1284. PMID: 15824366.

12. Sainani NI, Lawande MA, Pungavkar SA, Desai M, Patkar DP, Mohanty PH. Spontaneous intracranial hypotension: a study of six cases with MR findings and literature review. Australas Radiol. 2006; 50:419–423. PMID: 16981936.

13. Mokri B, Hunter SF, Atkinson JL, Piepgras DG. Orthostatic headaches caused by CSF leak but with normal CSF pressures. Neurology. 1998; 51:786–790. PMID: 9748027.

14. Camann WR, Murray RS, Mushlin PS, Lambert DH. Effects of oral caffeine on postdural puncture headache. A double-blind, placebo-controlled trial. Anesth Analg. 1990; 70:181–184. PMID: 2405733.
15. Mokri B. Headaches caused by decreased intracranial pressure: diagnosis and management. Curr Opin Neurol. 2003; 16:319–326. PMID: 12858068.

16. Jung IS, Choe H, Han YJ, Son JS. Spontaneous intracranial hypotension treated with epidural blood patch: a case report. Korean J Anesthesiol. 2005; 49:581–584.

17. Schievink WI, Maya MM, Moser FM. Treatment of spontaneous intracranial hypotension with percutaneous placement of a fibrin sealant. Report of four cases. J Neurosurg. 2004; 100:1098–1100. PMID: 15200130.

Fig. 1
Axial enhanced T1-weighted magnetic resonance imaging shows typical change of spontaneous intracranial hypotension with pachymeningeal enhancement (arrow) in a 55-year-old man with multiple spontaneous spinal cerebrospinal fluid leakage.
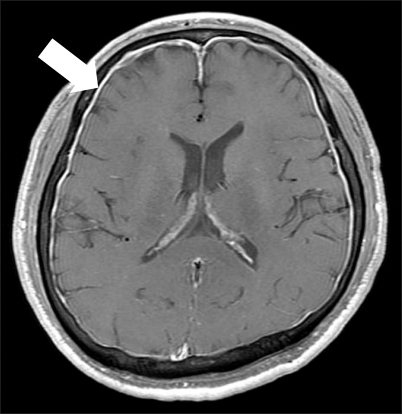
Fig. 2
Radionuclide cisternography shows cerebrospinal fluid leakage at upper cervical vertebral level (thin arrow) and middle thoracic vertebral level (thick arrow).




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download