Abstract
Purpose
To describe the demographics, relative incidence of subtypes, and clinical characteristics of blepharoptosis in Korean patients.
Methods
This is a retrospective, observational case series consisting of 2,328 patients who underwent ptosis surgery from 1991 to 2014 at a tertiary referral hospital in Korea. The patients were classified according to the type of ptosis and the evaluation of clinical characteristics including levator muscle function (LF) and degree of ptosis.
Results
Of the 2,328 patients, 1,815 (78%) had congenital ptosis and 513 (22%) had acquired ptosis. Simple congenital ptosis is the most common type overall (73.7%), and aponeurotic ptosis is the most common acquired type. More than three-quarters of eyes with congenital ptosis were affected in a moderate (34.4%) to severe degree (41.3%), and most of these eyes had fair (33.7%) to poor LF (60.1%). Among eyes with acquired ptosis, approximately three-quarters were affected in a mild (33.3%) to moderate degree (41.0%), with 63.3% of these eyes having good LF. The most widely used surgical technique was frontalis suspension (55.1%), followed by levator resection (29.0%) and aponeurosis repair (14.8%). At 3 years after the first surgery, 15.7% of patients with congenital ptosis and 10.4% of patients with acquired ptosis underwent reoperation.
Conclusions
Although the prevalence has decreased from previous years, the proportion of cases with congenital ptosis was higher in this study than has been shown in research conducted in the West. The majority of eyes with congenital ptosis was affected to a severe degree and had poor LF, while those with acquired ptosis were affected to a moderate degree and had good LF. More cases with acquired ptosis presented with fair to poor LF, and frontalis suspension surgery was performed more commonly compared to previous studies. The reoperation rate was higher in congenital ptosis compared to acquired ptosis.
Blepharoptosis, also referred to as ptosis, is an abnormally low position of the upper eyelids in primary gaze. Most patients with ptosis require surgery, and classifying the type of ptosis and then formulating a detailed strategy for the management of each type are essential for a good outcome.
There are numerous studies that classify the type of ptosis and evaluate demographic features [1234567]. However, these studies are somewhat dated, and more recent studies are lacking. Furthermore, most of the previous studies were conducted in the West. The awareness of the disease and demand for ptosis correction are affected by the era, the socio-economic status of the patient, and cultural factors including medical insurance coverage and the current standard of beauty. There are distinct cultural and racial differences between Asians and Westerners, and few large-scale studies evaluating patients with ptosis have been conducted, especially among Asian patients.
This is a large study conducted at a tertiary referral hospital that receives patients from around the country. We aim to present current clinical and demographic characteristics of Korean patients with ptosis and to compare this data with that from previous studies.
Approval for this study was obtained from the institutional review board and ethics committee (YUHS IRB 4-2016-0497). The study adhered to the tenets of the Declaration of Helsinki, and written informed consent was obtained from the parents or legal guardians of all patients if not from the patients themselves.
A review of the medical records of all patients with ptosis treated between 1991 and 2014 at a tertiary referral hospital in Seoul, South Korea was performed. All patients were operated on by a single surgeon (SYL). Information obtained from the medical records included the patients' clinical characteristics and past medical history including any previous surgeries for the treatment of ptosis.
The patients were classified as having congenital or acquired ptosis based primarily on the time of onset of the disorder. Additionally, the type of ptosis was determined based on patient history and clinical features. Physical examination included laterality of ptosis, levator muscle function (LF), degree of ptosis, intensity of skin crease, ocular motility, associated eyelid malpositioning, and pupil size [8]. LFs of infants or young children whose LF could not be measured accurately due to poor patient compliance were assessed as poor, fair, or good based on careful observation of eyelid and eyebrow movement, the existence of a double eyelid crease, Iliff's sign, degree of ptosis, and head posture. Standard photographs are shown in Fig. 1A, 1B.
We subdivided patients according to Beard's classification [9]. Congenital ptosis comprised simple, blepharophimosis-ptosis-epicanthus inversus syndrome, Marcus Gunn jaw-winking syndrome, and neurogenic ptosis. Acquired ptosis comprised aponeurotic, myogenic, mechanical, and neurogenic ptosis. We also followed Frueh's mechanistic classification, dividing our cases into myogenic, aponeurotic, mechanical, and neurogenic [1].
The severity of ptosis was classified according to Beard [39]: mild (margin reflex distance 1 [MRD1] of 3–4 mm), moderate (MRD1 of 2–3 mm), or severe (MRD1 of 0–2 mm). The LF was measured based on the methods of Berke [4]. If the LF was 8 mm or more, it was classified as good, between 5 and 8 mm was classified as fair, and 4 mm or less was classified as poor.
Reoperations were performed due to cosmetic or functional concerns such as undercorrection or overcorrection of ptosis; eyelid contour or crease deformity; eyelid malposition including entropion, ectropion, or retraction; granuloma formation; and recurrence of ptosis. The reoperation rate and surgical method used were investigated to estimate the surgical outcome. Patients with previous eyelid surgery and with <3 years of follow-up were excluded from the outcome analysis. The analysis was performed according to type of ptosis and surgical method.
A total of 3,190 eyes from 2,328 patients were included in this study. There were 236 patients who had undergone a previous surgery for the correction of ptosis. The average age of all patients was 17.3 years, and 1,336 patients (57.4%) were male.
There were 1,466 patients (63.0%) with unilateral ptosis and 862 patients with bilateral ptosis. Approximately 67% of the patients with congenital ptosis had unilateral disease, with the left eye being affected (52.2%) more often than the right eye. Among patients with acquired ptosis, 52% were affected by bilateral disease.
In 46% of the patients with congenital ptosis, LF could not be measured accurately due to poor patient compliance. It was assessed as poor in 94.5% and fair in 5.5% of the patients. When these patients were excluded from the analysis, the average LF measured 4.4 mm among the patients with congenital ptosis. Patients with acquired ptosis had an average LF of 8.7 mm. The demographic characteristics of all patients are presented in Table 1.
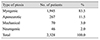
According to Beard's classification, the percentage of patients with congenital ptosis was greater at 78.0% than that of patients with acquired ptosis. Simple congenital ptosis without any concurrent anomalies comprised 94.5% of the cases of congenital ptosis. Among the cases of acquired ptosis, aponeurotic (52.1%) and myogenic (25.5%) were the most common (Table 2) [9]. Utilizing Frueh's mechanistic classification, myogenic was the most common (83.5%) type of ptosis (Table 3) [1].
The severity of ptosis is shown in Table 4. Among the cases of congenital ptosis, approximately 75% of eyes were of moderate to severe degree, while mild to moderate degrees were more common among cases of acquired ptosis.
Among cases with congenital ptosis, greater than 60% of eyes possessed poor LF, while 33.7% exhibited fair function. In contrast, 63.3% of eyes with acquired ptosis possessed good LF, while 12.2% possessed poor LF (Table 5).
The most common surgical technique used for correction of ptosis was frontalis suspension among cases of congenital ptosis and aponeurosis repair among cases of acquired ptosis. Autogenous fascia lata and silicone rods were the most commonly used suspension materials for correction of congenital and acquired ptosis, respectively (Table 6).
Reoperation data according to type of ptosis and surgical method are presented in Table 7. At 1, 2, and 3 years after the first surgery, 9.8%, 11.1%, and 15.7% of patients with congenital ptosis and 8.2%, 9.5%, and 10.4% of patients with acquired ptosis underwent reoperation, respectively. The reoperation rate increased over time. The cumulative rates of reoperation according to type of ptosis and surgical method are shown in Fig. 2A, 2B. The common surgical method of reoperation was autogenous fascia lata suspension surgery in cases of congenital ptosis and was the initial surgical method in acquired ptosis. The proportion of patients who underwent more than three surgeries was <5% in cases of both congenital and acquired ptosis.
The classification of ptosis plays an essential role in determination of the treatment plan because of the varying etiologies and features among the different types of ptosis. Congenital ptosis, which is present at the time of birth, is caused by dystrophy of the levator muscle. Therefore, it is related to poor LF, weak or absent eyelid crease, and lid lag. On the other hand, acquired ptosis is mainly caused by separation of the levator aponeurosis from the tarsal plate and is related to good LF, high eyelid crease, deepening of the upper sulcus, elevation of the eyebrow, and relatively late symptom onset [7810].
In 1972, Fox [11] classified ptosis as congenital, acquired, or heredofamilial and further subdivided acquired ptosis into neurogenic, myogenic, traumatic, and senile. In 1989, Beard [9] presented the classification scheme of congenital, acquired, and pseudoptosis and further divided acquired cases into myogenic, neurogenic, traumatic, and mechanical. In 1980, Frueh [1] suggested that such classification schemes were complex and confusing and instead proposed the mechanistic classification scheme of neurogenic, myogenic, aponeurotic, and mechanical.
In this study, patients were classified using historical classification schemes. We divided patients with ptosis into congenital and acquired groups based on the timing of development of the disorder. This classification scheme does not specify the cause of the ptosis, but is still useful in determining the appropriate surgical technique for correction of the disorder.
Previous studies have shown varying proportions of congenital and acquired ptosis. In 1949, Berke [4] reported that 88% of 200 ptosis patients had the congenital disease. In a study of 142 ptosis patients by Carbajal in 1958 [5], it was reported that 97% of the cases were congenital and 3% were acquired. In 1969, Smith et al. [6] reported that 67% of the cases were congenital, and in 1972, Fox [11] reported that 65% of the cases were congenital, 15% were heredofamilial, and 20% were acquired. In contrast, more recent studies have reported a smaller proportion of cases with congenital ptosis. In 1990, Rathbun [12] reported that 69% of ptosis patients possessed an aponeurotic defect, and only 20% of those were congenital. Other studies also reported a low proportion of cases with congenital ptosis: Clauser et al. [7] with 28.5% and Lim et al. [13] with 10.4%.
In our research, the proportion of cases with congenital ptosis was 78.0%. In previous studies evaluating Korean patients, the ratio of cases with congenital ptosis also decreased with time: 94% in 1979 [14], 91% in 1985 [15], 86% in 1995 [16], and 76% in 2005 [17]. Rathbun [12] suggested that the reason for the increased proportion of cases with acquired ptosis was the increased number of aged persons and the increased social acceptance of reconstructive procedures for the correction of aging changes. Improvement in socio-economic status and increased demand for a more aesthetic appearance are believed to have led to the increased recognition of acquired ptosis. However, the ratio of cases with congenital ptosis was still higher among Korean patients than it was among Westerners. Anatomical differences in the upper eyelid such as orbicularis hypertrophy, thick upper eyelid, or weak LF in Koreans were presented as the causes [16].
It is widely accepted that pure congenital ptosis is usually unilateral, while acquired ptosis can be bilateral or unilateral [810]. Our results supported this observation. Left eye predominance in cases of unilateral congenital ptosis was reported by Griepentrog et al. [18]. The authors suggested that simple congenital ptosis might be associated with an underlying failure of proper motor innervation as seen with Duane's retraction syndrome, which also shows left eye predominance. In this study, left eye involvement was more common, but this result did not reach statistical significance (p = 0.24). A higher frequency of males (67.2%) possessing congenital ptosis in our study also correlates with previous studies (60% to 63%) [1920].
Congenital ptosis was subdivided into simple congenital ptosis and unusual ptosis such as blepharophimosis, Marcus Gunn jaw-winking syndrome, superior rectus muscle weakness, congenital fibrosis, and 3rd nerve palsy. Acquired ptosis was subdivided into aponeurotic, myogenic, neurogenic, traumatic, and mechanical ptosis.
The most common type of congenital ptosis in our study was simple congenital ptosis, and the ratio of 94.5% was greater than previous reports of 74% to 85% [316181920]. Marcus Gunn jaw-winking syndrome represented 3.8% and 5% of congenital ptosis, blepharophimosis 2.8% and 4.5%, and congenital 3rd nerve palsy 2.8% and 7.7% in the first population-based study on the incidence of childhood ptosis in Minnesota [18] and a large 10-year review in the United Kingdom [20], respectively. In our study, unusual types of congenital ptosis other than simple were seen with relatively low frequency.
The type of acquired ptosis seen most frequently in our study was aponeurotic, followed by myogenic, neurogenic, traumatic, and mechanical ptosis. Common disorders causing myogenic ptosis include myasthenia gravis, myotonic dystrophy, chronic progressive external ophthalmoplegia, and oculopharyngeal-muscular dystrophy [21]. Myasthenia gravis and chronic progressive external ophthalmoplegia were the leading causes of myogenic ptosis among our patients.
Simple congenital ptosis is caused by dystrophy of the levator muscle. In our study, the second most common type of acquired ptosis after aponeurotic was myogenic. The high prevalence of myogenic ptosis therefore seems natural according to the mechanistic classification. These findings were similar to previous reports [17].
LF is related to the degree of ptosis, that is, the lower is the LF, the greater is the eyelid drooping [8]. Classically, acquired ptosis is known to be associated with good LF and less severe lid drooping [8]. In our study, approximately 75% of the eyes with acquired ptosis had mild to moderate lid drooping, but only 63.3% exhibited good LF. The average LF was 8.7 mm, and 24.5% of the eyes were determined to have fair LF. Kim and Lee [22] reported that Korean patients with involutional ptosis had decreased LF compared to Caucasian patients. The authors suggested that decreased LF was another possible mechanism causing involutional ptosis in Koreans and could be attributed to weakening of the levator muscle or aponeurosis itself and heavier eyelids endogenous to Koreans. Another study reported the average LF of Korean patients aged 50 years or older with ptosis as 10.0 mm, a value less than that of Caucasians [23]. The authors also commented on the thick orbicularis muscle and prominence of fat tissue in Koreans [23]. The contribution of abnormalities in the levator muscle itself to involutional ptosis has also been reported in a Western study [24]. A large proportion of cases with severe ptosis and poor LF among those with congenital ptosis was also noted in this study.
Regarding surgical techniques, Clauser et al. [7] most commonly performed levator resection (71.8%), followed by frontalis suspension. However, in this study, frontalis suspension was the most commonly performed surgery. A larger proportion of patients with congenital ptosis and poor LF could lead to increased performance of frontalis suspension surgery, especially using autogenous fascia lata. Silicone rods were commonly used in young patients with congenital ptosis from whom autogenous fascia lata could not be harvested and in cases of acquired ptosis with poor eye protection.
The reoperation rate was higher in congenital ptosis than acquired ptosis. Possible causes are poorer LF, an inaccurate preoperative examination due to low cooperation of young patients, and the lower predictability of surgery performed under general anesthesia in cases of congenital ptosis. The rate increased over time, and the increase was high in Supramid Extra and silicone rod suspension surgeries. The primary cause of late reoperation was recurrence, and these suspension materials were associated with high recurrence [2526]. Supramid Extra and silicone rods were used for temporary treatment in very young patients with congenital ptosis. Most patients with recurrence underwent autogenous fascia lata suspension for the second surgery. However, the silicone rod suspension surgical method was commonly used during reoperation in acquired ptosis, even in cases of recurrence, because the silicone rods were used in adult patients with a high risk of corneal exposure [26].
The retrospective nature of our study is one of its limitations. The LF was only a rough estimate in patients who were too young to have it measured accurately. We could not investigate the surgical success rate accurately, as large numbers of the patients included in this study underwent surgery long ago and their postoperative photographs were unavailable. The reoperation rate was investigated instead of the success rate, but the cumulative reoperation rate was somewhat inaccurate because of the varying follow-up period. Another implicit limitation in our study is selection bias. Only patients who underwent surgical correction of ptosis were included in this study. Patients with mild to moderate ptosis who did not require surgery were excluded, and this might have underestimated the prevalence of less severe disease. Furthermore, the larger proportion of cases of congenital ptosis at our institution could be due to our status as a tertiary referral hospital, where patients who require general anesthesia for ptosis correction are more likely to be sent. A proportion of adult patients with mild to moderate ptosis could have surgery performed at a primary or secondary hospital. Further research including patients who did not require corrective surgery or a nationwide study would be helpful to evaluate the overall characteristics of ptosis in Korea.
In conclusion, congenital ptosis was more common among our patients than the acquired. It exhibited a similar trend of decreased prevalence, but was still more common than was seen in research conducted in the West. More patients with acquired ptosis in our study presented with fair to poor LF compared to Westerners. Clinicians should consider these differences when determining the appropriate surgical technique. This study could help in identifying the characteristics of patients with blepharoptosis among the Korean population.
Figures and Tables
Fig. 1
Standard photographs for evaluating levator muscle function (LF) of a young patient whose LF could not be measured accurately. (A) An inert eyelid, extensive eyebrow elevation, no double eyelid crease, severe lid drooping, and chin lifting head posture suggested poor LF (left eye), (B) compared with fair LF suggested by some movement of the eyelid especially on vertical gaze, a double eyelid crease, and mild lid drooping (left eye).

Fig. 2
The cumulative rate of reoperation in (A) congenital and (B) acquired ptosis according to surgical method. AR = aponeurosis repair; LR = levator resection; FL = autogenous fascia lata suspension; SE = Supramid Extra suspension; SR = silicone rod suspension.

Table 1
Demographic characteristics of the patients

Values are presented as number (%) or mean ± SD unless otherwise indicated.
SD = standard deviation; min = minimum; max = maximum; LF = levator muscle function; PF = palpebral fissure width.
*Excluding patients whose LF could not be measured accurately due to poor patient compliance. Of the excluded patients, 94.5% were assessed as having poor LF and 5.5% as having fair LF.
References
2. Fox SA. Ophthalmic plastic surgery. 5th ed. New York: Grune & Stratton;1976. p. 353–359.
3. Beard C. Ptosis. 3rd ed. St. Louis: Mosby;1981. p. 39–75.
4. Berke RN. Congenital ptosis; a classification of 200 cases. Arch Ophthal. 1949; 41:188–197.
6. Smith B, McCord CD, Baylis H. Surgical treatment of blepharoptosis. Am J Ophthalmol. 1969; 68:92–99.

7. Clauser L, Tieghi R, Galie M. Palpebral ptosis: clinical classification, differential diagnosis, and surgical guidelines: an overview. J Craniofac Surg. 2006; 17:246–254.
8. Nerad JA. Evaluation and treatment of the patient with ptosis. In : Nerad JA, editor. Oculoplastic surgery: the requisites in ophthalmology. St. Louis: Mosby;2001. p. 157–192.
10. de Figueiredo AR. Blepharoptosis. Semin Ophthalmol. 2010; 25:39–51.
11. Fox SA. A new ptosis classification: late spontaneous ptosis. Arch Ophthalmol. 1972; 88:590–593.
12. Rathbun JE. Eyelid surgery. 1st ed. Boston: Little Brown;1990. p. 201–217.
13. Lim JM, Hou JH, Singa RM, et al. Relative incidence of blepharoptosis subtypes in an oculoplastics practice at a tertiary care center. Orbit. 2013; 32:231–234.

14. Ahn YS, Lee TS. Clinical observation and their surgical results of 67 cases of blepharoptosis. J Korean Ophthalmol Soc. 1979; 20:283–290.
15. Kim HM, Lee TS. Clinical observation and their surgical results of 127 cases of blepharoptosis. J Korean Ophthalmol Soc. 1985; 26:441–448.
16. Kim SY, Chung WS. Analysis of the causes of ptosis. J Korean Ophthalmol Soc. 1995; 36:1649–1654.
17. Kim IS, Choi JB, Rah SH, Lee SY. Classification of ptosis in Korea. J Korean Ophthalmol Soc. 2005; 46:1262–1269.
18. Griepentrog GJ, Diehl NN, Mohney BG. Incidence and demographics of childhood ptosis. Ophthalmology. 2011; 118:1180–1183.

19. Lee V, Konrad H, Bunce C, et al. Aetiology and surgical treatment of childhood blepharoptosis. Br J Ophthalmol. 2002; 86:1282–1286.

20. Berry-Brincat A, Willshaw H. Paediatric blepharoptosis: a 10-year review. Eye (Lond). 2009; 23:1554–1559.

21. Finsterer J. Ptosis: causes, presentation, and management. Aesthetic Plast Surg. 2003; 27:193–204.

22. Kim CY, Lee SY. Distinct features in Koreans with involutional blepharoptosis. Plast Reconstr Surg. 2015; 135:1693–1699.

23. Park CY, Jeon SL, Woo KI, Chang HR. The frequency and aspects of ptosis in Korean old age. J Korean Ophthalmol Soc. 2007; 48:205–210.
24. Pereira LS, Hwang TN, Kersten RC, et al. Levator superioris muscle function in involutional blepharoptosis. Am J Ophthalmol. 2008; 145:1095–1098.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download