Abstract
Purpose
Methods
Results
Conclusions
Figures and Tables
Fig. 1
Cataract grade according to standard photos of wide-field fundus imaging. (A) Grade 1, clearly visible or slightly obscured macular area. (B) Grade 2, mildly obscured macular area. (C) Grade 3, moderately obscured, but distinguishable macular area. (D) Grade 4, severely obscured, undistinguishable macular area.

Fig. 2
Percentage constituents of nuclear opalescence (NO), cortical opacities (CO), and posterior subcapsular cataracts (PSC) with the Lens Opacities Classification System III (LOCS III) in cataract grade based on wide-field fundus imaging. (A) NO with the LOCS III. (B) CO with the LOCS III. (C) PSC with the LCOS III.

Fig. 3
Cataract grade 4 eye without segmentation errors on spectral domain optical coherence tomography. (A) Wide-field fundus imaging shows a dense localized cataract artifact. (B) Spectral domain optical coherence tomography measurements do not show segmentation errors in either the inner or outer boundary line.

Fig. 4
Eyes with segmentation errors on spectral domain optical coherence tomography (SD-OCT). (A) A segmentation error on SD-OCT is observed only in the inner boundary line, and the automated segmentation line identifies the inner boundary line posterior to the actual inner limiting membrane. (B) A segmentation error on SD-OCT is observed in both the inner and outer boundary lines, and the automated segmentation line identifies the inner boundary line posterior to the actual inner limiting membrane and the outer boundary line posterior to the actual retinal pigment epithelium.

Table 1
Clinical characteristics of study participants and their eyes according to cataract grade on wide-field fundus imaging

Values are presented as mean ± standard deviation or number (%); Cataract grade was classified from 1 to 4 according to the standard fundus photos of the Optos Optomap: grade 1, clearly visible or slightly obscured macular area; grade 2, mildly obscured macular area; grade 3, moderately obscured, but distinguishable macular area; and grade 4, severely obscured, undistinguishable macular area.
*Analysis of variance test comparing normally distributed variables among cataract grade groups; †Fisher exact test comparing categorical variables among cataract grade groups.
Table 2
Correlation analyses among cataract grades on wide-field fundus imaging, age, LOCS III, SNR, and total macular thickness on SD-OCT
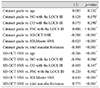
Cataract grade was classified from 1 to 4 according to the standard fundus photos of the Optos Optomap.
LOCS III = Lens Opacities Classification System III; SNR = signal-to-noise ratio; CC = correlation coefficient; NO = nuclear opalescence; CO = cortical opacity; PSC = posterior subcapsular cataracts; SD-OCT = spectral domain optical coherence tomography.
*Pearson correlation analysis; †Spearman correlation analysis.
Table 3
SNR and macular thickness of SD-OCT according to cataract grade with wide-field fundus imaging

Table 4
Segmentation errors in SD-OCT according to cataract grade on wide-field fundus imaging and SD-OCT SNR (χ2 linear trend test)
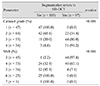
Segmentation error: inner boundary lines do not correspond to internal limiting membranes and outer boundary lines do not correspond to retinal pigment epithelia in SD-OCT; Cataract grade was classified from 1 to 4 according to the standard fundus photos of the Optos Optomap.
SD-OCT = spectral domain optical coherence tomography; SNR = signal-to-noise ratio.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download