Mutations in the BCR/ABL kinase domain contribute to resistance to imatinib, which has driven the choice of second-line tyrosine kinase inhibitors, such as dasatinib or nilotinib, in CML patients. Thus far, more than 90 different mutations have been reported in previous reports [1, 2]. The majority of known mutations are missense mutations. In contrast, insertion or deletion mutations are very rare, and only 3 such mutations have been reported [3, 4]. Here, we describe the insertions of 35 nucleotides resulting from frameshift mutation (p.Cys475Tyrfs*11) in the BCR/ABL kinase domain, which contributed to imatinib resistance, in 2 Korean patients with CML.
Case 1 was a 20-yr-old woman who was diagnosed with CML in the chronic phase 2 yr before. She had a major BCR/ABL rearrangement (b3a2) at diagnosis with a BCR/ABL fusion transcript/GAPDH ratio of 0.024 in peripheral blood (PB). She was treated with imatinib. The response was successful during the follow-up period, and the ratio was maintained between 0.0002 and 0.0003 in PB. After 15 months of imatinib treatment, her BCR/ABL quantification ratio increased to 0.05 in PB, which suggested molecular relapse. The therapeutic regimen was changed to dasatinib immediately, and her follow-up BCR/ABL quantification results 3 weeks after the change of treatment regimen showed marked reduction (from 0.05 to 0.00014) in PB. She was in a complete hematologic response state at a follow-up bone marrow examination that was performed 4 months after the treatment change from imatinib to dasatinib.
Case 2 was a 38-yr-old man who was treated with imatinib for 5 yr but who suffered from relapse with a lymphoblastic crisis of CML 4 yr before. After the relapse, he immediately underwent allogeneic bone marrow transplantation (BMT), and his BCR/ABL quantification results in PB changed from 0.25 at relapse to negative after the BMT. Five months after the BMT, his follow-up BCR/ABL quantification results in PB increased to 0.52, which suggested molecular relapse, but the treatment regimen was not changed. Finally, he expired due to sepsis 1 month after molecular relapse.
To confirm the diagnosis of imatinib resistance, BCR/ABL kinase domain mutation analyses that were based on reverse transcriptase PCR-direct sequencing were performed retrospectively using stored RNA at the time of molecular relapse for both patients. cDNA was synthesized from stored RNA by reverse transcriptase PCR methods. Three sets of forward and reverse primers were used for amplification of the BCR/ABL kinase domain, and the sequences of each primer were as follows: ABL-A (forward: 5'-CAT CAT TCA ACG GTG GCC GAC GG-3', reverse: 5'-GTT GCA CTC CCT CAG GTA GTC-3'), ABL-B (forward: 5'-GAA GAA ATA CAG CCT GAC GGT G-3', reverse: 5'-CGT CGG ACT TGA TGG AGA A-3'), and ABL-C (forward: 5'-TGA CAG GGG ACA CCT ACA CA-3', reverse: 5'-ATC TCA GGC ACG TCA GTG GT-3'). The amplification protocol consisted of an initial denaturation at 95℃ for 5 min, which was followed by 32 cycles of denaturation at 95℃ for 30 sec, annealing at 60℃ for 30 sec, and extension at 68℃ for 3 min, and a final extension at 72℃ for 7 min. After confirmation of the single bands that were sized 393, 482, and 487 bp by electrophoresis for ABL-A, -B, and -C, respectively, direct sequencing was performed using the BigDye Terminator Cycle Sequencing Ready Reaction kit on the ABI 3130 genetic analyzer (Applied Biosystems, Foster City, CA, USA) according to the manufacturer's protocol. The Sequencher program (GeneCodes Corp., Ann Arbor, MI, USA) was used for alignment with the reference sequence (Genbank accession no. X16416.1). The identified mutation was described according to the Human Gene Variation Society guidelines (http://www.hgvs.org/).
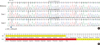
The direct sequencing results for both patients showed the same heterozygous frameshift mutation, which was an insertion of 35 nucleotides between the 1,423rd and 1,424th nucleotide (c.1423_1424ins35), substituting cysteine with tyrosine at the 475th codon and introducing a premature termination codon at the 11th downstream codon (p.Cys475Tyrfs*11) (Fig. 1). According to a review of the mutation database and a previous study, this was 1 of the 3 rare insertion or deletion mutations that have so far been reported only once [3, 4].
As previously reported, the majority of BCR/ABL kinase domain mutations resulting in imatinib resistance are missense mutations, comprising more than 95% of the known mutations. Otherwise, insertion or deletion mutations resulting in the premature truncation of the BCR/ABL kinase domain are very rare [1-4]. Given that different mutations have been shown to confer variable degrees of imatinib resistance, we can hypothesize that a frameshift mutation, which is the same type of mutation found in our patients, may induce more severe imatinib resistance than missense mutations because a truncated protein is thought to be generally more dysfunctional than a conserved protein that has only a single residue change. Our results supported this hypothesis because case 2 showed a very poor prognosis without a treatment regimen change, while case 1, whose therapeutic drug was changed from imatinib to dasatinib immediately after molecular relapse, showed good prognosis with no evidence of relapse. Therefore, it can be speculated that, in patients with insertion or deletion mutations resulting in premature truncation of the BCR/ABL kinase domain, a prompt change of treatment regimen is essential for the management of these patients.
In conclusion, we describe a rare frameshift mutation of Cys475Tyrfs*11 in the BCR/ABL kinase domain that contributed to imatinib resistance in 2 Korean patients with CML, and a prompt change of treatment regimen from imatinib to dasatinib was critical in these patients.
Figures and Tables
Fig. 1
Direct sequencing results of the BCR/ABL kinase domain in the 2 patients with CML are shown in the order of wild type (upper), case 1 (middle), and case 2 (bottom) (A). Both of our patients showed a heterozygous insertion of 35 bp (ACTTTGATAACCGTGAAGAAAGAACAAGATAGAAG) between the 1,423rd and 1,424th nucleotides (c.1423_1424insACTTTGATAACCGTGAAGAAAGAACAAGA TAGAAG), which resulted in the substitution of the cysteine with tyrosine at the 475th codon and introduced a premature termination codon at the 11th downstream codon (p.Cys475Tyrfs*11). The results are summarized in the following table (B).
References
1. Soverini S, Hochhaus A, Nicolini FE, Gruber F, Lange T, Saglio G, et al. BCR-ABL kinase domain mutation analysis in chronic myeloid leukemia patients treated with tyrosine kinase inhibitors: recommendations from an expert panel on behalf of European LeukemiaNet. Blood. 2011. 118:1208–1215.
2. Soverini S, Martinelli G, Amabile M, Poerio A, Bianchini M, Rosti G, et al. Denaturing-HPLC-based assay for detection of ABL mutations in chronic myeloid leukemia patients resistant to Imatinib. Clin Chem. 2004. 50:1205–1213.
3. Bamford S, Dawson E, Forbes S, Clements J, Pettett R, Dogan A, editors. Catalogue of Somatic Mutations in Cancer. last updated on 12 Mar 2012. http://www.sanger.ac.uk/genetics/CGP/cosmic.
4. Strhakova L, Bujalkova MG, Hojsikova I, Lukackova R, Behulova R, Mistrik M, et al. Use of direct sequencing for detection of mutations in the BCR-ABL kinase domain in Slovak patients with chronic myeloid leukemia. Neoplasma. 2011. 58:548–553.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download