Abstract
Purpose
To evaluate and compare visual acuity and reading speed for Korean language between a diffractive bifocal and trifocal intraocular lens (IOL) of the same material and haptic design.
Methods
We reviewed the medical records of the patients who had undergone bilateral cataract surgery with bifocal IOLs (AT LISA 801) on the both eyes (bifocal group) and trifocal IOLs (AT LISA tri 839 MP, trifocal group). The main outcome measures were the uncorrected distance, intermediate, and near visual acuity (uncorrected distance visual acuity [UCDVA], uncorrected intermediate visual acuity [UCIVA], and uncorrected near visual acuity [UCNVA]) and corrected distance, near, and distance-corrected intermediate visual acuity (corrected distance visual acuity [CDVA], corrected near visual acuity [CNVA], and distance-corrected intermediate visual acuity [DCIVA]) at last postoperative follow-up month. Reading speeds for Korean language were measured to check near visual function.
Results
Fourteen eyes (7 patients) were included in the bifocal group and 32 eyes of 16 patients in the trifocal group. There were no statistical differences between the two groups with respect to UCDVA, UCNVA, CDVA, and CNVA. However, UCIVA (0.35 vs. 0.22 logarithm of the minimum angle of resolution [logMAR], p < 0.01) and DCIVA (0.34 vs. 0.20 logMAR, p < 0.01) were significantly better in the trifocal group than in the bifocal group. The mean reading speed for logMAR 0.5 optotype (point 10) was 86.50 words per minute (wpm) in the bifocal group and 81.48 wpm in the trifocal group without a significant difference (p = 0.70).
Monofocal intraocular lens (IOL) previously required reading glasses for near vision after cataract surgery. Multifocal IOLs were developed to reduce spectacle dependence. They provided better uncorrected near visual acuity [123]. In addition, to provide better intermediate vision, trifocal IOLs were developed, which provided three main foci for far, near and intermediate [45678910].
Studies have focused on comparison between bifocal and trifocal IOLs [5111213]. Basically, visual acuity was the main outcome to compare bifocal with trifocal IOLs [1113]. However, good visual acuity does not always mean good near function, which is needed for reading books or newspapers. Jonker et al. [11] tried to compare reading functions between bifocal and trifocal IOLs. However, there have been no comparative studies, to date, of the reading functions for Korean language achieved with a diffractive bifocal and trifocal IOL of the same material and haptic design. Therefore, the goal of this study was to compare not only visual acuities but also reading speeds for evaluating reading functions with a diffractive bifocal and trifocal IOL of the same material and haptic design.
We reviewed charts for two patient groups undergoing bilateral cataract surgery from September, 2011 to November, 2015. One group was the bifocal group, implanted with the bifocal diffractive IOL AT LISA 801 (Carl Zeiss Meditec, Jena, Germany), and another group was the trifocal group, implanted with the trifocal diffractive IOL AT LISA tri 839 MP (Carl Zeiss Meditec). The same type of IOL was implanted in both eyes of each patient.
The inclusion criteria were patients with cataract or presbyopia/pre-presbyopia who did not want to wear reading glasses, aged over 40 years and with follow-up of at least 1 month. The exclusion criteria were patients with a history of previous ocular surgery, complications during surgery, glaucoma, corneal disease, iris disease, retinal problems, and any other ocular pathology that would limit postoperative visual outcome.
This study was approved by our institutional review board (IRB number: 2016-08-004) and all procedures were conducted according to the Declaration of Helsinki. Written informed consent was obtained from all patients.
Before surgery, a full ophthalmic examination was performed, including manifest refraction, keratometry, slitlamp examination, Goldmann applanation tonometry, fundus examination, uncorrected (UCDVA) and corrected distance visual acuity (CDVA) using the Early Treatment of Diabetic Retinopathy Study chart at 4 m, uncorrected (UCIVA) and distance-corrected intermediate visual acuity (DCIVA) at 80 cm, and uncorrected (UCNVA) and corrected near visual acuity (CNVA) at 40 cm. After postoperative 1 month, in addition to a full ophthalmic examination, reading speed was also evaluated.
Reading speed was measured by third generation retina display iPad (iPad Retina Display; Apple, Cupertino, CA, USA) at 40 cm distance. The application used in this study had been introduced by Song et al. [14]. The iPad (screen size 9.7", screen resolution 2,048 × 1,536) was set to maximum brightness in the display settings throughout all testing procedures. Letter size was presented logarithm of the minimum angle of resolution (logMAR) 0.0 to 1.0 at 0.1 logMAR steps. Patients were asked to read the sentence and then went on to the next stage, which displayed a smaller print sentence. After the test was completed, the application automatically calculated the reading speed (words per minute/letters per minute).
All surgeries were performed by the same experienced surgeon using a standard phacoemulsificaiton technique through a 2.2-mm clear corneal incision. All incisions were made at the steep axis. All IOLs were inserted into the capsular bag. A postoperative topical therapy was prescribed with a combination of topical antibiotics (moxifloxacin hydrochloride; Vigamox, Alcon, Fort Worth, TX, USA), steroid (dexamethasone; Maxidex, Alcon) at 4 times daily, and artificial tear eyedrops frequently for 1 month.
Mann-Whitney U-test was used to compare two groups for visual acuity and reading speed. Wilcoxon signed rank test was used for comparison between preoperative and postoperative visual acuity in bifocal group. Paired t-test was used to compare preoperative and postoperative visual acuity in trifocal group. A p-value <0.05 was considered statistically significant. SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis.
The bifocal group included 14 eyes of 7 patients and the trifocal group included 32 eyes of 16 patients. In bifocal group, 2 patients were male; and in trifocal group, 9 patients were male. Mean age of bifocal group and trifocal groups were 59.43 ± 6.07 and 57.50 ± 7.03, respectively, without significant differences (p = 0.39). Bifocal group showed significantly longer follow-up period than trifocal group (17.43 vs. 2.44 months, p < 0.01). No statistically significant differences were observed in terms of preoperative refractive results and CDVA between the two groups (Table 1). In both groups, there were significant differences between preoperative and postoperative CDVA (p = 0.04 in the bifocal group and p < 0.01 in the trifocal group).
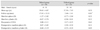
At last follow-up month, postoperative UCDVA, CDVA, UCNVA, and CNVA were not significantly different. However, statistically significantly better mean visual acuity was present in the trifocal group for postoperative UCIVA (0.35 vs. 0.22 logMAR, p < 0.01) and DCIVA (0.34 vs. 0.20 logMAR, p < 0.01) (Table 2). No statistically significant differences were observed in postoperative refractive results between the two groups (Table 1).
Postoperative reading speed at last follow-up month was double checked by words per minute and letters per minute. The mean reading speed for logMAR 0.5 optotype (point 10) was 86.50 ± 16.34 words per minute (wpm) and 218.72 ± 77.83 letters per minute (lpm) in bifocal group and 81.48 ± 27.33 wpm and 235.58 ± 81.30 lpm in trifocal group, with no significant group wise differences (p = 0.70 and 0.53, respectively). In addition, no statistically significant differences were found in postoperative reading speed between two groups at any letter sizes (Table 3, 4).
Patients with implanted multifocal IOLs may not desire spectacles. Thus, it is important for them to read books, newspapers or smart phones comfortably without reading glasses. Thus, many studies for multifocal IOLs have evaluated near visual acuities [347891011131516]. However, near visual acuity cannot fully represent actual near visual functions like reading functions. For checking reading function, Rasp et al. [17] compared reading acuity, reading distance and reading speed by using the Salzburg Reading Desk [18] among four bifocal IOLs and one monofocal IOL. They confirmed that multifocal IOLs with diffractive component provided better reading performance than that obtained with a refractive multifocal or monofocal IOL.
In this study, thus, we compared reading speed for Korean language between trifocal and bifocal IOL of the same material and haptic design. The mean reading speed for logMAR 0.5 optotype (point 10), which is used for newspaper font size was 86.50 ± 16.34 wpm in bifocal group and 81.48 ± 27.33 wpm in the trifocal group, without significant differences (p = 0.70). In addition, no statistically significant differences were found in postoperative reading speed between two groups at any letter sizes. This result was the same as reported by Jonker et al. [11] However, there could be some limitation at comparing these two groups directly because the follow-up period of the trifocal group was shorter than that of the bifocal group. For example, in bifocal group, there could be more neural adaptation which can affect reading speed. Thus, further study with same long follow-up periods is needed.
Song et al. [14] showed the mean reading speed for logMAR 0.5 optotype was 202.3 ± 88.4 wpm. This result looks faster than our results. However, in their study, the mean age of participants was 30.1 ± 4.5 and all participants had no any eye diseases. In this study, the mean ages of both groups were in the sixth decade and all participants got cataract surgery. These differences could explain this different result.
For trifocal IOL, Jonker et al. [11] evaluated reading function by using the Salzburg Reading Desk. The study used 2 types of IOLs: the Finevision Micro F trifocal IOL (PhysIOL, Liege, Belgium) and the Acrysof Restor IQ +3.0 diopters bifocal IOL (Alcon). They showed that there were no statistically significant differences in reading speed and reading acuity between two groups. However, the IOLs used in that study differed in material and haptic design. The trifocal IOL is a diffractive IOL made of a hydrophilic acrylic with an ultraviolet- and blue-light inhibitor, but the bifocal IOL is a diffractive IOL made of a hydrophobic acrylate/ methacrylate copolymer with an ultraviolet- and blue-light blocker [56].
In addition, Jonker et al. [11] showed mean reading speed of trifocal IOL group was 145.3 ± 32.9 wpm and that of bifocal IOL group was 144.6 ± 38.5 wpm. This difference could be explained by the difference of languages, which was used in each application (English vs. Korean language).
Trifocal IOLs were developed to provide three main foci for far, near and intermediate. However, distribution of light at three foci unavoidably causes decreasing the amount of energy to far and near, and so it might affect visual acuities at all distances [19]. Therefore, there have been many studies to evaluate performance of trifocal IOLs [456789101112131516].
Gatinel and Houbrechts [5] and Madrid-Costa et al. [12] compared trifocal with bifocal IOLs by using an optical bench. Gatinel and Houbrechts [5] showed that intermediate vision was more prominent with the trifocal IOL. Madrid-Costa et al. [12] showed that the trifocal IOL provided a better optical quality at the −1.5 diopters focal point.
Jonker et al. [11] and Mojzis et al. [13] compared trifocal with bifocal IOLs by using visual acuity basically. According to study of Jonker et al. [11], there were no statistically significant differences in visual acuities at any distances. They concluded that the trifocal IOL had noninferiority of visual outcomes, as compared with the bifocal IOL. On the other hand, Mojzis et al. [13] showed that there were no significant differences in distance visual acuities between two groups, but uncorrected and corrected near and intermediate visual acuities were significantly better in the trifocal group.
In the current study, postoperative UCDVA, CDVA, UCNVA, and CNVA were statistically no significantly different between two groups. However, postoperative UCIVA and DCIVA were significantly better in trifocal group than bifocal group. This result was closer to the study of Mojzis et al. [13] than that of Jonker et al. [11]. The reason why trifocal IOLs has better intermediate vision could be explained their ability to distribute light to far, near and intermediate distances. In addition, better optical quality at intermediate distance was confirmed by Gatinel and Houbrechts [5] and Madrid-Costa et al. [12]. In contrast, Mojzis et al. [13] reported no statistically significant differences in near visual acuity between two groups in this study. Near visual acuity could be affected by pupil size, pseudo-accommodation made by myopia or astigmatism, etc. [2021]. Therefore, it could differ with different circumstances of studies.
The limitations of this study were that it was a retrospective nonrandomized study. The trifocal IOL investigated in this study has been recently introduced, so the follow-up period of the trifocal group was shorter than that of the bifocal group. There were no preoperative reading speeds of both groups. However, preoperative reading speeds could be less important because both groups had cataract which could affect reading speeds. In addition, contrast sensitivity, ocular aberrations, or defocus curve were not evaluated because these are already well published. Thus, a prospective randomized study with long follow-up is needed.
In conclusion, trifocal diffractive IOLs provide same level of distance and near visual acuity and reading speed, that is near visual function, as that of bifocal diffractive IOLs. In addition, they provide better intermediate visual acuity over bifocal IOLs. Therefore, trifocal diffractive IOLs could be one of the choices for correcting cataract and presbyopia.
Figures and Tables
Table 2
Preoperative and postoperative visual acuity (logMAR) at the last follow-up month

Values are presented as mean ± standard deviation.
logMAR = logarithm of minimal angle of resolution; CDVA = corrected distance visual acuity; UCDVA = uncorrected distance visual acuity; UCIVA = uncorrected intermediate visual acuity; DCIVA = distance-corrected intermediate visual acuity; UCNVA = uncorrected near visual acuity; CNVA = corrected near visual acuity.
*<0.05 Mann-Whitney U-test.
References
1. Calladine D, Evans JR, Shah S, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2012; CD003169.

2. Javitt JC, Steinert RF. Cataract extraction with multifocal intraocular lens implantation: a multinational clinical trial evaluating clinical, functional, and quality-of-life outcomes. Ophthalmology. 2000; 107:2040–2048.
3. Nijkamp MD, Dolders MG, de Brabander J, et al. Effectiveness of multifocal intraocular lenses to correct presbyopia after cataract surgery: a randomized controlled trial. Ophthalmology. 2004; 111:1832–1839.

4. Cochener B, Vryghem J, Rozot P, et al. Visual and refractive outcomes after implantation of a fully diffractive trifocal lens. Clin Ophthalmol. 2012; 6:1421–1427.

5. Gatinel D, Houbrechts Y. Comparison of bifocal and trifocal diffractive and refractive intraocular lenses using an optical bench. J Cataract Refract Surg. 2013; 39:1093–1099.

6. Gatinel D, Pagnoulle C, Houbrechts Y, Gobin L. Design and qualification of a diffractive trifocal optical profile for intraocular lenses. J Cataract Refract Surg. 2011; 37:2060–2067.

7. Lesieur G. Outcomes after implantation of a trifocal diffractive IOL. J Fr Ophtalmol. 2012; 35:338–342.
8. Mojzis P, Pena-Garcia P, Liehneova I, et al. Outcomes of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2014; 40:60–69.

9. Sheppard AL, Shah S, Bhatt U, et al. Visual outcomes and subjective experience after bilateral implantation of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2013; 39:343–349.

10. Voskresenskaya A, Pozdeyeva N, Pashtaev N, et al. Initial results of trifocal diffractive IOL implantation. Graefes Arch Clin Exp Ophthalmol. 2010; 248:1299–1306.

11. Jonker SM, Bauer NJ, Makhotkina NY, et al. Comparison of a trifocal intraocular lens with a +3.0 D bifocal IOL: results of a prospective randomized clinical trial. J Cataract Refract Surg. 2015; 41:1631–1640.

12. Madrid-Costa D, Ruiz-Alcocer J, Ferrer-Blasco T, et al. Optical quality differences between three multifocal intraocular lenses: bifocal low add, bifocal moderate add, and trifocal. J Refract Surg. 2013; 29:749–754.

13. Mojzis P, Kukuckova L, Majerova K, et al. Comparative analysis of the visual performance after cataract surgery with implantation of a bifocal or trifocal diffractive IOL. J Refract Surg. 2014; 30:666–672.

14. Song J, Kim JH, Hyung S. Validity of Korean version reading speed application and measurement of reading speed: pilot study. J Korean Ophthalmol Soc. 2016; 57:642–649.

15. Alio JL, Montalban R, Pena-Garcia P, et al. Visual outcomes of a trifocal aspheric diffractive intraocular lens with microincision cataract surgery. J Refract Surg. 2013; 29:756–761.

16. Lee SC, Kim JW, Lim TH, et al. Clinical outcomes of diffractive aspheric trifocal intraocular lens implantation. J Korean Ophthalmol Soc. 2015; 56:1338–1344.

17. Rasp M, Bachernegg A, Seyeddain O, et al. Bilateral reading performance of 4 multifocal intraocular lens models and a monofocal intraocular lens under bright lighting conditions. J Cataract Refract Surg. 2012; 38:1950–1961.

18. Dexl AK, Schlogel H, Wolfbauer M, Grabner G. Device for improving quantification of reading acuity and reading speed. J Refract Surg. 2010; 26:682–688.

19. Montes-Mico R, Madrid-Costa D, Ruiz-Alcocer J, et al. In vitro optical quality differences between multifocal apodized diffractive intraocular lenses. J Cataract Refract Surg. 2013; 39:928–936.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download