Abstract
Purpose
To evaluate factors associated with the direction of horizontal deviation in the sensory strabismus of patients with unilateral organic amblyopia.
Methods
The medical charts of 53 patients who had been diagnosed with sensory strabismus between 2000 and 2009 were reviewed retrospectively. The underlying ocular disease, time of onset and the duration of vision impairment, refractive error and axial length of the fixing eye, and the direction and angle of deviation were analyzed to determine the distribution of underlying diseases and any factors relevant to determining the direction of the horizontal deviation.
Results
Congenital cataracts were the most common underlying disease, found in 33 patients, followed by acquired cataracts, optic nerve disorders, retinal detachment, glaucoma and lens subluxation. Among the 50 patients with horizontal strabismus, 11 had esotropia and 39 had exotropia. The incidence of esotropia was significantly higher when the fixing eye had hyperopia or emmetropia, than when the eye was myopic. Age of onset of vision deterioration and at diagnosis of sensory strabismus, and the axial length of the fixing eye had no relationship to the direction of horizontal deviation. In addition, the duration of visual impairment had no significant relationship with the direction or extent of horizontal deviation.
Conclusions
The most common cause of sensory strabismus was congenital cataracts and the most frequent type of strabismus was exotropia. With respect to the direction of horizontal strabismus, esotropia occurred significantly more often when the refractive error of the fixing eye was hyperopia or emmetropia than when the fixing eye was myopic.
Sensory strabismus is diagnosed when unilateral or bilateral asymmetrical visual impairment, caused by anisometropic amblyopia or an organic disease, destroys fusion, and thus disrupts the eyeball array [1]. With respect to the causes of sensory strabismus, Sidikaro and von Noorden [2] reported that anisometropic amblyopia was the most common cause, followed by cataracts and corneal opacity. However, Havertape et al. [3] found the most frequent cause to be cataracts, followed by optic nerve disorder and then anisometropic amblyopia. Sensory strabismus may be horizontal, vertical or torsional. The frequencies of esotropia and exotropia in patients with horizontal strabismus are variable [2,3].
Factors relevant to the direction of deviation in sensory strabismus have been explored in many studies [1-3]. It is accepted that age of onset, the degree of loss or deterioration of vision, the interorbital distance and the refractive error of the sound eye are all important, but no consensus as to the disease etiology has yet emerged. The purpose of the present study was to evaluate factors causing sensory strabismus and to define any parameters affecting the direction of horizontal deviation.
We conducted a retrospective review of the medical charts of patients with sensory strabismus caused by unilateral organic amblyopia in which the angle of deviation had been measured between March 2000 and November 2009. Sensory strabismus was classified as either esotropia or exotropia, and we investigated any underlying diseases, the time of onset and the duration of vision impairment, the refractive power and axial length of the fixing eye, as well as the angle of deviation. Patients with vision impairment caused by strabismic amblyopia or anisometropic amblyopia were excluded; thus, only those with sensory strabismus of organic origin were included in this study. When two or more underlying diseases were present, the condition most related to the vision impairment was selected for analysis.
With respect to the refractive error, emmetropia was considered present when the spherical equivalent after cycloplegic refraction using 1% atropine or 1% cyclopentolate hydrochloride was not more than ±0.5 diopter. Thirty-seven patients were diagnosed with myopia or hyperopia. The angle of deviation was measured using the alternate prism cover test, the Hirshberg test or the Krimsky prism test, depending on the level of vision and the extent of patient cooperation.
Statistical analysis was performed using SPSS ver. 12.0 (SPSS Inc., Chicago, Il, USA). Results were analyzed with the Mann-Whitney test, the chi-squared test or Pearson's correlation. The p-value was considered significant when the value was less than 0.05. Maryknoll Hospital Committee on Ethics in Research approved the implementation of the survey protocol. The study adhered to the tenets of the Declaration of Helsinki.
A total of 53 patients, 25 females (47.2%) and 28 males (52.8%), were diagnosed with sensory strabismus, and the age at which vision impairment initially occurred ranged from birth to 44 years (mean, 6.1 years). Among the 50 patients with horizontal strabismus, 11 (22.0%) had esotropia and 39 (78.0%) had exotropia. Of the remaining three patients, one had dissociated vertical deviation (DVD) only and two had both DVD and dissociated horizontal deviation. Inferior oblique overaction (IOOA) was observed in 6 patients (11.3%), among whom one had unilateral IOOA and five had bilateral IOOA.
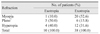
With respect to the disease underlying vision impairment, congenital cataracts were the most common, being found in 33 (62.3%) patients. Five (9.4%) patients had acquired cataracts, 4 (7.5%) an optic nerve disorder, 3 (5.7%) experienced retinal detachment, 2 (3.8%) had glaucoma and 2 (3.8%) other patients had lens subluxation (Table 1).
The age at which vision deterioration occurred was 8.3 ± 14.3 years (range, 0 to 44 years) in the esotropia group and 6.0 ± 10.5 years (range, 0 to 43 years) in the exotropia group (p = 0.710). No significant relationship was apparent between the onset age of vision impairment and the direction of eyeball deviation (p = 0.258). The age at diagnosis of sensory strabismus was 8.4 ± 13.1 years (range, 6 months to 44 years) for the esotropia group and 14.6 ± 16.5 years (range, 6 months to 44 years) for the exotropia group. Ages were not significantly different (p = 0.117).
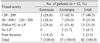
A refractive error in the fixing eye was observed in 48 patients. When the fixing eye had hyperopia or emmetropia, 9 patients had esotropia and 18 had exotropia. When the fixing eye was myopic, 1 patient had esotropia and 20 exotropia. The frequency of esotropia was significantly higher when the fixing eye had hyperopia or emmetropia than when myopia was present (p = 0.019) (Table 2). In the esotropia group, the axial length of the fixing eye was 22.2 ± 1.7 mm (range, 20.3 to 24.9 mm); in the exotropia group, the axial length was 22.3 ± 3.5 mm (range, 20.2 to 25.6 mm). Although the axial length was somewhat longer in the exotropia group, the difference was not statistically significant (p = 0.956).
With respect to the relationship between the duration of vision impairment (≤5 years vs. >5 years) and horizontal strabismus, 8 of the patients with a shorter disease duration had esotropia and 34 exotropia (esotropia : exotropia ratio = 0.24). Of patients who had a longer duration of disease, 2 had esotropia and 6 exotropia (esotropia : exotropia ratio = 0.33). The ratios were not significantly different (p = 0.653).
When the relationship between the duration of vision impairment and the degree of eyeball deviation was examined, esotropia and exotropia were 34.6 ± 20.7 prism diopters (PD) and 27.0 ± 13.9 PD, respectively, in patients with a disease duration of less than 5 years, and 50.0 ± 42.4 PD and 31.1 ± 16.8 PD, respectively, in those who had experienced disease for more than 5 years. Thus, no significant relationship was apparent between the duration of vision impairment and the degree of eyeball deviation in patients with either esotropia or exotropia (p = 0.69 and p = 0.73, respectively).
When the extent of vision in the deviated eye was measurable, there was no statistically significant difference in the direction of deviation with respect to deviated eye vision between patients with a visual acuity of 20 / 200 or below and those with a visual acuity above 20 / 200 (p = 0.397) (Table 3).
Sensory strabismus occurs when loss or deterioration of vision, arising in various ways, destroys fusion and thus, disrupts the eyeball array. Horizontal strabismus is the most common form of the condition and, in Korea, exotropia is reported to account for 75% to 85% of strabismus cases [4-6]. The frequencies of the various types of strabismus differ among ethnic groups. In Caucasians, the esotropia:exotropia ratio is 60 : 40 whereas, in Asians, the ratio is 33 : 67. This difference is thought to be due to between-race anatomical variations [7].
With respect to the cause of sensory strabismus, we found that cataracts were often to blame, being present in 71.7% of all patients, followed (in frequency) by optic nerve disorder, retinal detachment, glaucoma and lens subluxation. Sidikaro and von Noorden [2] reported that anisometropic amblyopia was the primary cause of sensory strabismus, and that cataracts and corneal opacity were less important. However, Havertape et al. [3] found that cataracts were the most frequent cause, followed by optic nerve disorders and anisometropic amblyopia.
Sidikaro and von Noorden [2] found that esotropia and exotropia occurred at similar rates when vision impairment commenced at an age of 5 years or younger, but exotropia was more common when impairment occurred after the age of 5 years. Havertape et al. [3] reported that esotropia was more common in patients suffering from a congenital loss of vision, and exotropia was more prevalent in patients whose vision loss was acquired. However, this proposed association was not statistically significant in our present work.
Many studies have explored the relationship between the refractive error of the normal eye and the direction of horizontal deviation in sensory strabismus. Von Noorden [1] found that when the refractive error of the normal eye was attributable to emmetropia or myopia, and that the eye which had lost vision showed more divergence. However, when the normal eye showed hyperopia, the eye which had lost vision displayed more convergence. Sidikaro and von Noorden [2] and Havertape et al. [3] could not find any relationship between the refractive error of the normal eye and the direction of strabismus. In the present study, fixing eyes with hyperopia or emmetropia showed a significantly greater frequency of esotropia, as compared to fixing eyes that were myopic. Although strabismus in cases of nanophthalmos, with a mean axial length of 18.4 mm (range, 15.5 to 20.7 mm), and were composed of nonaccommodative esotropia (33%), partially accommodative esotropia (27%), microesotropia (27%) and exotropia (13%), there are few studies regarding the association between the axial length and the type of the strabismus in patients with various ocular diseases [8]. In our study, in the fixing eye, the axial length was somewhat longer in the exotropia group, but the difference was not statistically significant.
A possible association between the duration of vision impairment and the extent of eyeball deviation has been studied. Yoon et al. [4] and Min et al. [9] found no significant relationship between disease duration and the extent of esotropia. However, the extent of exotropic eyeball deviation increased along with the duration of vision impairment. In the present study, when we compared patients who had experienced vision impairment for less than or equal to 5 years versus more than 5 years, no significant relationship between disease duration and either esotropia or exotropia was apparent. Similarly, Chang and Ahn [6] and Choi and Hwang [10] found that the duration of vision impairment was not significantly related to the degree of deviation.
Jampolsky [11] found that an eye with poor vision created divergence of a tonic nature, attributable to the blurred image at the macula and the peripheral retina, compared with the relatively clear image obtained by the other eye. However, the author stated that this could not explain sensory esotropia. In the present study, patients were divided into two groups: those with a deviated eye vision of 20 / 200 or lower and those with a deviated eye vision higher than 20 / 200. No statistical relationship was evident between the direction of deviation and the extent of vision in the deviated eye. Also, Sidikaro and von Noorden [2] reported that the extent of vision deterioration did not determine the direction of strabismus.
In conclusion, the most common cause of sensory strabismus in the present study was congenital cataracts and the most frequent type of strabismus was exotropia. With respect to the direction of horizontal strabismus, esotropia occurred significantly more often when the refractive error of the fixing eye was hyperopic or emmetropic, compared to when the fixing eye was myopic.
Figures and Tables
Notes
References
1. Von Noorden GK, Campos EC. Binocular vision and ocular motility: theory and management. 2002. 6th ed. St. Louis: Mosby;345–347.
2. Sidikaro Y, von Noorden GK. Observations in sensory heterotropia. J Pediatr Ophthalmol Strabismus. 1982. 19:12–19.
3. Havertape SA, Cruz OA, Chu FC. Sensory strabismus: eso or exo? J Pediatr Ophthalmol Strabismus. 2001. 38:327–330.
4. Yoon KC, You IC, Park YG. Clinical analysis of sensory strabismus. J Korean Ophthalmol Soc. 2002. 43:2483–2488.
5. Kim KS, Park SC. The clinical consideration of sensory strabismus. J Korean Ophthalmol Soc. 2005. 46:316–322.
6. Chang KC, Ahn M. Clinical observations in sensory heterotropia. J Korean Ophthalmol Soc. 2003. 44:1578–1583.
7. Ing MR, Pang SW. The racial distribution of strabismus. Proceedings of the 3rd meeting of the International Strabismological Association; 1978. 1978. New York: Grune & Stratton;107–110.
8. Sener EC, Mocan MC, Sarac OI, et al. Management of strabismus in nanophthalmic patients: a long-term follow-up report. Ophthalmology. 2003. 110:1230–1236.
9. Min BM, Min WK, Lee KM, Kim YB. Clinical evaluation of sensory heterotropia. J Korean Ophthalmol Soc. 1989. 30:767–772.
10. Choi MY, Hwang JM. Clinical analysis of sensory strabismus with organic amblyopia in children. J Korean Ophthalmol Soc. 2005. 46:1374–1381.
11. Jampolsky A. Ocular divergence mechanisms. Trans Am Ophthalmol Soc. 1970. 68:730–822.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download