Abstract
Purpose
To assess the clinical outcomes following botulinum neurotoxin type A (BoNT-A) treatment with an individualized injection technique based on the types of spasms and to compare the results of the individualized injection technique with those of the conventional injection technique in the same patients.
Methods
From November 2011 to July 2013, 77 BoNT-A injections were performed in 38 patients. Eighteen patients were treated with conventional BoNT-A injections before 2011, and 20 patients were referred to our hospital for unsatisfactory results after a conventional injection technique. We classified the patients by spasm-dominant sites: the lateral orbital area, representing the orbital orbicularis-dominant group (ODG); the glabella, representing the corrugator-dominant group (CDG); and the ptosis, representing the palpebral part of the orbicularis-dominant group (PDG). We increased the injection dose into the spasm-dominant sites of the blepharospasm groups. We assessed subjective symptom scores (functional disability score, FDS) after treatment.
Results
This study included 38 patients (26 women, 12 men; mean age, 60.6 ± 10.9 years). There were 21 patients in the ODG, 10 patients in the CDG, and 7 patients in the PDG. Mean ages were 59.7 ± 12.6, 59.8 ± 8.5, and 66.8 ± 9.0 years, and mean BoNT-A injection dose was 38.8 ± 11.2, 38.8 ± 11.2, and 38.8 ± 10.8 U in each group, respectively (p = 0.44, 0.82 Kruskal-Wallis test). Mean FDS after injection was 1.7 ± 0.7 in the ODG, 1.4 ± 0.8 in the CDG, and 1.2 ± 0.3 in the PDG. There were significant differences in reading and job scale among the three groups. In a comparison between the conventional and individualized injection techniques, there was a significant improvement in mean FDS and in the reading scale in the PDG with the individualized injection technique. The success rate was 92.1% in the conventional injection group and 94.1% in the individualized injection group.
Essential blepharospasm is a neuromuscular disorder presenting as bilateral, involuntary, persistent and spastic contraction of the orbicularis oculi, proceus muscle and corrugator muscle, which tends to run a progressive course [1]. The orbicularis oculi spasms may increase in frequency and severity to the point of functional blindness. The spasms are usually bilateral and are absent during sleep. Many patients gradually stop reading, watching television, and driving and avoid social contact [2]. The pathophysiology remains unknown, but the basal ganglia has been suggested to be primarily involved [1,3].
As the etiology of essential blepharospasm remains unknown, treatment is mainly directed toward symptomatic improvement. Various medical therapies, including biofeedback, hypnosis, acupuncture, psychotherapy, and drugs such as clonazepam, tetrabenazine, levodopa, haloperidole, meprobamate, lithium carbonate, diphenylhydantoin, and amantadine hydrochloride, have been tried with minimal success [2]. Surgical therapies including injection of alcohol, differential sectioning of the facial nerve [4,5,6], percutaneous fractional thermolytic destruction [7], frontalis sling [8], and myectomy [9,10,11,12] have been attempted with various success rates.
Botulinum neurotoxin type A (BoNT-A) therapy is currently the most common treatment modality. There have been multiple studies published in the peer-reviewed literature that show both the efficacy and safety of this treatment [13,14,15]. Botox treatment for essential blepharospasm is clinically successful, with a low incidence of adverse events, even when treatment durations extend to 20-plus years for individuals who tolerated treatment for 15 years. The lack of any major adverse events in over 2,281 treatments with more than 23,000 injection sites is strong evidence of clinical safety [16].
The authors have found that the clinical manifestation of essential blepharospasm is variable with respect to the most-involved muscles. According to the main author's clinical experiences over 17 years, essential blepharospasm patients can be classified into three groups according to the main muscles giving rise to the spasms: the lateral orbital area (orbicularis oculi), glabella (corrugator), and ptosis (palpebral part of the orbicularis oculi) (Fig. 1).
We assessed the clinical outcomes follwing BoNT-A treatment with an individualized injection technique based on the type of spasms and compared the results of the individualized injection technique with the conventional injection technique in the same patients.
A total of 38 patients (26 female, 12 male) were treated with BoNT-A. The age range was 37 to 81 years, with a mean of 60.6 ± 10.9 years. All included patients had a confirmed diagnosis of essential blepharospasm. From November 2011 to July 2013, 77 BoNT-A injections of these 38 patients were performed by one physician at the Department of Ophthalmology, Bundang CHA Medical Center, CHA University, Seongnam, Korea. Eighteen patients had been treated with convetional BoNT-A injections before 2011, and 20 patients were referred to our hospital for unsatisfactory results after undergoing the conventional injection technique.
We classified the patients by spasm-dominant site: the lateral orbital area representing the orbital orbicularisdominant group (ODG; 44 injections, 57.1%), the glabella representing the corrugator-dominant group (CDG; 25 injections, 32.5%), and the ptosis representing the palpebral part of the orbicularis-dominant group (PDG; 8 injections, 10.4%).
Purified BoNT-A (Meditoxin; Amore Pacific, Seoul, Korea) was used, and 100 U was diluted with 2.5 mL of injectable normal saline or 50 U was diluted with 1.25 mL of injectable normal saline. This resulted in 40 U of BoNT-A in every 1 mL of normal saline. The injection dose ranged from 20 to 60 U (0.5 to 1.5 mL), with a mean of 39.6 ± 0.23 U (0.99 ± 0.22 mL) per patient.
In the 18 patients who were treated with the conventional injection technique, the mean dose was 38.0 ± 1.20 U (0.95 ± 0.30 mL). The injection pattern was modified according to the spasm-dominant site (Fig. 2). We increased the injection dose into the spasm-dominant sites of the blepharospasm groups, and additional injections were carefully performed at the center of the upper eyelid 1mm above the lid margin in the patients who suffered from ptosis in the PDG. The conventional dose average was 10.4 ± 2.4 U (0.26 ± 0.06 mL) in the orbicularis region and 9.6 ± 2.0U (0.24 ± 0.05 mL) in the glabella region. The individualized dose average was 16.4 ± 4.0 U (0.41 ± 0.10 mL) in the orbicularis region, 12.4 ± 3.2U (0.31 ± 0.08 mL) in the glabella region and 4.4 ± 0.8U (0.11 ± 0.02 mL) in the upper eyelid ( p < 0.01 in the orbicularis region and glabella region, Mann-Whitney test).
Functional disability was assessed using a questionnaire (Fig. 3) [17] that was scored from 0 (no disability) to 4 (activity impossible) for six main daily life activities: reading, watching television, domestic tasks (housework, and so forth), mobility, work, and driving. Particular attention was paid to intermediate scores. Degrees of activity were defined so patients could precisely grade their disability. The sum of the obtained scores was then related to the maximum possible total score for each patient, excluding activities not applicable to the individual patient.
We assessed subjective symptom scores after treatment according to the spasm-dominant location in all patients and compared subjective symptom scores after the conventional injection technique with those after the individualized injection technique in the 18 patients who were treated with both. The onset of treatment effect, the most comfortable time, duration of action, and complications were also assessed after injection. The results were analyzed using independent t-tests, Mann-Whitney U-tests, ANOVA, and Kruskal-Wallis tests (IBM SPSS ver. 20.0; IBM Corp., Armonk, NY, USA).
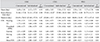
This study included 38 patients (26 women and 12 men; mean age, 60.6 ± 10.9 years; range, 37 to 81). There were 21 patients (14 female and 7 male) in ODG, 10 patients (7 female and 3 male) in CDG and 7 patients (6 female and 1 male) in the ptosis-dominant group. Mean age was 59.7 ± 12.6, 59.8 ± 8.5, and 66.8 ± 9.0 years, respectively (p = 0.44, 0.82 Kruskal-Wallis test) (Table 1).
Mean functional disability score (FDS) after injection was 1.7 ± 0.7 in the ODG, 1.4 ± 0.8 in the CDG, and 1.2±0.3 in the PDG ( p = 0.67, Kruskal-Wallis test). There were significant differences in reading and job scales among the three groups ( p = 0.02, Kruskal-Wallis test) (Table 2). There was no significant difference in any other items among the three groups. Comparing the clinical efficacy between the conventional and individualized injection techniques, there was a significant difference in reading scale among the three groups (p = 0.04, independent t-test) (Table 3). Comparing the clinical efficacy between the conventional and individualized injection techniques classified by spasm-dominant site, the success rate was 92.1% in the conventional injection group and 94.1% in the individualized injection group. There was a significant improvement in mean FDS and in reading scale in the ptosis-dominant group ( p = 0.01, 0.01, Mann-Whitney U-test) (Table 3).
Adverse events occurred in 12 of the 38 patients treated with the conventional injection technique (31.6%). The adverse effects of the injections were minor and transient. The frequent adverse effects were ecchymosis (4 patients, 10.5%), epiphora (2 patients, 5.3%), unnatural facial expression (3 patients, 7.9%), dry eyes (2 patients, 5.3%) and transient blepharoptosis (1 patient, 2.6%). No patients had major or systemic adverse effects. In the patients who were treated with the individualized injection technique, adverse events occurred in five of 17 patients (29.4%). The frequent adverse effects were ecchymosis (2 patients, 11.8%), epiphora (2 patients, 11.8%) and unnatural facial expression (1 patient, 5.9%).
Essential blepharospasm patients can be clinically classified by spasm-dominant site and the main periorbital muscle involved. Augmentation of injection dose according to the type of spasm significantly improved daily life function of the patients, especially for reading in the ptosis-dominant group. The treatment is useful in patients with secondary ptosis due to the weak levator function from longterm struggle against forceful eyelid closure [18].
A previous 14-year follow-up study reported a 43.3% incidence of adverse events. The most common adverse events were ptosis, diplopia, lid lag and epiphora [16]. Another retrospective study including 64 patients showed a first-year success rate of 93.8% [19]. In our study, there were no major adverse events, and the overall incidence of adverse events after individualized injection was less than that in the previous report. The success rate in both the conventional injection group and the individualized injection group was similar to that in other studies.
The FDS system is an easy-to-use scoring scale that is applicable to all patients and whose assessment criteria are explicit enough to restrict variability in the assessment of functional disability in patients with essential blepharospasm. Assessment takes 1 to 2 minutes and can be performed by the patient. The scale makes it possible to precisely quantify the patient's socio-professional disability at a given time [17].
This assessment scale is based on the ability to perform clearly defined tasks in daily life, thus minimizing interview subjectivity. Six criteria ensure an accurate result. Although some criteria, such as driving or working, do not apply to all patients (a frequent situation in our study's elderly population), these were excluded from the final calculation and did not affect the FDS accuracy.
We found differences in FDS after BoNT-A injection among the three groups. Even though the ptosis patients had been treated with the conventional BoNT-A injection technique, they suffered from difficulties in the activities that require intentional focusing, such as watching TV, reading and driving (Table 3). While a close-up task requires a specific narrow visual field, distance tasks require a wider visual field. Moderate improvement in eyelid opening after BoNT-A injection with the individualized technique can provide a wider visual field for reading and tasks requiring near vision. This may be why the individualized BoNT-A injection statistically improves only the reading FDS score (Table 3). It may not produce a sufficiently large effect to improve other activities requiring far vision and wider visual fields, such as driving.
As this study is retrospective, selective recall may have affected the results. For example, patients with severe disabilities may report larger differences. As an example, reading is challenging for blepharospasm patients, especially those with blepharoptosis, and so they may perceive a larger-than-actual effect after treatment. Since we used telephone interviews to collect data and the periods after treatment were variable, memory decay may have affected the results. However, FDS is the one of the most reliable evaluation tool for spasm-induced functional disabilities in essential blepharospasm patients. Another limitation of this study is the unclear treatment history of the referred patients regarding BoNT-A injection dose and injection technique. Last, there were a small number of patients in each subgroup. Further study with more patients is needed.
In conclusion, individualized injection of BoNT-A according to the spasm-dominant site is an effective and safe treatment method for essential blepharospasm patients.
Figures and Tables
Fig. 1
Classification of patients by spasm-dominant types. Circles show lateral orbital area (orbicularis oculi), diamonds show glabella (corrugator) and triangles show palpebral part of orbicularis oculi.

Fig. 2
Botulinum neurotoxin type A injection sites in the conventional injection group and the individualized injection group in blepharospasm patients. (A) Coventional injection sites of botulinum neurotoxin type A in essential blepharospasm and (B) spasm-dominant sites in essential blepharospasm.

Fig. 3
Comparison of clinical efficacy between conventional and individualized botulinum neurotoxin type A injection technique evaluated by functional disability scoring system [17]. In comparison of clinical efficacy between conventional and individualized injection technique, there was a significant difference in reading scale. FDS = functional disability score. *p < 0.05, independent t-test.

Table 2
Clinical efficacy after botulinum neurotoxin type A individualized injection according to spasm-dominant site

References
1. Henderson JW. Essential blepharospasm. Trans Am Ophthalmol Soc. 1956; 54:453–520.
2. Kim YD, Levine MR. Treatment of blepharospasm with botulinum A toxin. Korean J Ophthalmol. 1987; 1:102–108.
3. Jankovic J. Clinical features, differential diagnosis and pathogenesis of blepharospasm and cranial-cervical dystonia. Adv Ophthalmic Plast Reconstr Surg. 1985; 4:67–82.
4. Dortzbach RK. Complications in surgery for blepharospasm. Am J Ophthalmol. 1973; 75:142–147.
5. Frueh BR, Callahan A, Dortzbach RK, et al. The effects of differential section of the VIITH nerve on patients with intractable blepharospasm. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol. 1976; 81(4 Pt 1):OP595–OP602.
6. Reynolds DH, Smith JL, Walsh TJ. Differential section of the facial nerve for blepharospasm. Trans Am Acad Ophthalmol Otolaryngol. 1967; 71:656–664.
7. Battista AF. Surgical therapy for blepharospasm. Adv Neurol. 1983; 37:215–224.
8. Putterman AM, Urist M. Treatment of essential blepharospasm with a frontalis sling. Arch Ophthalmol. 1972; 88:278–281.
9. Callahan A. Blepharospasm with resection of part of orbicularis nerve supply: correction of intractable cases. Arch Ophthalmol. 1963; 70:508–511.
10. Fox SA. Relief of intractable blepharospasm: a preliminary report. Am J Ophthalmol. 1951; 34:1351–1356.
11. Fox SA. Essential (idiopathic) blepharospasm. Arch Ophthalmol. 1966; 76:318–321.
12. Gillum WN, Anderson RL. Blepharospasm surgery: an anatomical approach. Arch Ophthalmol. 1981; 99:1056–1062.
13. Albanese A, Asmus F, Bhatia KP, et al. EFNS guidelines on diagnosis and treatment of primary dystonias. Eur J Neurol. 2011; 18:5–18.
14. Colosimo C, Suppa A, Fabbrini G, et al. Craniocervical dystonia: clinical and pathophysiological features. Eur J Neurol. 2010; 17:Suppl 1. 15–21.
15. Simpson DM, Blitzer A, Brashear A, et al. Assessment: botulinum neurotoxin for the treatment of movement disorders (an evidence-based review). Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2008; 70:1699–1706.
16. Czyz CN, Burns JA, Petrie TP, et al. Long-term botulinum toxin treatment of benign essential blepharospasm, hemifacial spasm, and Meige syndrome. Am J Ophthalmol. 2013; 156:173–177.e2.
17. Grivet D, Robert PY, Thuret G, et al. Assessment of blepharospasm surgery using an improved disability scale: study of 138 patients. Ophthal Plast Reconstr Surg. 2005; 21:230–234.
18. Bodker FS, Olson JJ, Putterman AM. Acquired blepharoptosis secondary to essential blepharospasm. Ophthalmic Surg. 1993; 24:546–550.
19. Ababneh OH, Cetinkaya A, Kulwin DR. Long-term efficacy and safety of botulinum toxin A injections to treat blepharospasm and hemifacial spasm. Clin Experiment Ophthalmol. 2014; 42:254–261.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download