This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
We aimed to determine the long-term motor and sensory outcomes of patients with infantile exotropia.
Methods
In this longitudinal retrospective (historical cohort) study, the records of 76 patients with infantile exotropia were Studied. Subjects with constant exotropia manifesting before the age of 1 year who were at least 5 years old at recruitment time between 2008 and 2017 were included.
Results
The medical records of 26 patients were excluded due to not participating in follow-up examinations or having incomplete records. In total, 54 infantile exotropic patients (51.9% male) with a mean age of 11.1 ± 6.8 years and follow-up of 4.99 ± 3.58 years were studied. Postoperative sensory outcomes (central stereopsis [<60 sec/arc], peripheral fusion [60–3,000 sec/arc], and non-stereopsis [>3,000 sec/arc]) were observed in 38.9%, 38.9%, and 21.2% of patients, respectively. In terms of postoperative motor outcomes, 69%, 24%, and 7% were achieved as orthophoria, residual exotropia, and consecutive esotropia, respectively. Patients with a higher surgical age (p = 0.022) and better visual acuity (p = 0.004) had significantly better sensory outcomes, while higher preoperative deviation resulted in more suppression (p = 0.039, rs = 0.218).
Conclusions
With rates of 69% for motor success and 78.8% for sensory success, surgical outcomes of infantile exotropic patients seems to be favorable. Further studies are recommended to verify our findings.
Keywords: Infantile exotropia, Motor, Sensory, Surgical outcome
Infantile exotropia is defined by idiopathic, large-angle, constant exotropia appearing in the first 6 to 12 months of life [
12]. Based on the literature, infantile exotropia has an incidence rate of 1.1% [
3] and it is reported to affect about one per 30,000 infants in the general population [
4]. Early surgery is essential to achieve optimal motor and sensory outcomes [
25]. Surgery within 2 years of birth has been reported to yield an 80% success rate, while the success rate decreases to 40% thereafter [
6]. Similarly, acceptable sensory results are expected in 30% to 75% of patients if they are operated before the age of 2 years due to improvements in their ocular alignment and the development of binocular fusion [
7].
In a study by Hiles and Biglan [
8], 93% of infantile exotropic patients with a history of operation before 2 years of age showed fusion on the Worth four-dot test, and 75% responded to the Titmus stereo test in near distance; meanwhile in some other studies, sensory outcomes were disappointing [
39]. Elsewhere, Choi and Kim [
10] found that only 25% of their infantile exotropic patients who underwent surgery before the age of 1 year achieved good sensory outcomes after 12 months of follow-up.
To our knowledge, few studies have evaluated the long-term sensory outcomes of patients with infantile exotropia. As such, we aimed to elucidate these outcomes among children with different surgical ages.
Materials and Methods
In this longitudinal retrospective study, we included the records of all infantile exotropic patients (n = 76) who were operated either at Torfeh or Imam Hossein Medical Centers affiliated to the Shahid Beheshti University of Medical Sciences from 2008 to 2017. This study was approved by the Ethics Committee of the Ophthalmic Research Center, Shahid Beheshti University of Medical Sciences (IR.SBMU.ORC.REC.1397.15) and our study protocol adhered to the 1964 Declaration of Helsinki. A written informed consent letter was obtained from all study subjects after explanation of the study details.
We confirmed exotropia onset by (1) observing childhood photos taken before the age of 1 year, (2) reviewing the dates of operational records, or (3) by asking the patient's parents about the age of appearing eye deviation. The records of patients with exotropia onset occurring before age of 1 year with a constant angle of exotropia (≥30 prism diopters [PD]) and history of strabismus operation(s) by unilateral or bilateral lateral rectus recession with or without accompanying operations and an age of 5 years at time of recruitment were selected. Premature patients with a gestational age of 34 weeks a nd a birth weight of less than 1,500 g [
11] and patients who had a history of trauma, neurological (e.g., developmental disorders, cerebral palsy) and/or systemic diseases, orbital pathology, consecutive exotropia due to the previous esotropia surgery and fixational disorders (e.g., nystagmus, wandering eye, eccentric fixation) were excluded.
Eventually, we recruited 54 eligible patients who were at least 5 years old and their parents signed a consent form for inclusion following explanation of the study procedure. Variables included age of strabismus onset and surgery, spherical equivalent, type of operation, preoperative and postoperative angle of deviation, and accompanying operation data were gathered from their ocular examination records.
Recruited patients' examinations included visual acuity assessment by the Yang Vision Tester (SIFI Diagnostic SPA, Sicily, Italy) at a distance of 6 m under daylight conditions. Amblyopia was considered if the best-corrected visual acuity (BCVA) was 0.3 logarithm angle of resolution (logMAR) or worse or the BCVA difference between the two eyes was at least two lines [
12]. Young infantile exotropic patients were examined by cycloretinoscopy and we recorded spherical equivalents for them based on their ocular examination results, while the recruited patients who were at least 5 years old were examined using cycloautorefractometry (RM-8800; Topcon Medical, Oakland, NJ, USA). However, if any of these patients were not cooperative, we performed cycloretinoscopy instead. Measurements were repeated 30 to 45 minutes after the installation of tropicamide 1% and cyclopentolate 1% eye drops. The angle of deviation was measured at far (6 m) and near (30 cm) distances using the alternative prism cover or Krimsky test. Ocular motility was evaluated in all nine cardinal visual gazes. The A–V pattern was checked at 30 degrees superiorly and inferiorly to the primary position. Postoperative motor results were considered to indicate orthotropia if the deviation was between exotropia <10 PD to esotropia <5 PD, while residual exotropia was defined as the postoperative exotropia ≥10 PD a nd consecutive esotropia confirmed if the postoperative esotropia was ≥5 PD. Stereoacuity was determined using the Titmus test at near and classified as either central or fine stereopsis (<60 sec/arc), peripheral or gross stereopsis (60–3,000 sec/arc), or nonstereopsis (>3,000 sec/arc) [
13]. The Worth four-dot test results were classified as binocular fusion (four lights with orthotropia), suppression (two red or three green lights with deviation ≥10 PD), or abnormal retinal correspondence (four lights with deviation ≥10 PD). Clinically, combined sensory and motor outcomes were classified as excellent (orthophoria with fine stereopsis), fair (orthophoria with gross stereopsis), or failure (deviation with no stereopsis). Anterior and posterior ocular segments were examined using biomicroscopy and indirect ophthalmoscopy through the dilated pupil.
Sample size calculation
The sample size of the present study was calculated based on unpublished data indicating the findings of postoperative gross stereopsis in 6.7% of patients, which subsequently increased to a rate of 33.3% 1 year after the surgery. A sample size of 52 patients was calculated as necessary with consideration of a type I error of 0.05 and study power of 95%.
Statistical analysis
To describe data, we used means and standard deviations. To compare the results between groups, we employed Fisher's exact test (in nominal variables) and the Mann-Whitney test (in ordinal variables). To assess the relation of the baseline far deviation and the final result of the surgery (represented as an ordinal variable), we used Spearman's correlation coefficient (rs). All statistical analyses were performed using the IBM SPSS Statistics ver. 25.0 (IBM Corp., Armonk, NY, USA). All tests were two-tailed and p-values less than 0.05 were considered to be statistically significant.
Results
In this study, a total of 54 infantile exotropic patients (51.9% male) with a recruitment mean age of 11.1 ± 6.8 years were included.
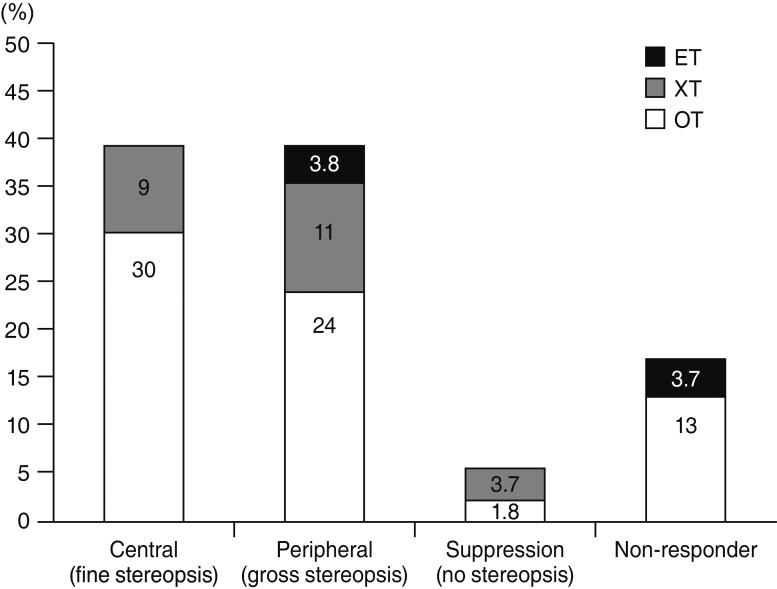
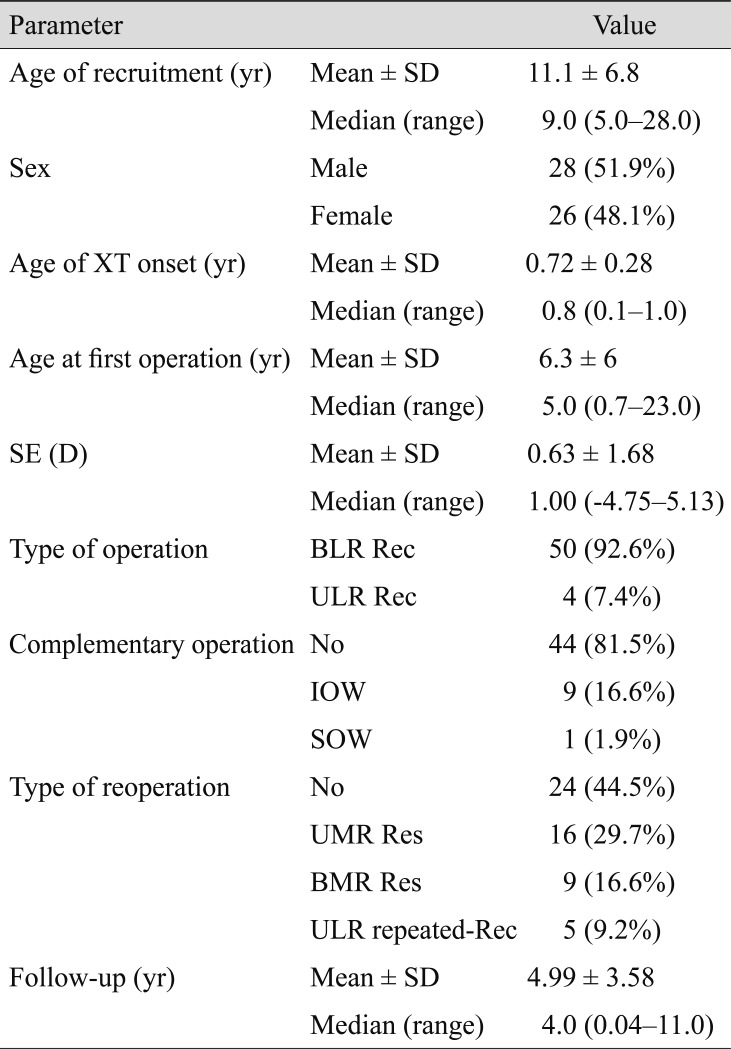
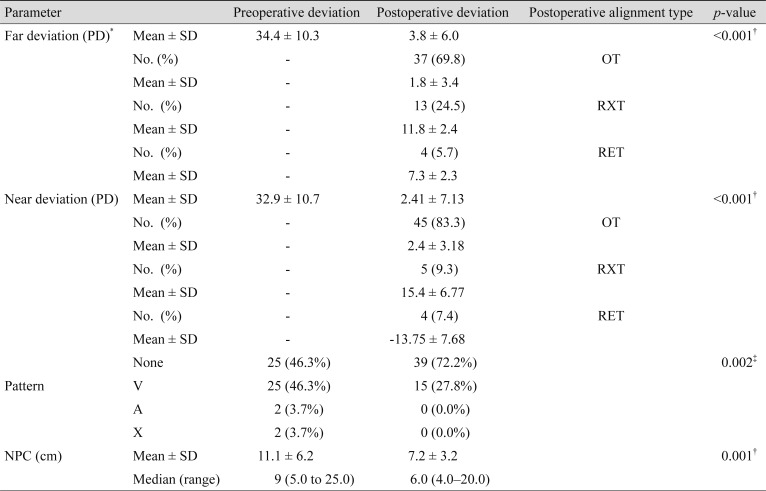
Table 1 summarizes the baseline characteristics of our study participants. As shown, most of the cases were operated on using the bilateral lateral rectus recession (92.6%) method and about 30% of their reoperations were unilateral medial rectus resection. Study subjects were followed up with for a n average of 4.99 ± 3.58 years. The postoperative mean angle of deviation was reduced significantly at distance and near (
p < 0.001) (
Table 2 and
Fig. 1). The postoperative ocular pattern was also significantly improved in patients with infantile exotropia (
p = 0.002).
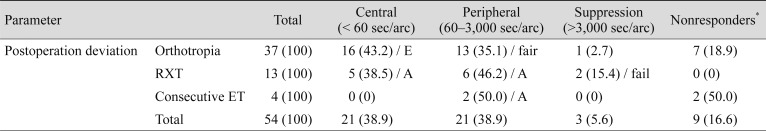
The results of Titmus testing are presented in
Table 3. The postoperative Worth four-dot test revealed 41 patients (75.9%) had binocular fusion and three patients (5.6%) had suppression, while 10 patients (18.5%) were uncooperative during this test so no results could be obtained.
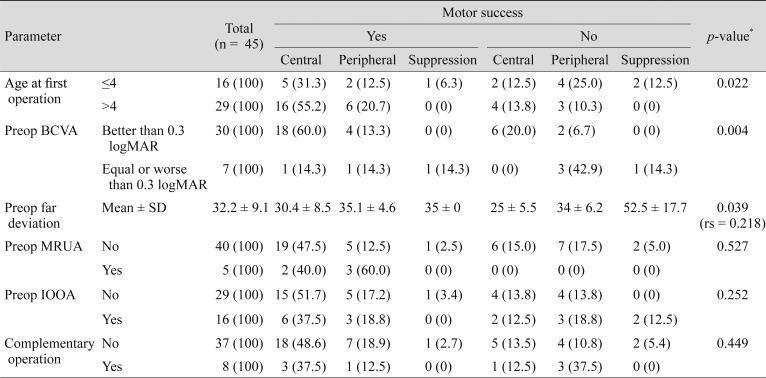
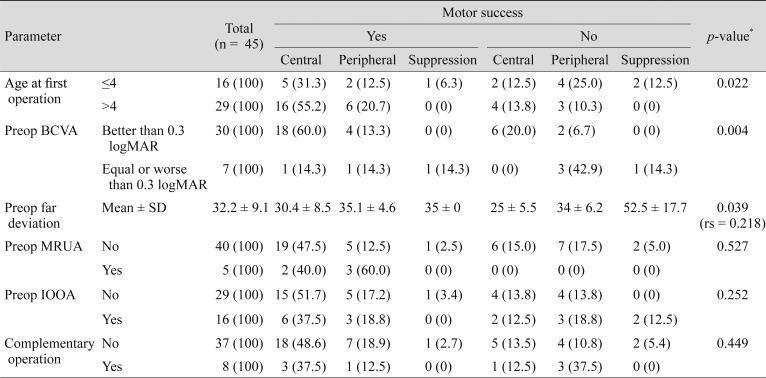
The postoperative sensory and motor outcomes with regard to different factors are presented in
Table 4. As shown, patients with a surgical age of older than 4 years (
p = 0.022) and who had preoperative BCVA results of better than 0.30 logMAR (
p = 0.004) had significantly better sensory outcomes, while a higher preoperative angle of deviation resulted in more suppression (
p = 0.039, rs = 0.218). None of the other factors (e.g., age of the first operation, preoperative inferior oblique over-action and complementary operation) were found to be risk factors affecting surgical outcomes of infantile exotropia.
Discussion
Infantile exotropia is defined as a large and constant outward eye deviation with an onset age of up to 12 months [
12]. As reported by different studies, even with early surgery, bifoveal fixation is less likely to be obtained in these cases [
39].
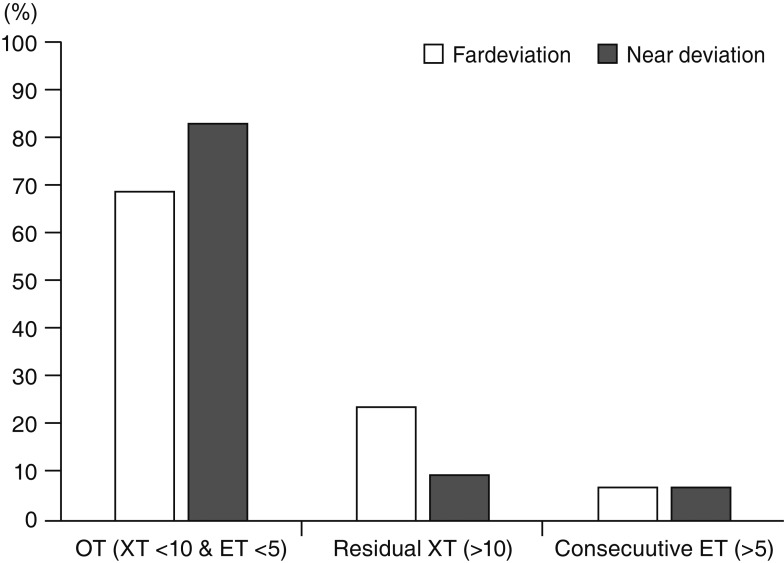
In the present study, postoperative fusion response findings as measured by the Titmus stereo test at near were obtained in 78% of our subjects, while postoperative motor success rates of 69% and 83.5% were achieved at far and near, respectively (
Fig. 1). This means that 9% of our subjects responded to the Titmus test at near despite showing residual exotropia at far. These results may suggest the convergence ability of these patients via positive fusional vergence at near.
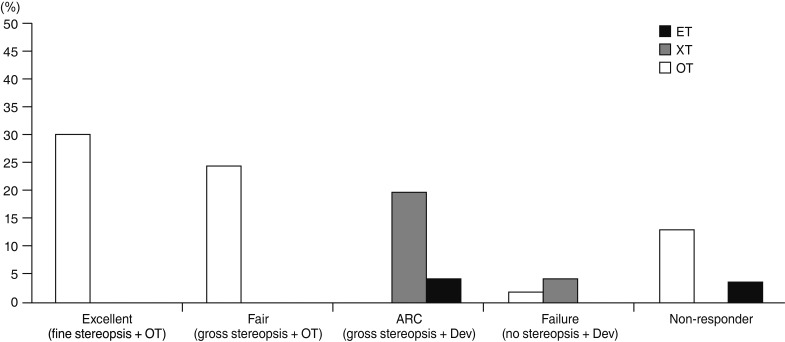
On the other hand, 1.8% of our subjects were not able to respond to the Titmus stereo test (suppression) in spite of having orthophoria (
Fig. 2). This outcome could be related to surgery being conducted in older ages after the brain maturation period. Fortunately, this occurred only in a very small portion of patients.
Best sensory outcomes were obtained in 21 subjects (39%) with fine stereoacuity, which is considered a very positive result (
Table 3 and
Fig. 2). This success may be due to these patients obtaining some degree of fusion when they were intermittent exotropia prior to the constancy of their deviation in the first two months of their life or we may have unintentionally included some patients with early-onset intermittent exotropia. Furthermore, it was found that surgery in patients aged older than four years and who had better baseline vision (BCVA better than 0.3 logMAR) led to better sensory outcomes observe after the surgery. The reason for this may be linked with the possibility of better measurements of deviation and an increased ability to respond to the Titmus test in older patients. More disappointing surgical outcomes and suppression were observed in cases with larger preoperative angle of deviation (
Table 4 and
Fig. 3).
A high level of binocularity has been reported in some studies where patients were followed up at least for four years [
1415]. This could be due to the intermittent nature of exodeviation before its constancy. In addition, early-onset intermittent exotropia may be associated with infantile exotropia in one-third to one-half of cases, leading to the observed high level of binocularity.
Hunter et al. [
3] reported the 1-year follow-up sensory results of 13 infantile exotropic patients with the same distribution of 50% between the intermittent and constant exotropic patients. Postoperative binocular vision was achieved in 70% of cases, while none of the included patients achieved bifixation. The authors did not find any statistically significant difference between the two groups regarding either sensory or motor outcomes, although the baseline angle of the intermittent group were significantly less when compared with the constant exotropia group. Overall, their fusion results were in line with our sensory outcomes (77%) except in terms of bifixation achievement, which was seen in 39% of our subjects.
Saunders and Trivedi [
16] studied 12 patients with early-onset intermittent exotropia and strabismus onset occurring before the age of 1 year and the surgical age of up to 2 years. These authors reported a stereoacuity of 40, 100, and 100 to 400 seconds of arc in two, three, and two patients, respectively (58%). They also found motor success corresponded to their sensory outcomes. As such, they concluded that the surgical outcomes in cases with early-onset intermittent exotropia were highly satisfying and that high grades of binocularity might be achievable in some cases.
Generally, combined motor and sensory success were obtained in 54% of our subjects, which is in line with the success rate of 58% reported by Saunders and Trivedi [
16]. We found different grades of fusion in 20% of our residual exotropic patients and 4% of our consecutive esotropic patients, respectively, outcomes resulting from the reduction of their exotropia to a similar degree of or less than the amount of esotropia at far (>5 and <10 PD).
In addition, 3.7% of our patients experienced failure response that could be due to the residual exotropia or their previous suppression. Only one patient (1.8%) had suppression while he was orthophoric, possibly due to the late timing of his surgery.
In our study, 76% of our cases showed f usion on the Worth four-dot test similar in scope to the Titmus test findings at near. Suppression and/or abnormal retinal correspondence were observed in 14% of our subjects, while 10% did not respond to the Worth four-dot test at all.
In our study, motor success rates of 69% and 83% at far and near distances and an A–V pattern among 27.8% of the population were obtained. In the study by Hunter et al. [
3], the motor success rate of 82% (±10 PD) and an A–V pattern affecting 38% were noted. As stated before, the criteria of exotropia <10 PD and esotropia <5 PD were considered as definitions of postoperative success in our study. The success rate of our investigation would likely be in line with the results of the study by Hunter et al. [
3] if we had considered the criteria of ±10 PD for our motor success postoperatively.
In this study, the onset of infantile exotropia was identified by way of reviewing the child's photos at the age of less than 1 year and/or health records or parents' reports. It should be noted that the differentiation of cases with early-onset intermittent exotropia from infantile exotropia before their administration time was not absolutely possible—especially when all of them had constant exotropia (more than 15 PD) at the time of administration.
Based on our findings, both our sensory and motor surgical outcomes of infantile exotropic patients were satisfactory, although these results could be due to the early intermittent phase of deviation before their constant exotropia at the time of administration. Further studies with a prospective design are recommended to investigate the postoperative sensory outcomes in infantile exotropic patients with an onset before the age of 1 year and surgery up to the age of 2 years.
Fig. 1
Postoperative motor outcomes in both far and near distances among patients with infantile exotropia (XT). OT = orthotropia; ET = esotropia.
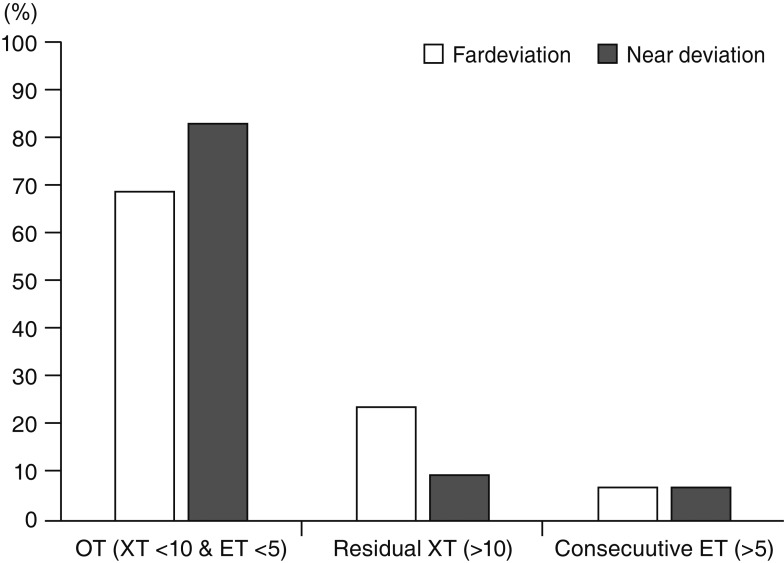
Fig. 2
Postoperative sensory outcomes in patients with infantile exotropia (XT). ET = esotropia; OT = orthotropia.
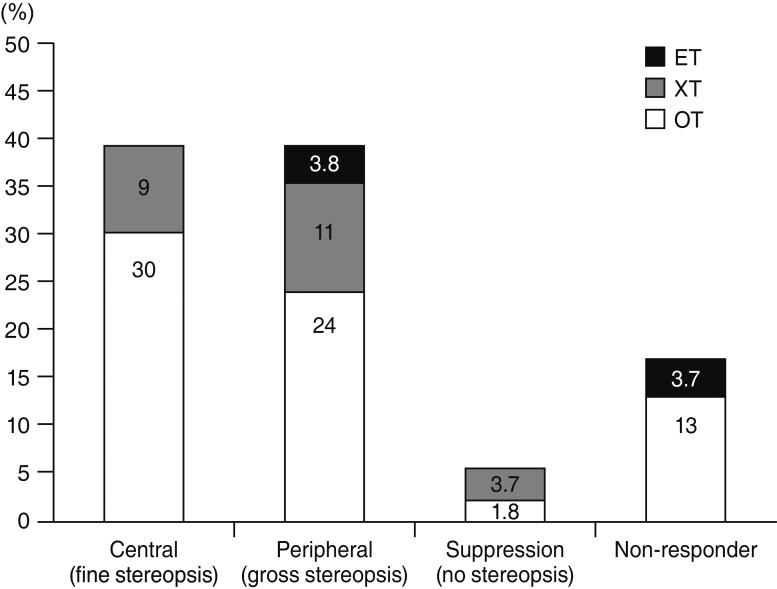
Fig. 3
Postoperative combined motor and sensory outcomes in patients with infantile exotropia (XT). ET = esotropia; OT = orthotropia; ARC = abnormal retinal correspondence; Dev = deviation.
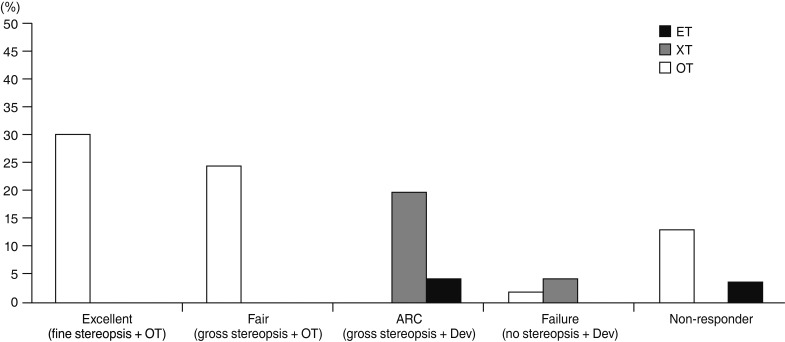
Table 1
Baseline characteristics of the study participants
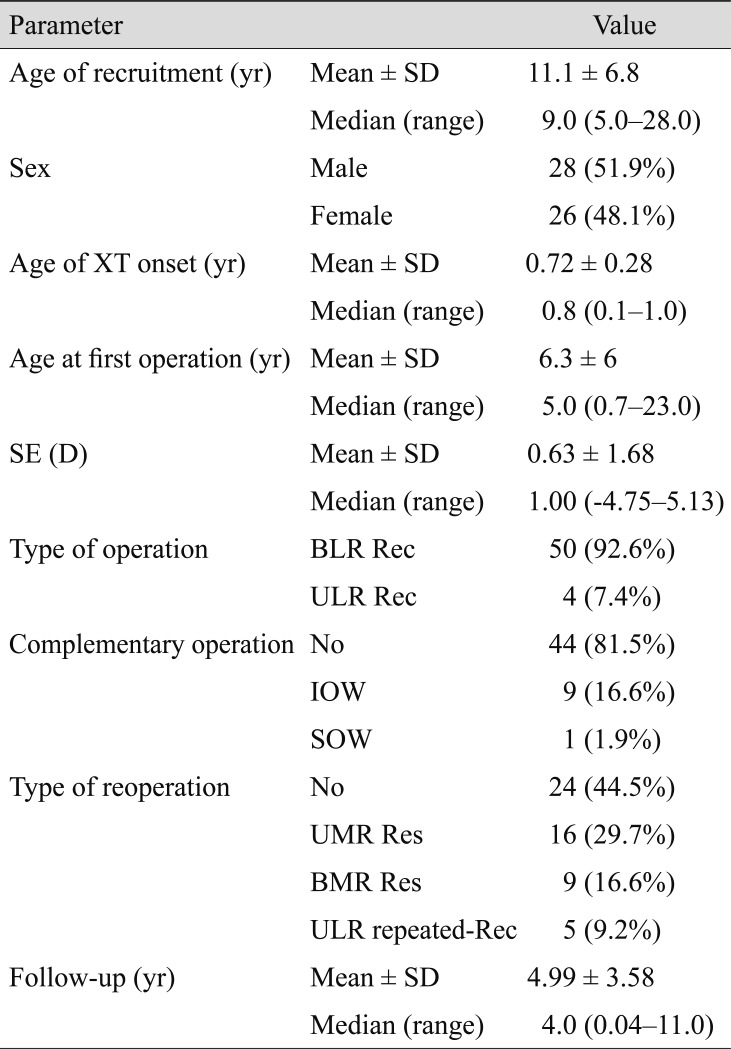
Table 2
Preoperative and postoperative extraocular muscle function and alignment
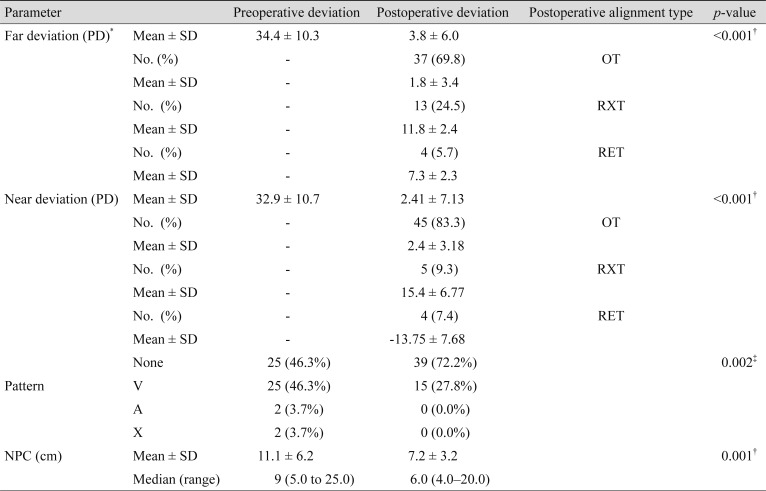
Table 3
Postoperative results of the near Titmus test of our subjects regarding to their alignment
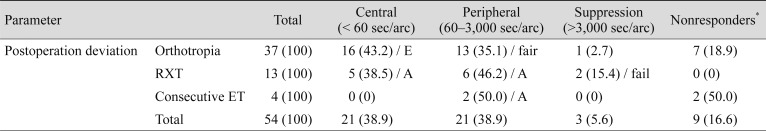
Table 4
Postoperative sensory and motor outcomes related to different factors




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download