Abstract
Purpose
To determine methods tried in clinical trials to reduce the progression of myopia in children, and spectacle prescribing patterns of hospital ophthalmologists.
Methods
A multi-sectioned survey composed of Likert items relating to the methods of reducing myopia progression (orthokeratology lenses [O-K lenses], undercorrected glasses, and topical atropine) and the patterns of prescribing spectacles for children (including two cases involving a 5-year-old girl and an 8-year-old boy) were distributed to members of the Korean Ophthalmological Society, and the collected data was statistically analyzed.
Results
A total of 78 out of 130 ophthalmologists returned the survey. On a scale of 1 to 5, the mean rates of whether the ophthalmologists think O-K lenses arrest myopia progression, and whether they recommend their patients to wear O-K lenses if indicative, were 3.06 and 2.75, respectively. Moreover, the mean rates of whether they consider that wearing glasses which are undercorrected would slow down the progression of the myopia, or if they think topical atropine helps in arresting myopia progression in children, were 2.34 and 1.27, respectively. In response to the case studies, the majority of practitioners preferred to prescribe the full amount found in cycloplegic refraction to pediatric patients with myopia.
Conclusions
Ophthalmologists in clinical practice encouraged children to wear O-K lenses more than undercorrected glasses as a way to retard myopia progression. However, the application of atropine is rarely tried in clinical trials. In managing pediatric patients with myopia (case specific), the majority of the practitioners chose to prescribe glasses with full cycloplegic correction.
Myopia, known to be the most common refractive error and childhood ocular disease in Asia, is a physiological process that the eye uses to adapt to the excessive near focal surroundings, which is easily correctable with optical devices [1]. Yet, the health risk associated with myopia should not be underestimated since the economic impact of routine optometry visits, contact lenses, spectacles, and refractive surgeries on the myopic population is considerable [1,2].
The onset age of myopia that is frequently mentioned is between 5 and 15 years, and a number of studies have been conducted to depict the prevalence rate of myopia worldwide. The etiology, pathogenesis, and treatment of myopia have also been debated over a long period of time in ophthalmic countries [3,4]. Studies and statistics for myopia by country have shown that both the incidence and progression rates of myopia are high in Asian children [3,4]. There had been epidemiological evidence that children who spend more time outside are protected from the development of myopia than those who spend more time doing near-work [5]. Moreover, methodological means to correct myopic refractive errors such as orthokeratology and the use of atropine have been reviewed intensively in East Asia [6-10]. In this study, a survey of Korean Ophthalmological Society members was conducted in order to evaluate the opinions of practitioners about some of the treatment modalities used to reduce myopia progression in children, as well as spectacle prescribing patterns for preschool children with myopia (2 cases).
A questionnaire was distributed to the members of the Korean Ophthalmological Society working in hospitals or private clinics in South Korea. Questionnaires completed by the respondents were collected at the 2009 Annual Symposium. The questionnaire was composed of two sections (one with multiple questions and another with two case specific questions). In the first section, respondents were asked to rate according to the Likert scale (from 1 to 5) on three statements about whether they think orthokeratology lenses (O-K lenses), undercorrected glasses, or the use of topical atropine reduces myopia progression in children (statement 1,3, and 4), in addition to one statement about whether they would recommend O-K lenses to their pediatric patients with myopia (statement 2). On a scale from 1 to 5, a response of 5 was considered as 'strongly agree with the statement,' and 1 was considered as 'strongly disagree with the statement.' In the second section, the respondents were asked about the patterns of prescribing glasses to their hypothetical pediatric patients; there were 2 case specific questions relating to a 5-year-old girl and an 8-year-old boy with detailed information including the child's age, distance vision, distance cover test (DCT) and near cover test (NCT), manifest refraction, and cycloplegic refraction (case 1 and case 2, Fig. 1). Respondents were asked to indicate whether spectacles should be prescribed, and whether this would be a full or partial correction. The collected data was statistically analyzed.
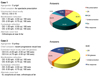
Seventy-eight ophthalmologists responded (56%) out of 130 who had consented to fill out the questionnaire. Responses to the four Likert scale items were analyzed. The majority of ophthalmologists practicing in Korea were neutral about the idea of the effects that O-K lenses have on reducing myopia progression. 16.7% (13 / 78) of the respondents strongly disagreed with statement 1, and did not recommend that their pediatric patients with myopia wear O-K lenses if indicative. Only 6.4% (5 / 78) strongly agreed with statement 1, and the majority of the physicians chose to be neutral-to-negative about prescribing O-K lenses to children with myopia (Fig. 2). The mean rates in which the ophthalmologists thought that O-K lenses arrest myopia progression, and whether they would recommend that their patients wear O-K lenses if indicative, were 3.06 and 2.75, respectively.
Of the respondents, 32% (25 / 78) strongly disagreed that optical undercorrection slows down the progression of myopia (statement 3), and the majority of ophthalmologists were negative about children with myopia wearing glasses that are undercorrected as a way to reduce myopia progression (Fig. 2).
The mean rates corresponding to whether they consider that wearing undercorrected glasses would slow down the progression of the myopia, and whether using topical atropine could help arrest myopia progression, were 2.34 and 1.27, respectively. 79.5% (62 / 78) of the respondents strongly disagreed with statement 4. The majority of the ophthalmologists who responded reacted negatively to the idea of using topical atropine to retard myopia progression in children with myopia (Fig. 2).
Two case records detailed myopic children, with one about a five year old girl, and the other about an eight year old boy. For case 1, spectacles were prescribed with full correction according to the cycloplegic refraction by 28.2% of respondents, and full correction according to the post-cycloplegic refraction by 24.4% (Fig. 1). For case 2, spectacles were prescribed with full correction according to the cycloplegic refraction by 43.6% of practitioners, a reduced correction both cylindrically and spherically by 20.5% (Fig. 1).
A number of previous studies have evaluated the efficacy of several interventions to reduce the progression of myopia. It is also well recognized in prescribing practices that uncorrected refractive error during childhood can result in the development of amblyopia and strabismus [11]. Some of the methodological means used to retard the progression of myopia include bifocal and multifocal lenses, contact lenses, orthokeratology lenses, atropine, pirenzipine, and tropicamide eye drops and ocular hypotensives [12-14]. However, there is no guideline produced by professional bodies to treat pediatric patients with myopia in Korea, and large-scaled randomized clinical trials are necessary to evaluate the efficacy of such treatment.
The results of the present study suggest that Korean ophthalmologists are not well convinced by some of the methods used to reduce myopia progression which are conveniently applicable in clinical trials. The ophthalmologists that participated in this study were neutral about the effect of corneal flattening on myopia reduction using orthokeratology lenses. Moreover, the majority of the participants reacted negatively to prescribing O-K lenses to children with myopia. Orthokeratology has been practiced for decades, yet since its use of a temporary alteration of the corneal shape does not correct the intrinsic cause of myopia and since it is associated with potential complications such as infective keratitis, its use in children is still controversial [15,16]. Although few studies have investigated the effect of undercorrection to slow down the progression of early-onset myopia, it had recently reported that undercorrection exhibited no beneficial effect on its reduction, and the response for prescribing undercorrected glasses was in broad agreement of such report [11,17]. Some of the theories associated with the effects of topical atropine in arresting myopia progression were that it blocks accommodation and reduces the possible effects of excessive accommodation on myopia progression [9,10,18]. For preschool children, not yet old enough to conduct near work on their own, with nearly symmetrical myopia less than -3.00 diopter (D), more than 50% of the respondents chose to prescribe spectacles according to the cycloplegic or post-cycloplegic refraction. For children in the beginning of elementary school with nearly symmetrical myopia to a greater degree of more than -3.00 D and small exophoria not requiring treatment, about 50% of the respondents chose to prescribe spectacles with full correction according to the cycloplegic refraction.
In conclusion, Korean ophthalmologists in clinical practice encouraged children to wear O-K lenses more than undercorrected glasses as a way to retard myopia progression, but not to a great extent. However, prescription of O-K lenses is rarely tried in clinical trials. The application of atropine is not considered a trustworthy method to reduce the progression of myopia in treating pediatric patients. As a management practice of pediatric patients with myopia either with or without negligible eyeball deviation, the majority of the practitioners chose to prescribe glasses with full cycloplegic correction.
Figures and Tables
References
1. Saw SM, Tong L, Chua WH, et al. Incidence and progression of myopia in Singaporean school children. Invest Ophthalmol Vis Sci. 2005. 46:51–57.
2. Goldschmidt E. The mystery of myopia. Acta Ophthalmol Scand. 2003. 81:431–436.
3. Lin LL, Shih YF, Tsai CB, et al. Epidemiologic study of ocular refraction among schoolchildren in Taiwan in 1995. Optom Vis Sci. 1999. 76:275–281.
4. Saw SM, Katz J, Schein OD, et al. Epidemiology of myopia. Epidemiol Rev. 1996. 18:175–187.
5. Saw SM, Hong RZ, Zhang MZ, et al. Near-work activity and myopia in rural and urban schoolchildren in China. J Pediatr Ophthalmol Strabismus. 2001. 38:149–155.
6. Chan B, Cho P, Cheung SW. Orthokeratology practice in children in a university clinic in Hong Kong. Clin Exp Optom. 2008. 91:453–460.
7. Heng LS, Khoo CY. Can contact lenses control the progression of myopia? Singapore Med J. 1994. 35:367–370.
8. Rubin ML, Milder B. Myopia--a treatable "disease"? Surv Ophthalmol. 1976. 21:65–69.
9. Bedrossian RH. The effect of atropine on myopia. Ann Ophthalmol. 1971. 3:891–897.
10. Choi TH, Jeong JW, Choi YY. The effect of atropine on myopic progression in children. J Korean Ophthalmol Soc. 2005. 46:1189–1195.
11. Adler D, Millodot M. The possible effect of undercorrection on myopic progression in children. Clin Exp Optom. 2006. 89:315–321.
12. Gwiazda J. Treatment options for myopia. Optom Vis Sci. 2009. 86:624–628.
13. Saw SM, Gazzard G, Au Eong KG, Tan DT. Myopia: attempts to arrest progression. Br J Ophthalmol. 2002. 86:1306–1311.
14. Syniuta LA, Isenberg SJ. Atropine and bifocals can slow the progression of myopia in children. Binocul Vis Strabismus Q. 2001. 16:203–208.
15. Van Meter WS, Musch DC, Jacobs DS, et al. Safety of overnight orthokeratology for myopia: a report by the American Academy of Ophthalmology. Ophthalmology. 2008. 115:2301–2313.e1.
16. McLeod SD. Overnight orthokeratology and corneal infection risk in children. Arch Ophthalmol. 2007. 125:688–689.
17. Chung K, Mohidin N, O'Leary DJ. Undercorrection of myopia enhances rather than inhibits myopia progression. Vision Res. 2002. 42:2555–2559.
18. Tong L, Huang XL, Koh AL, et al. Atropine for the treatment of childhood myopia: effect on myopia progression after cessation of atropine. Ophthalmology. 2009. 116:572–579.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download