Abstract
We report on a case of necrotizing keratoscleritis in primary Sjogren's syndrome. A 66-year-old female patient who was complaining of ocular pain, tearing and decreased vision in her right eye for the previous two days was admitted to our hospital. Visual acuity in the right eye was hand movement, and initial examination showed a 3.0 × 1.8 mm uveal mass bulging through a corneoscleral melting site in the nasal region of the right eye. Positive anti-nuclear antibody was identified at a titer of 1:320 with a speckled pattern, and both Sjogren's syndrome A and Sjogren's syndrome B antibody tests were positive, with titers >200 U/mL. A technetium 99m pertechnetate salivary scan revealed chronic sialoadenitis in the submandibular glands. We diagnosed the lesion as necrotizing keratoscleritis due to primary Sjogren's syndrome. A corneoscleral patch graft was performed, followed by immunosuppression including oral cyclosporin and topical prednisolone. During a follow-up period of 12 months, the corneoscleral graft was well maintained with no recurrence.
Sjogren's syndrome is a chronic autoimmune disorder affecting mainly middle-aged women. It is characterized by lymphocytic infiltration and destruction of the exocrine glands (mainly the salivary and lacrimal glands), resulting in dry mouth and eyes [1]. Although keratoconjunctivitis sicca is the major ocular manifestation in Sjogren's syndrome, severe corneal lesions with or without inflammation have also been rarely reported [2,3]. We describe a case of necrotizing keratoscleritis associated with primary Sjogren's syndrome.
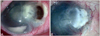
A 66-year-old woman was admitted complaining of ocular pain, tearing, and decreased vision in her right eye for the previous two days. She had hypertension and diabetes mellitus and had received a cataract operation through a superior corneal incision in the right eye five years previous. She had been treated for dry eye syndrome and recurrent infectious keratitis for the past two years at a private clinic, but she had not received any prescription for antibiotic treatment during the most recent two months. In the initial examination, the patient's corrected visual acuity was hand movement oculus dexter (OD). Slit lamp examination showed a 3.0 × 1.8 mm uveal mass bulging through a corneoscleral melting site in the nasal region of the right eye. Surrounding stromal opacity with corneal neovascularization and hypopyon were noted (Fig. 1). The patient had only superficial epithelial keratitis in the opposite eye. Chest X-ray, complete blood count, liver function test, renal function test, and coagulation profile were performed along with examination of autoimmune laboratory markers including anti-nuclear antibody (ANA), anti-neutrophil cytoplasmic antibody, rheumatoid arthritis (RA) factor, Sjogren's syndrome A (SSA) and Sjogren's syndrome B (SSB), anti-dsDNA, anti-Smith, anti-ribonecleo protein, anti-centromere, anti-cardiolipid, and anti-Scl-70 antibodies. An emergent corneoscleral patch graft was performed. The results of the Gram-stained smears, KOH mounting, and bacterial and fungus cultures conducted pre- and intra-operatively were all negative. Laboratory studies showed an elevated eosinophil level (9.3%), positive RA factor as determined by at a titer of 169 IU/mL, and positive ANA at a titer of 1:320 with a speckled pattern. Both SSA and SSB antibody tests were positive at titers >200 U/mL. Other laboratory findings were normal, and the patient did not have any articular symptoms. A technetium 99m pertechnetate salivary scan revealed chronic sialoadenitis in the submandibular glands. Therefore, we diagnosed the lesion as necrotizing keratoscleritis due to primary Sjogren's syndrome, and started immunosuppressive therapy including oral cyclosporin A (Cipol-N; Jongkeun Pharmacy, Seoul, Korea) and topical 1% prednisolone acetate (Pred Forte; Allergan, Irvine, CA, USA). Topical steroid application was maintained every hour for one month, was tapered to every four hours after two months, and the patient was slowly weaned from the drug by six months. Oral cyclosporine A was maintained at 200 mg for two months and tapered off over four months. Twelve months later, the previous corneoscleral patch graft was well maintained with no recurrence. Visual acuity was hand movement OD.
Most patients with scleritis have immune-mediated diseases, and up to half of affected individuals have an identifiable systemic illness. Rheumatoid arthritis is the most commonly associated systemic disease in patients with scleritis, followed by Wegener's granulomatosis, relapsing polychondritis, systemic lupus erythematosus, inflammatory bowel disease, and polyarteritis nodosa [4]. In the case presented here, autoimmune markers, chest X-ray, and systemic symptoms of the patient showed no evidence of this autoimmune diseases.
Sjogren's syndrome is a slowly progressing autoimmune disease, observed in 0.5% to 1.0% of the population. Systemic features, resulting from cutaneous, respiratory, renal, hepatic, neurologic, and vascular involvement, often occur. Corticosteroids, cyclophosphamide, and nucleoside analogues are reserved for severe extraglandular manifestations of Sjogren's syndrome [1].
Previously, Ahmadi-Simab et al. [5] reported a case of successfully treated refractory anterior scleritis in primary Sjogren's syndrome using rituximab. Cohen [2] reported two cases of sterile corneal perforation after cataract surgery in Sjogren's syndrome, and Vivino et al. [3] reported a case of repeated corneal melting and ulceration as the initial presentation of primary Sjogren's syndrome. However, to our knowledge, this is the first report of necrotizing keratoscleritis in primary Sjogren's syndrome.
In this case, corneoscleral perforation had developed only two days after the initial symptoms first occurred. This rapid progression might have been caused by previous corneoscleral thinning due to recurrent inflammation of the lesion. We were able to rule out infection via pre- and intra-operative smear and culture of the affected lesion and diagnosed the lesion as being due to primary Sjogren's syndrome via serologic examination, sialoscintigraphy, and typical symptoms. A corneoscleral patch graft was performed and followed by immunosuppression including oral cyclosporin and topical prednisolone. An oral steroid was not administered because the patient also had uncontrolled diabetes mellitus. In conclusion, based on this experience, for clinically suspected necrotizing keratoscleritis, evaluation for Sjogren's syndrome is recommended.
Figures and Tables
References
1. Mavragani CP, Moutsopoulos HM. Conventional therapy of Sjogren's syndrome. Clin Rev Allergy Immunol. 2007. 32:284–291.
2. Cohen KL. Sterile corneal perforation after cataract surgery in Sjogren's syndrome. Br J Ophthalmol. 1982. 66:179–182.
3. Vivino FB, Minerva P, Huang CH, Orlin SE. Corneal melt as the initial presentation of primary Sjogren's syndrome. J Rheumatol. 2001. 28:379–382.
4. Smith JR, Mackensen F, Rosenbaum JT. Therapy insight: scleritis and its relationship to systemic autoimmune disease. Nat Clin Pract Rheumatol. 2007. 3:219–226.
5. Ahmadi-Simab K, Lamprecht P, Nolle B, et al. Successful treatment of refractory anterior scleritis in primary Sjogren's syndrome with rituximab. Ann Rheum Dis. 2005. 64:1087–1088.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download