Abstract
A 68-year-old male patient presented with a week of sudden diplopia. He had been diagnosed with nasopharyngeal cancer 8 months prior and had undergone chemotherapy with radiotherapy. Eight-prism diopter right esotropia in the primary position and a remarkable limitation in abduction in his right eye were observed. Other pupillary disorders and lid drooping were not found. After three weeks, the marginal reflex distance 1 was 3 mm in the right eye and 5 mm in the left eye. The pupil diameter was 2.5 mm in the right eye, and 3 mm in the left eye under room illumination. Under darkened conditions, the pupil diameter was 3.5 mm in the right eye, and 5 mm in the left eye. After topical application of 0.5% apraclonidine, improvement in the right ptosis and reversal pupillary dilatation were observed. On brain magnetic resonance imaging, enhanced lesions on the right cavernous sinus, both sphenoidal sinuses, and skull base suggested the invasion of nasopharyngeal cancer. Lesions on the cavernous sinus need to be considered in cases of abducens nerve palsy and ipsilateral Horner's syndrome.
The cavernous sinus is a structure located near the center of the skull base, that is situated bilaterally on the medial side of both sphenoid sinuses [1,2]. It contains the oculomotor, trochlear, abducens, and the first two divisions of the trigerminal nerve as well as the oculosympathetic nerve plexus around the internal carotid artery [3-6]. These anatomical particularities are causes of solitary or combined diverse impairments of cranial nerves and postganglionic Horner's syndrome [1,3,4,7]. Tumour involvement of the cavernous sinus region due to distant metastasis or local extension has been reported in <1% of cancer patients [3,7]. Furthermore, the brain is a rarely involved site with head and neck cancers [3,8,9]. Nasopharyngeal carcinoma can spread through the foramen lacerum and invade the cavernous sinus, resulting in cranial nerve injuries [7]. In previous reports, there have been only 13 cases of combined abducens nerve palsy and ipsilateral Horner's syndrome secondary to metastatic neoplasm within the cavernous sinus [4,10-16]. Here, we report a case with a combination of 6th nerve palsy and incomplete Horner's syndrome caused by invasive nasopharyngeal cancer in the cavernous sinus.
We examined a 68-year-old man who had been suffering from diplopia for a week. The patient had been diagnosed with a nasopharyngeal squamous cell carcinoma 8 months prior and had received cisplantin-based chemotherapy with radiotherapy. On the first examination, 8-prism diopter right esotropia in the primary position and a remarkable limitation in abduction in his right eye were observed. Other pupillary disorders and lid drooping were not found (Fig. 1). After 3 weeks, the patient complained of lid drooping in the right eye. The marginal reflex distance 1 (MRD1) was 3 mm in the right eye and 5 mm in the left. In addition to right mild ptosis, anisocoric pupils with a smaller right pupil were found and the anisocoria increased in the dark. After topical application of 0.5% apraclonidine (Iopidine; Alcon, Fort Worth, TX, USA), the patient's right pupil dilated from 2.5 mm to 5 mm in bright light and the right MRD1 increased from 3 mm to 5 mm (Fig. 2). Hypohydrosis and other neurologic abnormalities were not observed. Brain magnetic resonance imaging (MRI) revealed newly appeared gadolinium-enhanced mucosal thickening in both sphenoid sinuses combined with bony destruction of the skull base. These lesions extended to the right cavernous sinus with encasement of the internal carotid artery (ICA) (Fig. 3). The patient underwent bilateral functional endoscopic sinus surgery with biopsy. Pathology was consistent with poorly differentiated invasive squamous cell carcinoma (Fig. 4). Seven weeks later, the esotropia worsened and the limitation of abduction, anisocoria, and right ptosis persisted. No other neurologic abnormalities were found up to the last visit. The patient died of cancerous cachexia 15 months after the diagnosis of nasopharyngeal cancer.
Neither abducens nerve palsy nor Horner's syndrome provides an indication of the location of the lesion. However, when both are present, it is important to localize the site of the lesion [16]. When these rare clinical features are manifested, we have to consider paratrigerminal syndrome or a lesion of the posterior cavernous sinus [1]. Sympathetic nerve fibers travel over the wall of the carotid artery and in the cavernous portion the fibers leave the ICA and accompany the abducens nerve for only a few millimeters in the posterior portion of the sinus [4,10,12,16] (Fig. 5). Therefore, we could consider a posterior cavernous sinus lesion due to combined abducens nerve palsy. Furthermore, incomplete Horner's syndrome without anhydrosis, as in the case reported here, indicates the involvement of the periarterial sympathetic plexus at the third angulation point [17]. To date, only 13 cases with this combination of symptoms secondary to metastatic neoplasm within the cavernous sinus have been reported [4,10-16]. Regarding the primary lesions in these cases, there were 1 small cell lung cancer [10], 1 parotid cancer [10,12], 1 breast cancer [11], 1 gastric cancer [10], 1 uterine cancer [4], 3 undetermined origins [13,14] and 3 nasopharyngeal cancers [15]. Unlike in other three nasopharyngeal cancer cases reported by Hirao et al. [15], the cancer only invaded the 6th nerve and sympathetic fiber without involvement of the 5th nerve in this case. Malignant tumors that affect the cavernous sinus commonly result in the 5th and the 6th nerve injuries [3,8]. The more medial location of the abducens nerve has been postulated as the reason for its frequent involvement when confronted with the compressive forces in a confined space or direct invasion [8]. In this case, the nasopharyngeal cancer extended through the sphenoidal sinus demonstrated by brain MRI and positron emission tomography (Fig. 3). Therefore, the cancer affected only the 6th nerve without involvement the 3rd nerve, which occupies a superior position at the lateral wall of the sinus, in addition to the 4th and 5th nerve [1]. Although autopsy was not permitted and there was a limitation of anatomical access, we suggest that tumor cells in the sphenoidal sinus had spread to the 6th nerve in the cavernous sinus, and then perineurally metastasized to the oculosympathetic nerve fibers before joining the first division of the 5th nerve [3]. A plausible alternative to cocaine or hydroxyamphetamine in the diagnosis of Horner's syndrome is apraclonidine, a direct α-receptor agonist with strong α2 and weak α1 activity [18]. In patients with Horner's syndrome, reversal of anisocoria and improvement of ptosis occur after application of apraclonidine due to denervation supersensitivity of the α1 receptor [18]. With respect to the length of survival in patients with tumor invasion of the cavernous sinus region as reported in the literature, most individuals live no longer than six months and the ultimate outcome is a dismal 75% to 85% expected mortality within 2 years [3,8]. The patient described in this report died 5 months after the presentation of combination abducens nerve palsy with Horner's syndrome. In other words, this manifestation may be a significant predictor of survival in addition to the location of the lesion. This is the first reported case of abducens nerve palsy with Horner's syndrome due to tumor invasion into the cavernous sinus in a Korean patient. The presence of Horner's syndrome and the 6th nerve palsy should be cautiously investigated to confirm the existence of the cavernous sinus lesions.
Figures and Tables
Fig. 1
Ocular movements. Right esotropia and limitation of abduction in the right eye consistent with right abducens nerve palsy were observed.

Fig. 2
(A1,B1) Before topical application of 0.5% apraclonidine in room light. Pupil right eye (OD) measured 2.5 mm (A1), pupil left eye (OS) measured 3.0 mm (B1). (A2,B2) After topical application of 0.5% apraclonidine in bright light. Pupil OD measures 5.0 mm (A2), pupil OS measured 4.0 mm (B2). Reversal of pupillary dilatation under topical application of 0.5% apraclonidine was detected. (C1,C2) Note also the improvement of the mild ptosis in the right side after topical application of 0.5% apraclonidine.

Fig. 3
Axial T1-weighted contrast-enhanced magnetic resonance images. Ill-defined right cavernous sinus lesion extending into the sphenoidal sinus and encasement of the internal carotid were found.
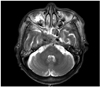
Fig. 4
A photomicrograph of the frozen biopsy during the functional endoscopic sinus surgery showing the moderately to poorly differentiated squamous cells in the right sphenoid sinus (H&E, ×200).
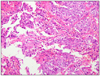
Fig. 5
Schematic drawing demonstrating the anatomy of the posterior portion of the cavernous sinus on the right side. Oculosympathetic nerve fibers leave the internal carotid artery, and then join the abducens nerve for a short distance in the posterior portion of the cavernous sinus (arrow). CN III = oculomotor nerve; CN IV = trochlear nerve; CN V = trigeminal nerve; ICA = internal carotid; CN VI = abducens nerve; Sym = oculosympathetic nerve.

Notes
References
1. Silva MN, Saeki N, Hirai S, Yamaura A. Unusual cranial nerve palsy caused by cavernous sinus aneurysms. Clinical and anatomical considerations reviewed. Surg Neurol. 1999. 52:143–148.
2. Rhoton AL Jr. The cavernous sinus, the cavernous venous plexus, and the carotid collar. Neurosurgery. 2002. 51:4 Suppl. S375–S410.
3. Ampil FL, Heldmann M, Ibrahim AM, Balfour EL. Involvement of the cavernous sinus by malignant (extracranial) tumour: palliation in six cases without surgery. J Craniomaxillofac Surg. 2000. 28:161–164.
4. Tsuda H, Yorinaga Y, Tamada Y, et al. Combination of abducens nerve palsy and ipsilateral postganglionic Horner syndrome as an initial manifestation of uterine cervical cancer. Intern Med. 2009. 48:1457–1460.
5. George A, Haydar AA, Adams WM. Imaging of Horner's syndrome. Clin Radiol. 2008. 63:499–505.
6. Parkinson D. Bernard, Mitchell, Horner syndrome and others? Surg Neurol. 1979. 11:221–223.
7. Kano H, Niranjan A, Kondziolka D, et al. The role of palliative radiosurgery when cancer invades the cavernous sinus. Int J Radiat Oncol Biol Phys. 2009. 73:709–715.
8. Curry MP, Newlon JL, Watson DW. Cavernous sinus metastasis from laryngeal squamous cell carcinoma. Otolaryngol Head Neck Surg. 2001. 125:567–568.
9. Djalilian HR, Tekin M, Hall WA, Adams GL. Metastatic head and neck squamous cell carcinoma to the brain. Auris Nasus Larynx. 2002. 29:47–54.
10. Tsuda H, Ishikawa H, Kishiro M, et al. Abducens nerve palsy and postganglionic Horner syndrome with or without severe headache. Intern Med. 2006. 45:851–855.
11. Gutman I, Levartovski S, Goldhammer Y, et al. Sixth nerve palsy and unilateral Horner's syndrome. Ophthalmology. 1986. 93:913–916.
12. Tsuda H, Ishikawa H, Asayama K, et al. Abducens nerve palsy and Horner syndrome due to metastatic tumor in the cavernous sinus. Intern Med. 2005. 44:644–646.
13. Slamovits TL, Cahill KV, Sibony PA, et al. Orbital fine-needle aspiration biopsy in patients with cavernous sinus syndrome. J Neurosurg. 1983. 59:1037–1042.
14. Wilhelm H, Ochsner H, Kopycziok E, et al. Horner's syndrome: a retrospective analysis of 90 cases and recommendations for clinical handling. Ger J Ophthalmol. 1992. 1:96–102.
15. Hirao M, Oku H, Sugasawa J, et al. Three cases of abducens nerve palsy accompanied by Horner syndrome. Nihon Ganka Gakkai Zasshi. 2006. 110:520–524.
16. Kurihara T. Abducens nerve palsy and ipsilateral incomplete Horner syndrome: a significant sign of locating the lesion in the posterior cavernous sinus. Intern Med. 2006. 45:993–994.
17. Ozveren MF, Uchida K, Erol FS, et al. Isolated abducens nerve paresis associated with incomplete Horner's syndrome caused by petrous apex fracture: case report and anatomical study. Neurol Med Chir (Tokyo). 2001. 41:494–498.
18. Freedman KA, Brown SM. Topical apraclonidine in the diagnosis of suspected Horner syndrome. J Neuroophthalmol. 2005. 25:83–85.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download