Abstract
Purpose
To identify the long term clinical course of amblyopia and strabismus that developed secondary to a monocular corneal opacity following suspected epidemic keratoconjunctivitis (EKC) in infancy.
Methods
This was a retrospective study analyzing the medical records of seven patients, treated in our clinic, who were followed for more than five years.
Results
Four patients in our clinic underwent a corneal ulcer treatment following suspected EKC. Each developed a monocular corneal opacity. Three patients with a chief complaint of corneal opacity were transferred to our clinic from other clinics. These patients had documented histories of treatment for EKC in infancy. All patients were treated with early occlusion therapy, but amblyopia persisted in four patients. Furthermore, all patients had strabismus and showed a significant reduction of stereoscopic vision.
Conclusions
Although infants with EKC are not always cooperative, slit lamp examination should be performed as early as possible, and appropriate medical treatment should be performed, thus reducing the development of corneal opacity. Careful follow up should be regularly performed, and the occurrence of amblyopia or strabismus should be verified at an early stage using visual acuity or ocular alignment examination. Ophthalmologic treatments, including active occlusion therapy, should also be pursued.
Epidemic keratoconjunctivitis (EKC) is a relatively common ocular disease caused by human adenoviruses. EKC is characterized by having not only symptoms that include foreign body sensation, and pruritus, but also signs including unilateral or bilateral hyperemia, discharge, blepharoedema, chemosis, follicular and papillary conjunctival response as well as the findings of membranes on slit lamp examination [1-3]. In most cases, EKC is easily diagnosed based on clinical symptoms and slit lamp examination. Adults may complaint of visual disturbances due to subepithelial corneal opacity developing after EKC. However, most patients completely recover without any side effects after a two to three week clinical course [1,3,4]. EKC is much more difficult to diagnose in infants, since they are less cooperative in ophthalmic examinations. The development of a corneal ulcer due to membrane formation in the progression of the disease may cause a corneal opacity to form in one eye, even after complete healing of the keratoconjunctivitis [1,4,5].
Various studies have reported that once there is a corneal opacity in one eye, induced either by infection or trauma, complications such as amblyopia, strabismus, or reduced stereoscopic vision can develop, even if the opacity is not severe [6-10].
The high prevalence of EKC as opposed to other ocular diseases. has not resulted in many reports on amblyopia, strabismus or impairment of sensory function caused by EKC induced corneal opacity. Thus, we sought to determine the long term clinical course of the amblyopia and strabismus following EKC induced corneal opacity formation in infants.
This study was a retrospective one to analyze the medical records of seven patients, who were treated for more than five years in our clinic between June 1992 and February 2001. Some of these patients underwent corneal ulcer treatment following EKC and developed a corneal opacity in one eye. Other patients, whose medical histories of infant EKC were verified, were treated for corneal opacity induced amblyopia or strabismus. We collected data on each patient. This data included each patient's age at the time of the EKC infection, the type of corneal opacity, visual acuity, refractive error, the beginning period of occlusion therapy, the period of development, and the type of strabismus and stereoscopic vision. Corneal opacity was graded using Fantes classification [11].
Visual acuity examination was performed during the course of observation when measurement was possible using a pictured visual acuity test chart. If visual acuity examination was not possible during the first medical examination with a numbered visual acuity chart, then a picture visual acuity chart was used for initial visual acuity measurement. Visual acuity was examined using a numbered visual acuity chart as early as possible. All patients underwent refractive error correction and visual acuity examination after cycloplegic refraction. Visual acuity was measured using a projection chart (Topcon auto chart projector; Topcon, Tokyo, Japan), and measured values were assessed by conversion to logarithm of the minimal angle of resolution (logMAR) [12].
An alternate prism cover test was used to measure the angle of strabismus in the far and near distance after the patient had been corrected for refractive error. The motor function of the external ocular muscles was tested using duction and version tests. The Lang and Titmus test were used for stereopsis. In addition, the Worth four-dot test and afterimage test were performed to assess sensory function.
Four patients were male, and three were female. Suspected EKC occurred in all patients within one year after birth. The mean age of EKC development was 5.0 ± 3.6 months (range, 1 to 12 months). The mean follow up period was 9.4 ± 2.8 years (range, 5 to 11.5 years). Four patients visited our clinic with chief complaints of monocular edema, hyperemia, and discharge. Chemosis, follicle formation, papillary conjunctival reaction, and corneal ulceration were noted on the slit lamp examination. Three of these four patients were admitted to the hospital and were medically treated. No patients had systemic symptoms.
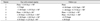
The remaining three patients with a chief complaint of corneal opacity were transferred to our clinic from other clinics. These patients had previously documented histories of treatment for suspected EKC, and monocular corneal opacity was noted on slit lamp examination. All patients showed post suspected EKC monocular corneal opacity located in the central cornea, with Fantes classification [11] grade 2, corneal opacity was easily identified on slit lamp examination (Table 1).
Visual acuity examination was not possible at the first visit in these patients due to their young age. During the follow up period, the mean best corrected visual acuity (BCVA) in the eyes with corneal opacity on the first medical examination was logMAR 1.17 ± 0.64 (range, 2 to 0.4). The mean BCVA in the normal eyes was logMAR 0.40 ± 0.15 (range, 0.6 to 0.2) at that time, and all seven patients had amblyopia.
Cycloplegic refraction was performed in all patients, and glasses were prescribed for correction of refractive error, as needed. In cases of refractive error, patients with a corneal opacity showed myopia (1 patient), astigmatism (2 patients), myopic astigmatism (2 patients), or hyperopic astigmatism (2 patients). Three patients had anisometropia. One patient had anisometropia with myopia in one eye and hyperopia in the other eye. Two patients had compound hyperopic anisometropia, where both eyes were hyperopic, but to differing degrees (Table 2).
Occlusion therapy was performed in all patients, and the mean period from the time of suspected EKC treatment until the beginning of occlusion therapy was 24.58 ± 18.46 months (range, 3 to 46 months). Occlusion therapy was begun 30.93 ± 15.63 months (range, 10 to 48.5 months). Initial occlusion durations were half of awakened hours (4 to 6 hours), duration of occlusion and frequencies of visits were determined according to the response to occlusion therapy and patients' compliance. We recommended at least one hour of near visual activities such as reading a book, dictation, computer or video game, and television watching, while patched.
The mean BCVA were logMAR 0.36 ± 0.38 (0.7 to 0.0) and logMAR 0.03 ± 0.05 (0.1 to 0.0) for eyes with corneal opacity and for normal eyes, respectively, at the final visit. Four patients (57%) showed amblyopia at the final visit (Table 3). Patients with anisometropia showed amblyopia, even at the final follow up visit.
Of the four patients who visited our clinic with suspected EKC symptoms, three showed orthophoria at the first visit. Ocular alignment examination was not carried out for the remaining since cooperation was poor. Three patients who had been transferred to our clinic with a chief complaint of corneal opacity showed 10 prism diopters (PD) of exotropia, 8 PD of exotropia, and 25 PD of exotropia with dissociated vertical deviation at the first visit. During the follow up period, all seven patients showed strabismus, and the mean period from the time of suspected EKC onset until the appearance of strabismus was 3.0 ± 2.2 years (range, 0.4 to 7 years). The types of strabismus included esotropia (1 patient), constant exotropia (1 patient), intermittent exotropia (2 patients), exotropia with dissociated vertical deviation (1 patient), intermittent exotropia with inferior oblique overaction (1 patient), and intermittent exotropia with dissociated vertical deviation (1 patient). The deviated angles of each patient are shown in Table 4.
The Lang test, Titmus test, Worth four-dot test and afterimage test were performed during the follow up period, when patients cooperated. Only two of the seven patients (28.6%) could pass the Lang test. Titmus test results varied from a case in which 50 seconds to a case in which a fly wing could caught in 3,000 seconds with stereoscopic vision. On the Worth four-dot test, fusion was seen in two patients (28.6%). On the afterimage test, all seven patients (100%) showed normal retinal correspondence (Table 5).
Infection-induced monocular corneal opacity may cause a decline in the development of visual acuity or may lead to ocular motor abnormalities in infants [6-10]. Beneish et al. [7] reported amblyopia in five infants, who had developed corneal opacity after suffering from herpes keratitis. They emphasized the importance of refractive error correction and early occlusion therapy, along with scrupulous follow up for infants. Cameron and Mullaney [8] also reported corneal opacity and amblyopia among infants with vernal keratoconjunctivitis. They asserted that the probability of opacity formation should be minimized, if the corneal epithelial defect is stimulated to regenerate at an early stage. They further suggest prompt occlusion therapy in patients that develop amblyopia after corneal opacity formation. As a consequence, good visual prognosis may be expected.
In comparison with other diseases, such as herpes keratitis or vernal keratoconjunctivitis, EKC has a high prevalence rate and is highly infective. Nevertheless, since relapses are not common and the clinical course is self-limiting, post EKC corneal opacity may often be overlooked, and the opportunity for regular scrupulous follow up observation may be missed.
In general, diagnosis of EKC are mainly clinical. EKC is diagnosed as typical symptoms such as an acute onset red eye with watery discharge, contagion of fellow eye in a few days and so on. Viral isolation are the most clear and definite options for the diagnosis of EKC. But they are expensive, slow, uncomfortable and not routinely used even if it is endemic disease in Korea. Our patients have also characters; contagious to family, fellow eye infection, typical symptoms. And they got a corneal specialist diagnosis.
In this study, all patients showed a visual acuity difference of two lines or more on the initial measurement of visual acuity. Although occlusion therapy was implemented at an early stage, four patients (57%) showed amblyopia at the final follow up visit.
Generally, amblyopia may develop caused by strabismus, anisometropia and visual stimulus deprivation in the critical period of visual development. Amblyopia caused by corneal opacity after infectious ocular surface disease could be induced by two specific things: 1) opacity-induced blockage of proper visual stimulation required for visual development and 2) anisometropia-induced defocusing of the image on one retina leading to blunting of visual pathway development in the affected eye [6]. All seven patients had suspected post EKC opacity of the central cornea sufficiently large to be easily seen on slit lamp examination. Early occlusion therapy was performed in all patients, who achieved good visual development, and some patients showed improvement in visual acuity. However, patients with anisometropia showed poor visual acuity at final follow up, despite undergoing early occlusion therapy. This study showed that patients with anisometropia induced by corneal opacity might have poor prognosis of visual prognosis.
All patients had strabismus of one type or another during the follow up, including esotropia, exotropia, exotropia with dissociated vertical deviation, and exotropia with inferior oblique overaction. Four of the seven patients underwent strabismus surgery. Because stereoscopic vision is the high binocular visual function of both eyes, the presence of strabismus, amblyopia or anisometropia in infants could be acutely affected in the random dot stereotest [13]. Only two patients passed the Lang test. They showed relatively good stereoscopic vision even on the Titmus test in comparison with the other patients.
With respect to the quantitative sensory test, only two patients with good stereoscopic vision also showed fusion on the Worth four-dot test. Two patients with good stereoscopic vision and the Worth four-dot test results had less difference in visual acuity or refractive error between their eyes at an early stage, compared with other patients. These two patients also exhibited good final visual acuity. Less pronounced visual acuity and refractive error differences between the two eyes suspected of early EKC were associated with better visual acuity and stereoscopic vision. All patients showed normal retinal correspondence on afterimage test. This was due to the fact that strabismus occurred through a sudden corneal opacity development. There was no time to adapt to the new sensory changes, and normal retinal correspondence was maintained owing to abruptly developed amblyopia.
In this study, all seven patients, who underwent long-term follow up due to monocular corneal opacity development after suspected EKC, developed amblyopia. These patients were treated with early occlusion therapy, but amblyopia remained in more than half of them (4 / 7, 57%), even after occlusion therapy was implemented. Furthermore, all patients had strabismus and deceased stereoscopic vision. Thus, although cooperation is difficult to secure in infants with suspected EKC, slit lamp examination should be performed as often as possible, and appropriate medical treatment should be instituted, thus minimizing the possibility of corneal opacity development. Those cases in which the corneal opacity remains, the clinical course of the disease should be well explained to the patient's parents. Careful follow up should be regularly performed, and the occurrence of amblyopia or strabismus should be verified at an early stage using visual acuity, and ocular alignment examination. Ophthalmologic treatments, including active occlusion therapy, should also be pursued.
Figures and Tables
References
1. Kim SY, Park KS, Kim JH, Kim SM. A statistic observation of the clnical epidemic keratoconjunctivitis. J Korean Ophthalmol Soc. 1969. 10:15–19.
2. Ishii K, Nakazono N, Fujinaga K, et al. Comparative studies on aetiology and epidemiology of viral conjunctivitis in three countries of East Asia--Japan, Taiwan and South Korea. Int J Epidemiol. 1987. 16:98–103.
3. Schrauder A, Altmann D, Laude G, et al. Epidemic conjunctivitis in Germany, 2004. Euro Surveill. 2006. 11:185–187.
4. Lund OE, Stefani FH. Corneal histology after epidemic keratoconjunctivitis. Arch Ophthalmol. 1978. 96:2085–2088.
5. Alsuhaibani AH, Sutphin JE, Wagoner MD. Confocal microscopy of subepithelial infiltrates occurring after epidemic keratoconjunctivitis. Cornea. 2006. 25:1102–1104.
6. Von Noorden GK. Factors involved in the production of amblyopia. Br J Ophthalmol. 1974. 58:158–164.
7. Beneish RG, Williams FR, Polomeno RC, Flanders ME. Herpes simplex keratitis and amblyopia. J Pediatr Ophthalmol Strabismus. 1987. 24:94–96.
8. Cameron JA, Mullaney PB. Amblyopia resulting from shield ulcers and plaques of the cornea in vernal keratoconjunctivitis. J Pediatr Ophthalmol Strabismus. 1997. 34:261–262.
9. Chong EM, Wilhelmus KR, Matoba AY, et al. Herpes simplex virus keratitis in children. Am J Ophthalmol. 2004. 138:474–475.
10. Jones SM, Weinstein JM, Cumberland P, et al. Visual outcome and corneal changes in children with chronic blepharokeratoconjunctivitis. Ophthalmology. 2007. 114:2271–2280.
11. Fantes FE, Hanna KD, Waring GO 3rd, et al. Wound healing after excimer laser keratomileusis (photorefractive keratectomy) in monkeys. Arch Ophthalmol. 1990. 108:665–675.
12. Jin YH. A new logMAR vision chart: Jin's vision chart. J Korean Ophthalmol Soc. 1997. 38:2036–2044.
13. Lee BH, Kim MM. Comparisons of the Lang, Randot, TNO and new stereo tests in screening and office use in children. J Korean Ophthalmol Soc. 1990. 31:651–660.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download