Abstract
Methods
A retrospective chart review was performed on patients with ON between January 2000 and December 2009. We obtained the best-corrected visual acuity (BCVA), Goldmann perimetry, relative afferent pupillary defect (RAPD), and color function tests as well as brain magnetic resonance imaging (MRI) findings in patients who were in the acute stage of the disorder.
Results
Nine eyes in eight patients were included. The mean age of patients at presentation was 60.5 years (range, 53 to 71 years). Six patients were female, and two were male. There was one patient with bilateral ON. The mean BCVA at presentation was 20 / 400 (no light perception-20 / 70). Eight eyes (89%) complained of pain with eye movement. Six eyes (66%) had disc edema. Central scotoma was the most common field defect. All eyes had color abnormalities. Five eyes in four patients showed abnormalities of the involved optic nerves on MRI. The patients were followed for a mean of 11.3 months (range, 2 to 34 months). All of the patients recovered to a BCVA of 20 / 40 or better within 2 months. On the last follow-up, the mean BCVA was 20 / 20 (20 / 40 to 20 / 16). Four eyes showed remnant central scotoma. One eye had remnant RAPD, and two eyes had mild color abnormalities.
Optic neuritis (ON) is an acute inflammatory condition affecting the optic nerve. The most common cause of ON is demyelination of the optic nerve (either idiopathic or due to multiple sclerosis), although there are other possible etiologies, including para-infectious responses, infections and vasculitides. ON typically affects young adults between 18 and 45 years of age, with a mean age of 30 to 35 years; there is a strong female predominance [1]. In the Optic Neuritis Treatment Trial (ONTT), the mean patient age was 31.8 years, and 77% of participants were female [2].
Idiopathic ON and non-arteritic anterior ischemic optic neuropathy (NAION) are acute optic neuropathies with overlapping clinical profiles. ON typically presents as painful loss of vision in younger patients and has good potential for improvement, whereas NAION typically presents as painless loss of vision in the middle-aged or elderly with usually less complete recovery. Although there has been some effort to differentiate ON and NAION using visual field testing [3], magnetic resonance imaging (MRI) [4], pattern electroretinography [5], or optic disc morphology [6], there is no gold standard for distinguishing ON from NAION.
Especially in the elderly, ON is uncommon and is often misdiagnosed as NAION. Although we occasionally encounter elderly patients with ON in the clinic, few reports that document ON in elderly patients have been published. Therefore, in this report, we described the clinical course and characteristics of ON in elderly patients.
This study was a retrospective case series. We reviewed the medical records of patients who attended the Neuro-ophthalmic Clinic in the Department of Ophthalmology at Seoul National University Hospital and were diagnosed with ON between January 2000 and December 2009. The study protocol followed the tenets of the Declaration of Helsinki. Informed consent was obtained, and the Institutional Review Board of Seoul National University Hospital Clinical Research Institute approved the study.
We searched for patients who were diagnosed with ON or NAION and who were also >50 years of age at the time of initial presentation. Patients who were finally diagnosed with ON by an experienced neuro-ophthalmologist (SJK) were included in this study. The patient age at onset, gender, medical history, duration from the onset of visual symptoms, and presence of ocular pain on eye movement were noted. Determination of the best-corrected visual acuity (BCVA) and the presence of a relative afferent pupillary defect (RAPD), and visual field testing, color function testing, and fundoscopy were performed at the initial presentation and on each follow-up visit. Patients who underwent any treatment before the visit to our clinic and who had a previous visual loss history or other ocular abnormalities causing visual loss were excluded. Whether or not the patients received treatment for ON was also ascertained.
The diagnosis of ON was made on the basis of clinical symptoms, such as ocular pain or gradual visual loss over several days, signs of abnormal optic nerve thickening or enhancement on MRI with contrast, and the clinical course of subsequent visual recovery. To distinguish ON from NAION, fluorescene angiography (FAG) was also performed, and disc non-perfusion was ruled out.
We examined RAPD by performing the swinging flashlight test and identified color abnormalities by testing participants using the Hardy-Rand-Rittler (HRR) color plate. Color abnormalities were graded as normal color function, and mild, moderate or severe defects. Visual fields were examined with the Goldmann perimeter (GVF) by experienced technicians. The mean BCVAs were calculated after conversion to a logarithm of the minimal angle of resolution (logMAR). Visual acuity of the counting fingers was converted to 2 in logMAR, and hand movement to 3 in logMAR. However, light perception or no light perception were not actually visual measurements, so therefore these parameters were excluded from our calculations [7].
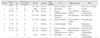
Nine eyes of eight patients were included in our study. Patient demographics and initial examination results are listed in Table 1. The mean age of the patients was 60.5 years (range, 53 to 71 years). Six patients were female, and two patients were male. One patient had bilateral ON. Five right eyes and four left eyes were involved. One patient had diabetes, and another patient had hyperthyroidism.
At the time of the initial examination, eight eyes (89%) were accompanied by pain on eye movement. The mean BCVA was 20 / 400 (range, no light perception-20 / 70). Six eyes (66%) had disc swelling, whereas three eyes had a normal disc appearance. Unaffected fellow eyes had normal disc appearances with normal cup-disc ratios. In patients with unilateral ON, all affected eyes had RAPD, and in the patient with bilateral ON, the more severely affected eye had RAPD. GVF revealed four eyes with central scotomas, two eyes with altitudinal defects, and one eye with generalized decrease of perception. Two eyes could not perform the field test due to poor vision. Four eyes failed to distinguish figures on all the plates during the HRR color function test, and three eyes had severe color function defects. Two eyes did not undergo the color test at the time of the initial examination. Five patients had MRI, and five eyes of four patients had abnormalities (such as optic nerve swelling or enhancement of the involved optic nerve) noted on MRI, but no participants showed abnormal brain enhancement (Table 1). The duration from the onset of decreased vision to the time of lowest visual acuity was 9.3 days (range, 5 to 14 days).
Among eight patients, three were treated with intravenous, high-dose corticosteroid therapy and three received oral corticosteroid therapy. Two of the three patients who received oral steroids were misdiagnosed with NAION initially, and the other patient was treated at a primary ophthalmic clinic before referral to our clinic. Oral steroids were tapered in our clinic, and intravenous, high-dose corticosteroid therapy was not administered due to the request of the patient. The other two patients refused to receive intravenous high-dose corticosteroid therapy. Three patients who received intravenous steroids showed no side effects.
Two patients (cases 3 and 7) was misdiagnosed as NAION initially because they were elderly, had systemic illness such as diabetes mellitus or hypertension, and had disc swelling with relatively abrupt visual impairment, which are all more common in NAION. They also complained of less specific eye pain on eye movement. One patient (case 3) had an altitudinal defect on GVF. However, no participants showed abnormal disc perfusion on FAG. One participant (case 3) demonstrated optic nerve enhancement on MRI, and both showed visual improvement during follow-up, which led to a final diagnosis of optic neuritis.
The patients were followed for a mean of 11.3 months (range, 2 to 34 months), and all recovered to a BCVA of 20 / 40 or better within 2 months. Eight eyes gained complete visual recovery, and one eye achieved partial recovery. At the last follow-up, the mean BCVA was 20 / 20 (20 / 40 to 20 / 16). Three eyes had remnant, small central scotomas, and one eye had a small paracentral scotoma. RAPD remained in one eye, and mild color abnormalities were present in two eyes. Disc pallor was observed in five eyes (Table 2).
This is the first report involving ON in patients >50 years of age. Based on our results, ON in elderly patients is uncommon; there were only eight patients who visited our clinic between January 2000 and December 2009 who were diagnosed with ON. The diagnosis of ON was based strictly on clinical judgment considering the neuro-ophthalmic history and examination (fundoscopy, visual field testing, color testing, and MRI). The clinical course of visual impairment was also considered in the final diagnosis of ON because ON (but not NAION) is typically associated with substantial visual recovery [8]. In this study, all affected eyes recovered visual acuity better than 20 / 40 within two months. This clearly demonstrates that ON had a good visual prognosis, even in patients >50 years of age.
Nevertheless, there is no gold standard for the diagnosis of ON. Rizzo and Lessell [9] reported that ON and NAION have many overlapping clinical profiles, and it may be difficult to differentiate between ON and NAION solely on nosologic grounds in some instances of acute, unilateral optic neuropathies. From previous reports [1,3-6], some distinguishing characteristics between ON and NAION are known, as follows: ON occurs in young patients, whereas NAION occurs in elderly patients; ON has a normal-color disc edema without hemorrhage in the acute stage and culminates with temporal pallor, whereas NAION has altitudinal or pale disc edema with hemorrhage and retinal arterial attenuation in the acute stage and persistent segmental or altitudinal optic atrophy [6]; most ON patients who receive gadolinium have abnormal signal intensity on MRI, whereas few NAION patients show abnormalities [4]; and ON has characteristic central scotoma on the fixation point with a sloping border, whereas NAION has an inferior altitudinal defect with a sharp border along the horizontal meridian [3]. Despite all of these differences, the diagnosis of ON in some instances is still a matter of debate. In our study, the two patients who received oral steroids were initially misdiagnosed with NAION and prescribed oral steroids. After obtaining a detailed history and undergoing GVF, MRI and follow-up examinations, they were re-diagnosed with ON.
The diagnosis of ON in our cases was made according to the initial presenting features, including pain on eye movement, gradual visual impairment over several days, optic nerve abnormalities on MRI during the acute stage, the pattern of visual field defect on initial examination and follow-up, and visual recovery. Eight of nine eyes experienced pain on eye movement preceding visual impairment in our study, whereas 92% of patients enrolled in the ONTT reported pain [2]. With respect to disc swelling, greater than one-half of the eyes had disc swelling, and one-third of ONTT patients had disc swelling [2]. The discrepancy in the percentages of pain and disc swelling between our study and the ONTT may be attributed to the small number of cases or the different age distribution; further evaluation is necessary.
MRI was performed in only five patients, including one patient with bilateral ON; abnormal findings, such as swelling or enhancement of the optic nerve, were demonstrated on MRI in five eyes of four patients. No patient had abnormal brain lesions on MRI. Considering the relationship between ON and multiple sclerosis, the small number of cases in our study made it difficult to evaluate the prevalence of multiple sclerosis in elderly patients. However, the high incidence of optic nerve abnormalities on MRI in this study suggested that MRI was important in the diagnosis of ON, which is in agreement with the findings of Rizzo et al. [4].
Central scotoma is the characteristic feature of the visual field in ON [3]. In this study, four eyes had central scotoma at the time of the initial examination, and two eyes showed central scotoma during follow-up. The latter two eyes had very poor visual detection of hand movements and failed to perform GVF initially. Two eyes that showed initial altitudinal defects, which is more common in NAION [3] but also can be seen in ON [1-3,10], recovered completely at the time of final examination, whereas visual field defects in NAION rarely recover. Therefore, follow-up visual field tests may aid in the diagnosis of ON.
Elderly patients are prone to decline intravenous, high-dose corticosteroid therapy when offered due to the known side effects, such as sleep disturbances, mood changes, gastric disturbances, facial flushing, weight gain during the treatment period, and infections [11]. Subsequently, the overall treatment rate appears to be lower than that occurring in pediatric or young adult patients. There is also a substantial tendency for multiple sclerosis to develop in patients with ON [12,13], and the intravenous administration of high-dose corticosteroids may lessen the risk of progression to multiple sclerosis within two years of an acute attack of ON [14]. The low rate of intravenous high-dose corticosteroid treatment and age >50 years in this study might have influenced the later development of multiple sclerosis. However, the mean follow-up period for our patients was only 11.3 months, and the prevalence of multiple sclerosis is also much lower in Asian countries compared with the Western population [15]. Therefore, we could not further evaluate this hypothesis regarding ON and multiple sclerosis.
The three patients who received intravenous, high-dose corticosteroid therapy initially had more severely impaired visual acuity than counting fingers. Despite steroid therapy, which is known to induce early visual recovery [16], it took >1 month to acquire a visual acuity of 20 / 40 or better, and remnant, tiny central scotomas existed on the final examination in two of these patients. Based on these findings, the effect of intravenous steroid therapy in elderly patients must be further evaluated.
This study had some limitations. First, this was a retrospective study; the number of patients was small because ON is uncommon in elderly patients. Second, the follow-up period of patients was too short to evaluate their long-term prognosis. The favorable visual outcome of ON prohibits patients from returning to the clinic. The two patients who were followed for only two months did not visit our clinic after their visual acuity recovered. A comparison of clinical characteristics with ON in young adults or in patients with NAION may be necessary. Some patients in this study were diagnosed with ON because they showed substantial visual recovery during follow-up, so the conclusion that elderly patients with ON have a good prognosis may be biased. Moreover, visual function testing (including contrast sensitivity or Humprey visual field testing) or evaluation of the fellow eye may help to understand ON in elderly patients. However, we believe that this study is worthy to report because this is the first trial to investigate ON in patients >50 years of age, which is contrary to the general perception that ON occurs between the ages of 20 and 50 years, with a peak between 30 and 35 years of age.
In summary, we have shown that ON can develop in elderly patients, and the clinical features of ON in elderly patients do not differ from the clinical features in young patients. Careful diagnostic approaches are essential for the differential diagnosis of acute optic neuropathies in elderly patients. Further evaluations regarding treatment modalities for ON and their effect in elderly patients will be necessary. Although the pathogenesis of ON in elderly patients may differ from ON in young patients, we could not identify any basis by which to determine the differences.
References
1. Walsh FB, Hoyt WF, Miller NR. Walsh and Hoyt's clinical neuro-ophthalmology. 1982. Vol. 1:4th ed. Baltimore: Williams & Wilkins.
2. Optic Neuritis Study Group. The clinical profile of optic neuritis. Experience of the optic neuritis treatment trial. Arch Ophthalmol. 1991. 109:1673–1678.
3. Gerling J, Meyer JH, Kommerell G. Visual field defects in optic neuritis and anterior ischemic optic neuropathy: distinctive features. Graefes Arch Clin Exp Ophthalmol. 1998. 236:188–192.
4. Rizzo JF 3rd, Andreoli CM, Rabinov JD. Use of magnetic resonance imaging to differentiate optic neuritis and non-arteritic anterior ischemic optic neuropathy. Ophthalmology. 2002. 109:1679–1684.
5. Froehlich J, Kaufman DI. Use of pattern electroretinography to differentiate acute optic neuritis from acute anterior ischemic optic neuropathy. Electroencephalogr Clin Neurophysiol. 1994. 92:480–486.
6. Rath EZ, Rehany U, Linn S, Rumelt S. Correlation between optic disc atrophy and aetiology: anterior ischaemic optic neuropathy vs optic neuritis. Eye (Lond). 2003. 17:1019–1024.
7. Holladay JT. Proper method for calculating average visual acuity. J Refract Surg. 1997. 13:388–391.
8. Beck RW, Cleary PA, Backlund JC. The course of visual recovery after optic neuritis. Experience of the optic neuritis treatment trial. Ophthalmology. 1994. 101:1771–1778.
9. Rizzo JF 3rd, Lessell S. Optic neuritis and ischemic optic neuropathy. Overlapping clinical profiles. Arch Ophthalmol. 1991. 109:1668–1672.
10. Nevalainen J, Krapp E, Paetzold J, et al. Visual field defects in acute optic neuritis: distribution of different types of defect pattern, assessed with threshold-related supraliminal perimetry, ensuring high spatial resolution. Graefes Arch Clin Exp Ophthalmol. 2008. 246:599–607.
11. Chrousos GA, Kattah JC, Beck RW, Cleary PA. Side effects of glucocorticoid treatment. Experience of the optic neuritis treatment trial. JAMA. 1993. 269:2110–2112.
12. Rizzo JF 3rd, Lessell S. Risk of developing multiple sclerosis after uncomplicated optic neuritis: a long-term prospective study. Neurology. 1988. 38:185–190.
13. Beck RW, Cleary PA, Anderson MM Jr, et al. The Optic Neuritis Study Group. A randomized, controlled trial of corticosteroids in the treatment of acute optic neuritis. N Engl J Med. 1992. 326:581–588.
14. Beck RW, Cleary PA, Trobe JD, et al. The Optic Neuritis Study Group. The effect of corticosteroids for acute optic neuritis on the subsequent development of multiple sclerosis. N Engl J Med. 1993. 329:1764–1769.
15. Alter M, Good J, Okihiro M. Optic neuritis in Orientals and Caucasians. Neurology. 1973. 23:631–639.
16. Beck RW, Trobe JD. What we have learned from the Optic Neuritis Treatment Trial. Ophthalmology. 1995. 102:1504–1508.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download