Abstract
Purpose
To compare the anterior capsule contraction and intraocular lens (IOL) decentration among three types of IOL to determine the influence of haptic design on anterior capsule stability.
Methods
One hundred fifty patients were enrolled in this prospective, randomized study and 260 eyes underwent implantation of one of the following IOLs: modified L-haptic IOL (n = 74), modified C-haptic IOL (n = 97), or a plate-haptic IOL (n = 89). The area of the anterior capsule opening, IOL decentration, and capsule overlap were measured using retroillumination photospot 1 day and 2 months after cataract surgery.
Results
The area of capsule opening at postoperative day 1 was significantly different between the three IOLs (p < 0.01). All IOLs showed reduction of the anterior capsule opening from 1 day to 2 months after surgery, and greater reduction was shown in the modified C-haptic IOL (p < 0.001). At postoperative month 2, IOL decentration was significantly different between the IOLs and showed a positive correlation with the mean area reduction during month 2.
Complete anterior capsulotomy is one of the critical steps in cataract surgery. Even in cases where the surgeon performs a perfect capsulotomy, changes in the anterior capsule opening may occur, usually several weeks after surgery [1]. Reduction of the anterior capsule opening area leads to a reduced optic zone area and severe contraction may cause a reduction in visual outcomes. Recently, several studies have focused on how to prevent anterior capsule contraction.
Some pathologic conditions, like uveitis, pseudoexfoliation syndrome, and retinitis pigmentosa, are correlated with anterior capsule contraction [234]. In normal eyes, reduction of the anterior capsule opening is related to the initial anterior capsulotomy size, roundness, circularity, and intraocular lens (IOL) design and material [567]. Some studies have reported that silicone IOLs with a plate-haptic design are more susceptible to anterior capsule shrinkage due to the limitation of capsular dilation [8]. Tsinopoulos et al. [9] reported that anterior capsule contraction syndrome occurs more frequently with hydrophilic lenses than with hydrophobic lenses.
Due to advances in minimally invasive surgery, foldable acrylic IOLs are preferred over various other materials. We hypothesized that IOL haptic design may influence anterior capsule stability in the very early post-surgery period, even when IOLs are made of the same material. A previous study compared IOLs made with different designs and different materials. There are few studies that have evaluated differences in anterior capsule stability after single piece acrylic IOL implantation with modified L-haptic design or plate-haptic design.
The purpose of our study was to compare anterior capsule contraction and IOL decentration following implantation of single piece acrylic IOLs with different haptic designs.
This was a prospective, observer-blinded study of patients who had cataract surgery between March 2012 and November 2013 at Seoul St. Mary's Hospital, Seoul, Korea. In all, 260 eyes from 150 patients were included in this study. Study protocol followed the guidelines of the Declaration of Helsinki and was approved by the hospital's institutional review board. Written informed consent was obtained from patients before the study and potential complications were explained in detail. Inclusion criteria were the presence of a senile cataract in adults older than 55 years of age, normal axial length between 22 mm and 25.5 mm, and a dilated pupil larger than 8.0 mm. No patient had a history of ocular surgery, pupil abnormality, or ocular disease other than cataract. Each patient underwent a complete ophthalmologic evaluation.
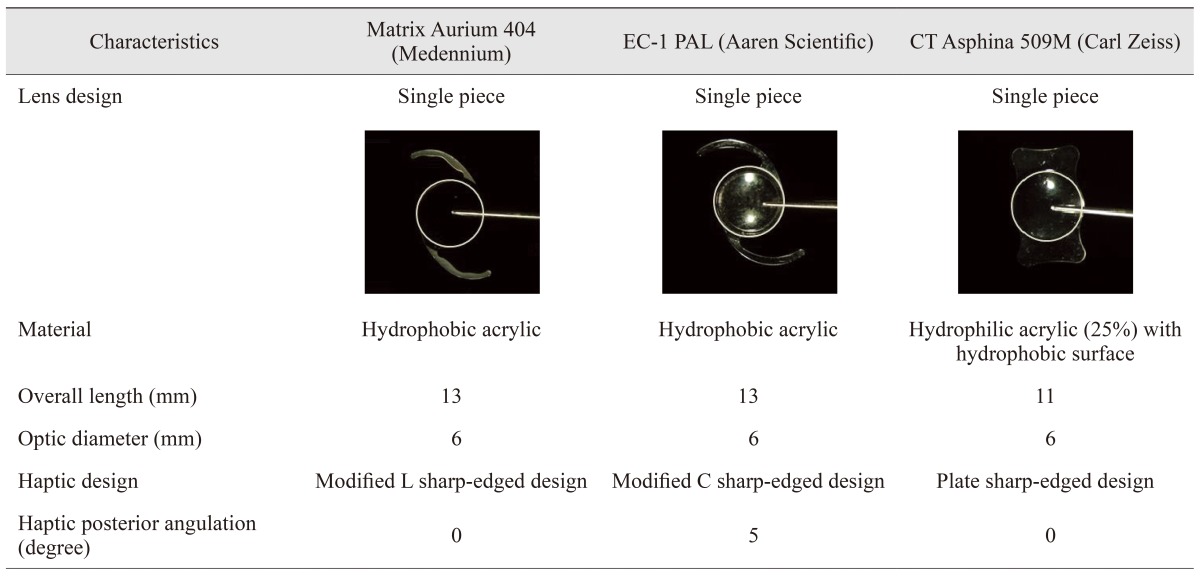
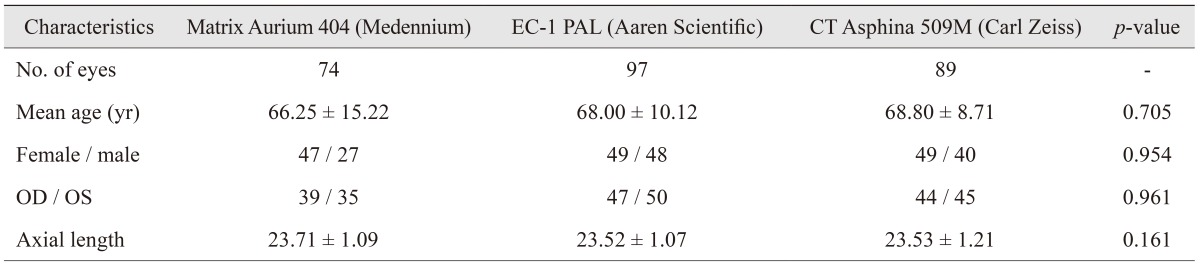
Patients were randomly implanted with one of three types of IOL during cataract surgery: Matrix Aurium 404 IOL (Medennium, Irvine, CA, USA), EC-1 PAL IOL (Aaren Scientific, Ontario, CA, USA), and CT Asphina 509M IOL (Carl Zeiss, Jena, Germany). The three IOLs have different haptic designs but are made of the same acrylic material and consist of a single piece (Table 1).
One surgeon (CKJ) performed all of the cataract surgeries using a standard procedure. Continuous curvilinear capsulorhexis of 5.0 mm to 5.5 mm diameter was carefully performed. After successful phacoemulsification, the IOL was implanted.
Digital retroillumination photospots through a dilated pupil were obtained to evaluate the area of the anterior capsule opening immediately after continuous curvilinear capsulorhexis before viscoelastic removal, 1 day and 2 months postoperatively (Fig. 1A-1C). IOL decentration was measured using vector analysis between the pupil center and IOL center. Maximal and minimal distances between the edge of capsulotomy and the edge of the IOL optic were calculated to determine capsulotomy overlap (overlap = distance minimum / distance maximum). All measurements were repeated three times and performed by a single experienced technician. Photospots were imported into Image J (National Institutes of Health, Bethesda, MD, USA) for measurement of capsulotomy diameter and area. IOL optic size was used as a reference scale. We used the same amount and type of mydriatic eyedrops to eliminate the effect of mydriatic drops on changes in the shape and size of the pupil before taking the photospot.
Statistical analysis was performed using PASW ver. 18.0 (SPSS Inc., Chicago, IL, USA). Paired t-tests and Mann-Whitney tests were used for pair-wise comparisons. One-way ANOVA was used to compare all three IOLs. Pearson correlations were used to evaluate linear relationships. All data are expressed as the mean ± standard deviation. A p-value less than 0.05 was considered statistically significant.
Seventy-four patients received a modified L-haptic IOL, 97 patients received a modified C-haptic IOL, and 89 patients received a plate-haptic IOL implant. The average patient age was 66.25 ± 15.22 years in the modified L-haptic IOL group, 68.00 ± 10.12 years in the modified C-haptic IOL group, and 68.80 ± 8.71 years in the plate-haptic IOL group (p = 0.705) (Table 2).
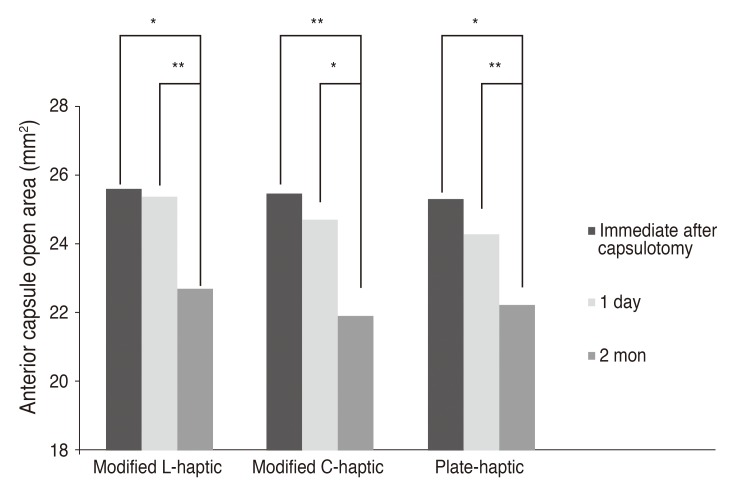
The initial area of the anterior capsule opening was not significantly different between the three IOL groups (p = 0.129). Fig. 2 shows the area of the anterior capsule opening on day 1 and 2 months postoperatively according to the IOLs. The differences in area between the time point after continuous curvilinear capsulorhexis and postoperative day 1 was 0.38 ± 1.26 mm2 for the modified L-haptic IOL, −0.54 ± 1.88 mm2 for the modified C-haptic IOL, and 0.03 ± 2.13 mm2 for the plate-haptic IOL.
All IOLs showed significant reductions in anterior capsule opening at 2 months compared to on day 1, and a greater reduction was shown in the modified C-haptic IOL (modified L-haptic IOL, −1.81 ± 2.76 mm2; modified C-haptic IOL, −3.91 ± 2.91 mm2; and plate-haptic IOL, −2.50 ± 1.95 mm2) groups. The mean area reduction was significantly different between the three IOLs (p = 0.003).
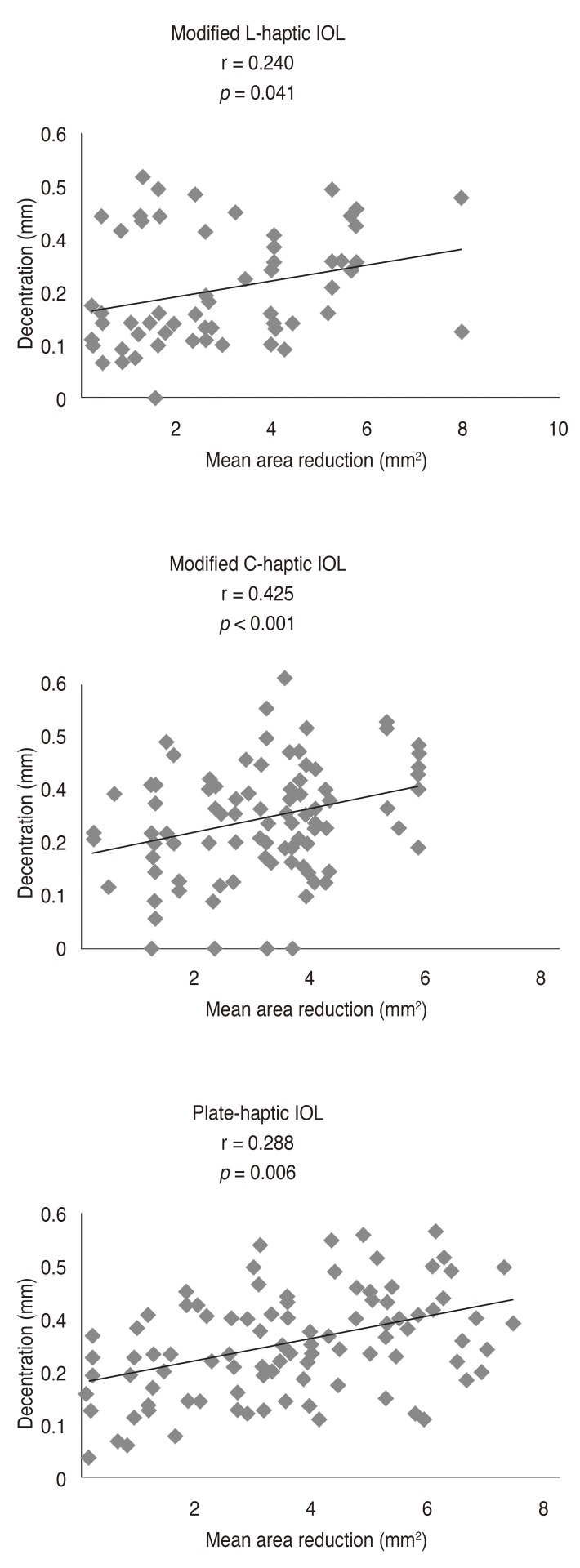
Two months postoperative, IOL decentration was significantly different between the three IOLs (modified L-haptic IOL, 0.24 ± 0.12; modified C-haptic IOL, 0.31 ± 0.12; and plate-haptic IOL, 0.26 ± 0.11, respectively; p = 0.002). No significant differences were founded in capsule overlap between the three IOLs (modified L-haptic IOL, 0.51 ± 0.16; modified C-haptic IOL, 0.48 ± 0.17; and plate-haptic IOL, 0.51 ± 0.16, respectively; p = 0.233). In all three IOLs, the degree of IOL decentration was significantly correlated with mean area reduction between the initial capsulotomy and postoperative month 2, with the strongest correlations observed for the modified C-haptic IOL (Fig. 3).
Various reports have shown that IOL design and material are correlated with anterior capsule contraction [810]. With respect to IOL material, contraction occurs more frequently with silicone IOLs than with polymethylmethacrylate or acrylic IOLs [8]. Hayashi et al. [10] reported that hydrophilic acrylic IOLs are associated with a more pronounced reduction of the anterior capsule opening than hydrophobic acrylic IOLs. However, other authors have found no correlation between hydrophilicity of acrylic IOLs and anterior capsular shrinkage [111213]. Gonvers et al. [6] reported that anterior capsule contraction in eyes with plate-haptic silicone IOLs was more extensive than that in eyes with three piece silicone/polymethylmethacrylate IOLs. Some studies have reported no significant differences between single piece and three piece acrylic IOLs or between two haptic and four haptic IOLs [1114]. We evaluated changes in the anterior capsule opening at 1 day and 2 months after uncomplicated cataract surgery using single piece acrylic IOLs with different haptic designs.
Reduction of the anterior capsule opening results from an imbalance between the centripetal force of anterior capsular fibrosis and centrifugal force of the zonule [1516]. Anterior capsular fibrosis is induced by cytokines produced by lens epithelial cells (LEC) [17]. Blocking LEC proliferation, migration, and differentiation prevents anterior capsule contracture. Acrylic IOLs strongly adhere to the anterior capsule, which inhibits LEC migration [1819].
There was a significant reduction in anterior capsule opening at 2 months compared to 1 day after surgery for all three IOLs. This reduction was largest in the modified C-haptic IOL, followed by the plate-haptic IOL and the modified L-haptic IOL. Despite being composed of the same material and having the same hydrophilicity, in our study we measured less reduction of the anterior capsule opening with the modified L-haptic IOL than the modified C-haptic IOL. This suggests the haptic of the modified C-haptic IOL may have had poor tensile strength and did not overcome centripetal forces resulting from capsular fibrosis [2021]. The greater stability of the modified L-haptic IOL seemed to be related to proper tension on the bag along its equator which resulted in less change in the anterior capsulotomy area. A previous study reported that a single piece IOL with modified L-haptic showed less capsulotomy ovaling and maintained the capsular bag robustly [22]. Our result also supports the finding that the modified L-haptic design is associated with less anterior capsule contraction.
Plate-haptic designs are known to cause less stretching of the capsular bag and more pronounced anterior capsule contraction [56]. Previous studies have mostly evaluated cases of first generation silicone plate-haptic IOL implantation. Compared with past silicone IOLs with plate-haptic design, the acrylic IOLs with plate-haptic design used in this study have relatively larger overall diameters and interfacial haptic planes. These IOLs showed less contraction compared to modified C-haptic IOLs and were comparable to the modified L-haptic IOLs with regard to a reduction in anterior capsule contraction.
Single piece acrylic IOLs are known to produce less haptic force than three piece IOLs [23]. Hayashi and Hayashi [24] reported that single piece acrylic IOLs with modified-L haptic design resulted in no significant change in IOL decentration compared with three-piece acrylic IOLs. We found similar results for the degree of IOL decentration with the modified L-haptic design. In our study, decentration of the modified L-haptic design was significantly less than that of the modified C haptic IOL, although the difference was only less than 0.1 mm. This suggests that haptic design is associated with better IOL centration. In a correlation analysis, IOL decentration was positively correlated with the mean area reduction between the initial value and the value 2 months after surgery. Additionally, the strongest correlation was shown for the modified-C haptic IOL. Ohmi and Uenoyama [25] found that IOL decentration after surgery is influenced by asymmetric capsular contraction. When we performed a well-centered circular capsulotomy, the degree of IOL decentration was significantly different according to IOL type. It is possible that different haptic designs may result in different forces on the capsular bag and affect anterior capsulotomy shape after IOL implantation.
The strengths of our study include the relatively large population compared with previous studies and the prospective randomized study design. Although our study had a relatively short follow-up period, our results are instructive. It is known that anterior capsule contraction after cataract surgery progresses rapidly during the first month and then slows after 3 months [10]. The proliferation of LEC and capsular contracture are active for 3 months after surgery and the initial results correlate with later results. In our study, none of the patients presented with visually significant contracture during the first 2 months. We were able to observe uncomplicated changes to their anterior capsule openings.
In summary, our study demonstrated that contraction of the anterior capsule opening area was greater with the modified C-haptic IOL than modified L-haptic and palate haptic IOLs. The degree of IOL decentration was significantly different by IOL type, and showed a positive correlation with the mean area reduction over 2 months. Recently, acrylic has been a popular IOL material and IOL design is an important factor influencing outcomes. Anterior capsule contraction and IOL decentration vary according to IOL haptic design and, consequently, haptic design should be taken into consideration when determining the IOL to be used in selected cases.
References
1. Hara T, Azuma N, Chiba K, et al. Anterior capsular opacification after endocapsular cataract surgery. Ophthalmic Surg. 1992; 23:94–98. PMID: 1549302.

2. Jin-Poi T, Shatriah I, Khairy-Shamel ST, Zunaina E. Rapid anterior capsular contraction after phacoemulsification surgery in a patient with retinitis pigmentosa. Clin Ophthalmol. 2013; 7:839–842. PMID: 23674886.
3. Takamura Y, Tomomatsu T, Arimura S, et al. Anterior capsule contraction and flare intensity in the early stages after cataract surgery in eyes with diabetic retinopathy. J Cataract Refract Surg. 2013; 39:716–721. PMID: 23541898.

4. Davison JA. Capsule contraction syndrome. J Cataract Refract Surg. 1993; 19:582–589. PMID: 8229711.

5. Sickenberg M, Gonvers M, van Melle G. Change in capsulorhexis size with four foldable loop-haptic lenses over 6 months. J Cataract Refract Surg. 1998; 24:925–930. PMID: 9682111.

6. Gonvers M, Sickenberg M, van Melle G. Change in capsulorhexis size after implantation of three types of intraocular lenses. J Cataract Refract Surg. 1997; 23:231–238. PMID: 9113574.

7. Ursell PG, Spalton DJ, Pande MV. Anterior capsule stability in eyes with intraocular lenses made of poly(methyl methacrylate), silicone, and AcrySof. J Cataract Refract Surg. 1997; 23:1532–1538. PMID: 9456412.

8. Cochener B, Jacq PL, Colin J. Capsule contraction after continuous curvilinear capsulorhexis: poly(methyl methacrylate) versus silicone intraocular lenses. J Cataract Refract Surg. 1999; 25:1362–1369. PMID: 10511936.

9. Tsinopoulos IT, Tsaousis KT, Kymionis GD, et al. Comparison of anterior capsule contraction between hydrophobic and hydrophilic intraocular lens models. Graefes Arch Clin Exp Ophthalmol. 2010; 248:1155–1158. PMID: 20414785.

10. Hayashi K, Hayashi H, Nakao F, Hayashi F. Reduction in the area of the anterior capsule opening after polymethylmethacrylate, silicone, and soft acrylic intraocular lens implantation. Am J Ophthalmol. 1997; 123:441–447. PMID: 9124240.

11. Park TK, Chung SK, Baek NH. Changes in the area of the anterior capsule opening after intraocular lens implantation. J Cataract Refract Surg. 2002; 28:1613–1617. PMID: 12231321.

12. Vock L, Georgopoulos M, Neumayer T, et al. Effect of the hydrophilicity of acrylic intraocular lens material and haptic angulation on anterior capsule opacification. Br J Ophthalmol. 2007; 91:476–480. PMID: 17108011.

13. Saika S, Miyamoto T, Ohnishi Y. Histology of anterior capsule opacification with a polyHEMA/HOHEXMA hydrophilic hydrogel intraocular lens compared to poly(methyl methacrylate), silicone, and acrylic lenses. J Cataract Refract Surg. 2003; 29:1198–1203. PMID: 12842690.

14. Kim SY, Yang JW, Lee YC, Kim SY. Effect of haptic material and number of intraocular lens on anterior capsule contraction after cataract surgery. Korean J Ophthalmol. 2013; 27:7–11. PMID: 23372373.

15. Spalton DJ. Posterior capsular opacification after cataract surgery. Eye (Lond). 1999; 13(Pt 3b):489–492. PMID: 10627830.

16. Weiblinger RP. Review of the clinical literature on the use of the Nd:YAG laser for posterior capsulotomy. J Cataract Refract Surg. 1986; 12:162–170. PMID: 3517297.

17. Nishi O, Nishi K, Imanishi M. Synthesis of interleukin-1 and prostaglandin E2 by lens epithelial cells of human cataracts. Br J Ophthalmol. 1992; 76:338–341. PMID: 1622944.

18. Nagata T, Minakata A, Watanabe I. Adhesiveness of AcrySof to a collagen film. J Cataract Refract Surg. 1998; 24:367–370. PMID: 9559473.

19. Oshika T, Nagata T, Ishii Y. Adhesion of lens capsule to intraocular lenses of polymethylmethacrylate, silicone, and acrylic foldable materials: an experimental study. Br J Ophthalmol. 1998; 82:549–553. PMID: 9713064.

20. Richter-Mueksch S, Kahraman G, Amon M, et al. Uveal and capsular biocompatibility after implantation of sharp-edged hydrophilic acrylic, hydrophobic acrylic, and silicone intraocular lenses in eyes with pseudoexfoliation syndrome. J Cataract Refract Surg. 2007; 33:1414–1418. PMID: 17662434.

21. Moreno-Montanes J, Sanchez-Tocino H, Rodriguez-Conde R. Complete anterior capsule contraction after phacoemulsification with acrylic intraocular lens and endocapsular ring implantation. J Cataract Refract Surg. 2002; 28:717–719. PMID: 11955919.
22. Pandey SK, Werner L, Wilson ME Jr, et al. Capsulorhexis ovaling and capsular bag stretch after rigid and foldable intraocular lens implantation: experimental study in pediatric human eyes. J Cataract Refract Surg. 2004; 30:2183–2191. PMID: 15474834.
23. Lane SS, Burgi P, Milios GS, et al. Comparison of the biomechanical behavior of foldable intraocular lenses. J Cataract Refract Surg. 2004; 30:2397–2402. PMID: 15519095.

24. Hayashi K, Hayashi H. Comparison of the stability of 1-piece and 3-piece acrylic intraocular lenses in the lens capsule. J Cataract Refract Surg. 2005; 31:337–342. PMID: 15767155.

25. Ohmi S, Uenoyama K. Decentration associated with asymmetric capsular shrinkage and intraocular lens design in a rabbit model. J Cataract Refract Surg. 1995; 21:293–296. PMID: 7674165.

Fig. 1
Digital retroillumination photospots 1 day and 2 months after surgery. (A) Modified L-haptic IOL, (B) modified C-haptic IOL, (C) plate-haptic IOL. IOL = intraocular lens.
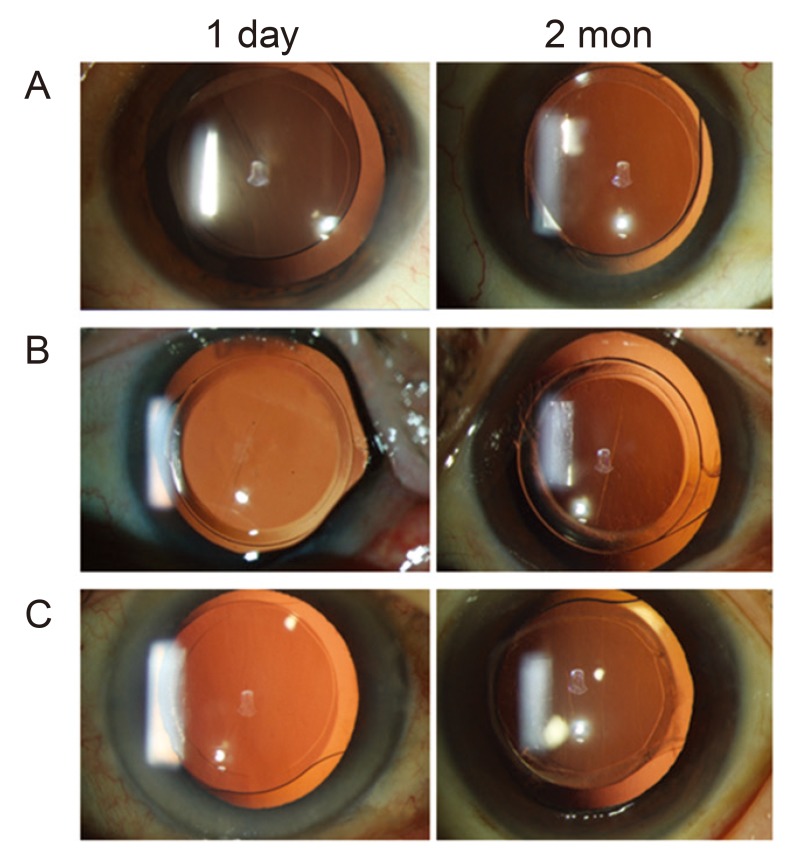
Fig. 2
Change in anterior capsule opening area (mm2) according to the three types of intraocular lenses. The asterisks denote a statistically significant difference: *p < 0.01, **p < 0.001.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download