Abstract
Background
Complications following lumbar transforaminal epidural injection are frequently related to inadvertent vascular injection of corticosteroids. Several methods have been proposed to reduce the risk of vascular injection. The generally accepted technique during epidural steroid injection is intermittent fluoroscopy. In fact, this technique may miss vascular uptake due to rapid washout. Because of the fleeting appearance of vascular contrast patterns, live fluoroscopy is recommended during contrast injection. However, when vascular contrast patterns are overlapped by expected epidural patterns, it is hard to distinguish them even on live fluoroscopy.
Methods
During 87 lumbar transforaminal epidural injections, dynamic contrast flows were observed under live fluoroscopy with using digital subtraction enhancement. Two dynamic fluoroscopy fluoroscopic images were saved from each injection. These injections were performed by five physicians with experience independently. Accuracy of live fluoroscopy was determined by comparing the interpretation of the digital subtraction fluoroscopic images.
Results
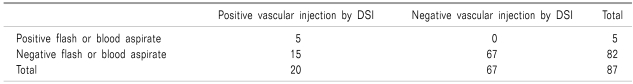
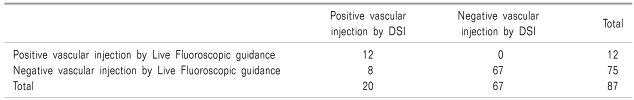
Using digital subtraction guidance with contrast confirmation, the twenty cases of intravascular injection were found (the rate of incidence was 23%). There was no significant difference in incidence of intravascular injections based either on gender or diagnosis. Only five cases of intravascular injections were predicted with either flash or aspiration of blood (sensitivity = 25%). Under live fluoroscopic guidance with contrast confirmation to predict intravascular injection, twelve cases were predicted (sensitivity = 60%).
Lumbar transforaminal epidural steroid injections (ESIs) are frequently employed for the treatment of lower back pain with a radicular component secondary to lumbar disc pathology, degenerative condition of the lumbar spine or failed back surgery syndrome [1-3]. The mechanism of therapeutic benefit is attributed to relieving the inflammation secondary to mechanical and/or chemical nerve root irritation [4-6]. Transforaminal epidural injections of anesthetic and corticosteroids are generally safe with a reported minor complication rate of 9.6% in the lumbar spine [7]. Rare but serious morbidity has also been documented including: transient paraplegia, spinal cord infarction with myelopathy, subdural hematoma, cerebellar infarct, and death [8-12]. Many of these adverse outcomes are thought to be secondary to inadvertent intravascular injection and embolization of corticosteroid particles via the vertebral artery or the radiculomedullary arteries [10-13].
The reported incidence of inadvertent vascular injection is 9% to 26% in intermittent fluoroscopically guided transforaminal epidural injections depending on the level of injection [14,15]. Because of the fleeting appearance of a vascular contrast pattern, prior studies have recommended observation of dynamic contrast flow under live fluoroscopy. However, when vascular contrast patterns are overlapped by expected epidural patterns, it is hard to distinguish them even on live fluoroscopy. These simultaneous epidural and vascular injections are the most common type of inadvertent vascular injection with an incidence of 8.9% in lumbosacral injections [16]. Therefore, the addition of digital subtraction may enhance visualization of contrast distribution and vascular uptake during injection [17,18]. The purpose of this study is to determine how accurately live fluoroscopy detects inadvertent intravascular injection during lumbosacral transforaminal epidural injections using dynamic contrast flow under digital subtraction fluoroscopy as the gold standard.
A total of 87 lumbosacral transforaminal ESIs performed on 46 patients. All patients were included who were thought to be appropriate candidate for a transforaminal lumbosacral ESIs during a 5-month period (June through October 2009) to treat either lumbar disc pathology or spinal stenosis. Patients receiving either interlaminar or caudal ESIs were excluded, as were patients who were pregnant or had known allergies to contrast dye, iodine, fish, or shellfish. If the authors considered the needle placement difficult and needed multiple attempts, the cases were excluded from the study.
All procedures were performed under fluoroscopic guidance with contrast enhancement by five physicians with experience. The patients were prepared and draped in a sterile fashion in a prone position. For lumbar transforaminal ESIs, the fluoroscope was positioned so that an oblique view of the appropriate neural foramen was obtained. The overlying soft tissue was then anesthetized with 1% lidocaine. An appropriate length styleted 22-gauge needle was guided inferior to the pars interarticularis and into the neural foramen. Under biplanar visualization, the needle was advanced into the "safe triangle" inferior to the pedicle, and superolateral to the exiting spinal nerve, thus avoiding nerve, dorsal root ganglion, and dural sleeve puncture. For S1 transforaminal injection, the 22-gauge needle was guided into the superior lateral quadrant of the S1 foramen using biplanar fluoroscopy.
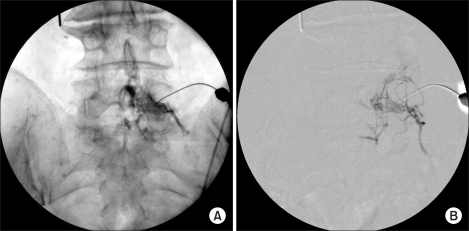
After all levels and the ideal needle position were confirmed by biplanar fluoroscopy, the presence or absence of flash and/or aspiration in the needle and syringe were observed and documented. Subsequently, 1.0 ml of nonionic contrast was injected under live fluoroscopy with using digital subtraction enhancement. Two dynamic fluoroscopic images, live fluoroscopic images and digital subtraction fluoroscopic images were saved from each injection (Fig. 1). If there was vascular spread, the needle was repositioned. Data were collected prospectively, including the patient's age, sex and diagnosis. Statistical evaluation was then performed on the above data including χ2 test, Fisher exact test, McNemar test, sensitivity and specificity (SPSS Version 17.0) to determine the significance of the findings.
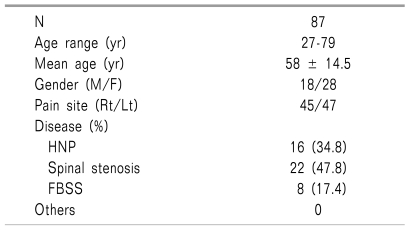
Eighty-seven lumbosacral transforaminal ESIs performed on 46 patients (mean age, 58 years; range, 27-79 years) were recorded. Sixty lumbar and 27 S1 transforaminal ESIs were performed. Of those, 47 cases (54%) were left-sided injections, and 40 cases (46%) were right-sided injections (Table 1).
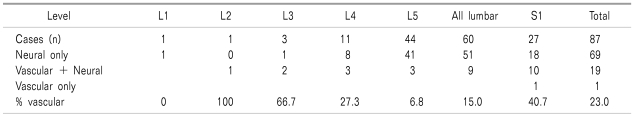
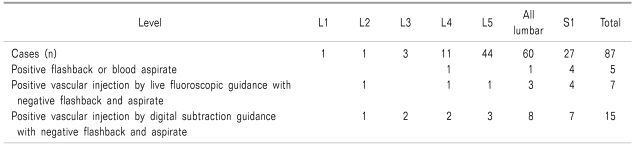
Using digital subtraction guidance with contrast confirmation, our overall rate of intravascular injection was 23% (n = 20). Transforaminal ESIs performed at S1 had an intravascular injection rate of 40.7% (n = 11) compared with 15.0% (n = 9) for all the lumbar injections (Table 2). There was no significant difference in the incidence of intravascular injections by diagnosis in patients with post-spine surgery (33.3%) compared with those with none spine surgery (21.3%; Fisher exact test, P value = 0.460). There was also no significant difference in incidence of intravascular injections based on gender (19.6% female; 29.0% male; Fisher exact test, P value = 0.425). Although there were 20 documented vascular injections, only 5 of these were predicted with either a flash or aspiration of blood (sensitivity = 25%). The 67 nonvascular injections were predicted by a negative flash and negative blood aspiration in 67 (Table 3, 4).
There were 20 documented vascular injections, 12 cases were predicted under live fluoroscopic guidance with contrast confirmation (sensitivity = 60%). False positive vascular response (indicating a vascular pattern was present on a live fluoroscopic image when not documented in the digital subtraction image) was not observed (Table 5).
In this prospective study of 87 injections, the incidence of intravascular injections during lumbosacral transforaminal ESIs as determined by digital subtraction fluoroscopic guidance was 23% overall. Transforaminal ESIs performed at S1 had an intravascular injection rate of 40.7% (n = 11) compared with 15.0% (n = 9) for all the lumbar injections (Table 2). There was a statistically significant higher intravascular injection rate at S1 compared with the lumbar levels. The higher intravascular injection rate at S1 may be contributed to increased vascularity in the sacral foraminal region. The sample was too small in the individual lumbar levels to make statistically significant conclusion about incidence of vascular injection at each level.
The majority of these vascular injections are venous. The vertebral venous plexus is a valveless system that extends to the entire length of the vertebral column, and is confluent with the venous systems of the lower limb and pelvis caudally and with the dural sinuses cranially [19,20]. The vertebral venous system can be divided into three intercommunicating divisions:
The internal posterior vertebral venous plexus within the epidural space is located predominately dorsolaterally, which must be avoided during injections. The serious morbidity associated with transforaminal injection is thought to be caused primarily by inadvertent arterial injection and embolization of corticosteroid particles [20-24]. Although the risks are greater with intra-arterial injection, intravenous injections should also be avoided. The reason is that partial or total intravenous administration of the corticosteroids is contrary purpose of epidural injection: to place a high concentration of the medication at the site of pathology. To avoid inadvertent vascular injection, several methods have been suggested including: aspiration with a syringe, dynamic observation of live fluoroscopy during contrast injection, digital subtraction angiography, usage of short bevelled or blunt needles, and an application of an anesthetic test dose.
Furman et al. reported that using a positive flash or blood aspirate to predict intravascular injections during lumbar transforaminal ESIs was 44.7% sensitive by comparing with intermittent fluoroscopy [15]. In this study, we found that flash or blood aspiration was 25% sensitive by comparing with digital subtraction fluoroscopic guidance. Thus, a positive flash or aspiration of blood was only predictive of intravascular injection in a quarter of the documented vascular injections. The negative pressure for aspiration may result in the collapse of the vessel, thus preventing blood uptake. Therefore, this method is clearly unreliable. Although only transforaminal lumbosacral ESIs were investigated, the implication of this finding extends throughout interventional pain management. In our study, the authors found that flash or blood aspiration was 100% specific. Although a negative flash or blood aspiration is unreliable, a positive flash or blood aspiration reliably predicts a vascular injection, and the needle tip should be repositioned.
During the process of contrast injecting, intermittent fluoroscopic spot filming is inadequate for visualizing vascular uptake. Matthew et al. reported that intermittent fluoroscopy missed the vascular uptake in more than 50% of simultaneous epidural and vascular injection [14]. Based on these prior studies, live fluoroscopy is recommended during contrast injection. Our study showed that the intravascular injections were found in 12 cases of 87 cases under live fluoroscopic guidance with contrast confirmation (13.8%). It also observed that using digital subtraction guidance with contrast confirmation, the intravascular injection occurred in 20 cases of the 87 cases (23%). There was a statistically significant higher rate of intravascular injections noted with transforaminal ESIs performed under digital subtraction guidance, compared with those by live fluoroscopic guidance (McNemar test, P = 0.039). This is an important that live fluoroscopic guidance is useful method to detect intravascular injection but the vascular contrast patterns are overlapped by expected epidural patterns, it can miss more vascular injections. It comes as no surprise that the significant difference in detection of vascular injections between in live fluoroscopic images and in digital subtraction images.
Digital picture can be enhanced with a variety of controls such as contrast and brightness. Digital subtraction was achieved by imaging software of a computer [25]. Our fluoroscopic device has optional digital subtraction packages that would likely perform these steps automatically and faster. Subtraction of the preinjection image from the postinjection image eliminates the majority of bone shadows. This image can highlight the distribution of an epidurogram and vascular uptake clearly.
Disadvantage of the digital subtraction fluoroscopic imaging adds to radiation exposure to the patient, physician and staff. The cost of adding the digital subtraction to a new purchase or to upgrade an existing fluoroscopy is not high, but will not likely be compensated. The cost of an entry digital subtraction package would be about 15 thousand to 18 thousand dollars above the base cost of a good fluoroscopy.
It has been previously proposed that digital subtraction fluoroscopy may be useful method for documentation of epidural contrast spread and perhaps discography [18]. When contrast patterns are different from expected, the possibility that one is injecting into unintended structures should warn the injectionist to reposition the needle.
This finding demonstrate that digital subtraction fluoroscopic imaging is superior to blood aspiration or live fluoroscopy in detecting intravascular injections with lumbar transforaminal epidural injection. But, large-scale and controlled trials would be required to prove the effectiveness of digital subtraction fluoroscopic imaging in spinal diagnostic and treatment procedure.
Vascular contrast patterns are especially difficult to observe when they simultaneously occur to the expected epidural pattern. This is an important observation since this current study showed that live fluoroscopic guidance can miss more vascular injections when they simultaneously occur to the expected epidural injection (sensitivity 60%). This prospective evaluation demonstrate that digital subtraction fluoroscopic imaging is superior to blood aspiration or live fluoroscopy in detecting intravascular injections with lumbar transforaminal epidural injection.
References
1. Boswell MV, Trescot AM, Datta S, Schultz DM, Hansen HC, Abdi S, et al. Interventional techniques: evidence based practice guidelines in the management of chronic spinal pain. Pain Physician. 2007; 10:7–111. PMID: 17256025.
2. Buenaventura RM, Datta S, Abdi S, Smith HS. Systematic review of therapeutic lumbar transforaminal epidural steroid injections. Pain Physician. 2009; 12:233–251. PMID: 19165306.
3. Marshall LL, Trethewie ER, Curtain CC. Chemical radiculitis: a clinical, physiological and immunological study. Clin Orthop Relat Res. 1977; 129:61–67. PMID: 608297.
4. Wheeler AH, Murrey DB. Chronic lumbar spine and radicular pain: pathophysiology and treatment. Curr Pain Headache Rep. 2002; 6:97–105. PMID: 11872180.

5. Hadjipavlou AG, Tzermiadianos MN, Bogduk N, Zindrick MR. The pathophysiology of disc degeneration: a critical review. J Bone Joint Surg Br. 2008; 90:1261–1270. PMID: 18827232.
6. Yamashita M, Ohtori S, Koshi T, Inoue G, Yamauchi K, Suzuki M, et al. Tumor necrosis factor-alpha in the nucleus pulposus mediates radicular pain, but not increase of inflammatory peptide, associated with nerve damage in mice. Spine. 2008; 33:1836–1842. PMID: 18670336.

7. Botwin KP, Gruber RD, Bouchlas CG, Torres-Ramos FM, Freeman TL, Slaten WK. Complications of fluoroscopically guided transforaminal lumbar epidural injections. Arch Phys Med Rehabil. 2000; 81:1045–1050. PMID: 10943753.

8. Kennedy DJ, Dreyfuss P, Aprill CN, Bogduk N. Paraplegia following image-guided transforaminal lumbar spine epidural steroid injection: two case reports. Pain Med. 2009; 10:1389–1394. PMID: 19863744.

9. Bogduk N, Dreyfuss P, Baker R, Yin W, Landers M, Hammer M, et al. Complications of spinal diagnostic and treatment procedures. Pain Med. 2008; 9:S11–S34.

10. Houten JK, Errico TJ. Paraplegia after lumbosacral nerve root block: report of three cases. Spine J. 2002; 2:70–75. PMID: 14588291.
11. McLain RF, Fry M, Hecht ST. Transient paralysis associated with epidural steroid injection. J Spinal Disord. 1997; 10:441–444. PMID: 9355063.

12. Reitman CA, Watters W 3rd. Subdural hematoma after cervical epidural steroid injection. Spine. 2002; 27:E174–E176. PMID: 11884923.

13. Baker R, Dreyfuss P, Mercer S, Bogduk N. Cervical transforaminal injection of corticosteroids into a radicular artery: a possible mechanism for spinal cord injury. Pain. 2003; 103:211–215. PMID: 12749976.

14. Smuck M, Fuller BJ, Chiodo A, Benny B, Singaracharlu B, Tong H, et al. Accuracy of intermittent fluoroscopy to detect intravascular injection during transforaminal epidural injections. Spine. 2008; 33:E205–E210. PMID: 18379390.

15. Furman MB, Giovanniello MT, O'Brien EM. Incidence of intravascular penetration in transforaminal cervical epidural steroid injections. Spine. 2003; 28:21–25. PMID: 12544950.

16. Smuck M, Fuller BJ, Yoder B, Huerta J. Incidence of simultaneous epidural and vascular injection during lumbosacral transforaminal epidural injections. Spine J. 2007; 7:79–82. PMID: 17197337.

17. Jasper JF. Is digital subtraction fluoroscopy a useful tool for the interventional pain physician? Pain Physician. 2002; 5:36–39. PMID: 16896356.
18. Jasper JF. Role of digital subtraction fluoroscopic imaging in detecting intravascular injections. Pain Physician. 2003; 6:369–372. PMID: 16880884.
19. Batson OV. The vertebral vein system. Caldwell lecture, 1956. Am J Roentgenol Radium Ther Nucl Med. 1957; 78:195–212.
20. Tiso RL, Cutler T, Catania JA, Whalen K. Adverse central nervous system sequelae after selective transforaminal block: the role of corticosteroids. Spine J. 2004; 4:468–474. PMID: 15246308.

21. Breslin DS, Martin G, Macleod DB, D'ercole F, Grant SA. Central nervous system toxicity following the administration of levobupivacaine for lumbar plexus block: a report of two cases. Reg Anesth Pain Med. 2003; 28:144–147. PMID: 12677626.

22. Kim DW, Shim JC. Incidence of intravascular penetration during transforaminal lumbosacral epidural steroid injection. Korean J Pain. 2007; 20:26–30.

23. Karasek M, Bogduk N. Temporary neurologic deficit after cervical transforaminal injection of local anesthetic. Pain Med. 2004; 5:202–205. PMID: 15209975.

24. Stretanski MF, Chopko B. Unintentional vascular uptake in fluoroscopically guided, contrast confirmed spinal injections: a 1-yr clinical experience and discussion of findings. Am J Phys Med Rehabil. 2005; 84:30–35. PMID: 15632486.

25. Barbey MM, Farber A, Marienhoff N, Gmelin E. Digital subtraction angiography with carbon dioxide-basic principles, technique and clinical application. Vasa. 1999; 28:243–249. PMID: 10611841.
Fig. 1
(A) An anteroposterior live fluoroscopic image taken during contrast injection for right L5-S1 transforaminal steroid injection. It shows the epidural contrast pattern without vascular injection. (B) An anteroposterior digital subtraction image taken during same injection. It shows a simultaneous epidural and vascular contrast pattern.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download