Abstract
A 60-year-old male was referred to the ophthalmologic clinic with aggravated anterior uveitis and corneal edema despite the use of topical and systemic steroids. He had undergone cataract surgery in both eyes 15 years previous. Slit lamp examinations revealed a retained lens fragment in the inferior angle of the anterior chamber, with severe corneal edema and mild anterior uveitis. The corneal edema and uveitis subsided following surgical extraction of the lens fragment. That a retained lens fragment caused symptomatic anterior uveitis with corneal edema 15 years after an uneventful cataract surgery is unique. A retained lens fragment should be considered as one of the causes of anterior uveitis in a pseudophakic patient.
In uneventful phacoemulsification, lens fragments may be hidden beneath the iris and may not be visible after the procedure [1]. Although the clinical features and management of retained lens fragments in the posterior segment have been well described [2-6], there is limited published data about those in the anterior segment. After cataract surgery, retained nuclear fragments in the anterior segment may cause persistent postoperative inflammation and corneal edema [7]. We present a case in which a retained lens fragment caused anterior uveitis with severe corneal edema 15 years after cataract surgery.
A 60-year-old male was referred to the ophthalmology clinic with recurrent uveitis of the right eye and severe corneal edema. He had undergone cataract surgery in both eyes 15 years previous. He denied any history of ocular trauma or ocular surgery other than cataract surgery. He had been diagnosed with anterior uveitis one month previous at a private eye clinic, for which administration of topical 1% prednisolone acetate led to remission. Anterior uveitis recurred with severe corneal edema one month after the first episode. Despite topical and systemic steroid treatment, the anterior chamber (AC) inflammation and corneal edema worsened, leading to the referral of this patient to our clinic.
At initial presentation, visual acuity was 0.2 OD, and 0.9 OS using a Snellen visual acuity chart. Intraocular pressure (IOP) was 15 mmHg OD and 17 mmHg OS as measured with a non-contact tonometer (NCT). An OD slit lamp examination revealed grades 1 and 2 AC reactions with flare and severe corneal edema. A small whitish fragment, previously diagnosed as hypopion at the private eye clinic, was observed in the inferior portion of the AC (Fig. 1). After dilation with mydriatics, a retained lens fragment was identified in the superior capsule. The OD vitreous and fundus were not visualized due to severe corneal edema, but B-ultrasonography revealed no remarkable signs. Specular pachymetry of the right eye was not possible due to the severe corneal edema and endothelial decompensation. It was concluded that the whitish material in the inferior angle of the AC was a retained lens fragment, because a retained lens fragment was also discovered in the superior capsule.
Surgery was performed on the right eye under local anesthesia. A clear corneal incision was made at the superior cornea, and hyaluronate sodium (13.8 mg/0.6 mL/SYR, Healon 5 inj; Meditip Co., Seoul, Korea) was injected into the anterior chamber. The lens fragment was removed with lens forceps, and the remaining hyaluronate sodium was removed with irrigation and aspiration (Stellaris Vision Enhancement System; Bausch & Lomb, Rochester, NY, USA).
On postoperative day 1, OD corneal edema was slightly aggravated, and visual acuity was limited to a finger count at 10 cm. Measurement with NCT revealed an IOP of 15 mmHg. After one month, OD corneal edema was much improved, and visual acuity had increased to 0.4 by Snelln visual acuity chart. A two-month post-operative OD follow-up examination revealed reduced corneal edema and subsequent improvement of visual acuity to 0.7 by Snellen visual acuity chart (Fig. 2). Although the OD cornea was clear, an endothelial cell count showed 458 cells/mm2, and specular pachymetry revealed significant loss of hexagonality (Fig. 3A and 3B).
Postoperative anterior segment inflammation after cataract surgery can be a difficult diagnostic and management problem. Causes of late onset postoperative inflammation include retained lens fragments, reactivated uveitis, and infections, such as endophthalmitis and wound abscess [8]. Late onset of corneal edema after a cataract surgery also has been reported to be caused by retained lens fragments [7-9], intraocular lens fragments [10], and endothelitis [11].
A retained lens fragment in the anterior segment after phacoemulsification with an intact posterior capsule is an uncommon complication. A retained cortical fragment causes an inflammatory reaction that can generally be treated with topical corticosteroids, resulting in resolution of the inflammation and resorption of the cortical material. Retained unencapsulated nuclear material frequently causes an inflammatory reaction in the AC as well as corneal edema of varying severity [8].
There have been several hypotheses for retained nuclear fragments in the AC. Bohigian and Wexler [7] suggested that direct mechanical trauma to the corneal endothelium played a role in the corneal edema caused by retained AC lens fragments. Some researchers have suggested that lens fragments may be trapped in the posterior chamber during phacoemulsification in high myope patients with small pupils and a hard nucleus, especially if significant shattering of fragments occurs during phacoemulsification [8,12]. Together with the lens fragments themselves, lens epithelial cells on those fragments may play a role in this inflammation [13].
In the present case, the patient had undergone cataract surgery at another other eye clinic 15 years previous; it was impossible to determine the preoperative refractive errors and keratometry values. Anterior uveitis with corneal edema was refractory despite topical and systemic steroid therapy, so the lens fragment in this patient was thought to be a nuclear fragment. As in prior cases, surgical removal of the nuclear fragment was required in order to improve the AC reaction and corneal edema [7-9]. A unique feature of this case is that the interval between cataract surgery and anterior uveitis was 15 years. In previous cases, the interval was between 6 weeks to 27 months, much shorter than in this case [7-9,14,15].
We hypothesize that the lens fragment in this patient remained sequestered behind the iris or posterior chamber for 15 years after cataract surgery. The lens fragment might have produced a mild AC reaction without significant visual disturbance. Alternatively, the lens fragment may have been sequestered in the posterior capsule with no inflammation after the cataract operation. It is possible that the lens fragment migrated into the anterior chamber, possibly due to minor trauma or capsule deformation during fibrosis, leading to the acute onset of the AC reaction with severe corneal edema. At the first diagnosis of anterior uveitis one month before the initial visit to our clinic, the lens fragment might have been located in the inferior angle, as in a previously recorded case [9]. The lens fragment might have migrated to the surface of the iris to come into contact with the corneal endothelium, leading to corneal edema and decreased vision.
This case highlights that retained lens fragments should be considered as causes for anterior uveitis in a pseudophakic eye, even years after cataract surgery. This case has shown that the time interval between surgery and anterior uveitis can be as long as 15 years. Therefore, when a pseudophakic patient presents with anterior uveitis, a possible hidden lens fragment should be considered. In such cases careful examination including gonioscopy should be performed. In a patient with some cortical remnant, especially within the superior lens capsule, a follow-up showed be performed to assess the possibility of lens fragment migration and subsequent chronic uveitis.
Figures and Tables
Fig. 1
Slit lamp examination shows the lens fragment in the inferior portion of the anterior chamber of the right eye.

Fig. 2
Slit lamp examination two months after removal of the lens fragment shows improved corneal edema.
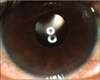
Fig. 3
Specular pachymetry two months after removal of the lens fragment shows a significant decrease in endothelial cell count (458 cells/mm2) and loss of hexagonality in the right eye. (A) Right eye. (B) Left eye. R=right; C=photograph serial number; T=corneal thickness; N=no. of cells picked up; Min=minimum cell area; Max=maximum cell area; AVG=average cell area; SD=standard deviation; CV=coefficient of variation; CD=cell density; L=left.

References
1. Dick HB, Kohnen T, Jacobi FK, Jacobi KW. Long-term endothelial cell loss following phacoemulsification through a temporal clear corneal incision. J Cataract Refract Surg. 1996. 22:63–71.
2. Kim IK, Miller JW. Management of dislocated lens material. Semin Ophthalmol. 2002. 17:162–166.
3. Tommila P, Immonen I. Dislocated nuclear fragments after cataract surgery. Eye (Lond). 1995. 9(Pt 4):437–441.
4. Wong D, Briggs MC, Hickey-Dwyer MU, McGalliard JN. Removal of lens fragments from the vitreous cavity. Eye (Lond). 1997. 11(Pt 1):37–42.
5. Gilliland GD, Hutton WL, Fuller DG. Retained intravitreal lens fragments after cataract surgery. Ophthalmology. 1992. 99:1263–1267.
6. Stefaniotou M, Aspiotis M, Pappa C, et al. Timing of dislocated nuclear fragment management after cataract surgery. J Cataract Refract Surg. 2003. 29:1985–1988.
7. Bohigian GM, Wexler SA. Complications of retained nuclear fragments in the anterior chamber after phacoemulsification with posterior chamber lens implant. Am J Ophthalmol. 1997. 123:546–547.
8. Hui JI, Fishler J, Karp CL, et al. Retained nuclear fragments in the anterior chamber after phacoemulsification with an intact posterior capsule. Ophthalmology. 2006. 113:1949–1953.
9. Gedde SJ, Karp CL, Budenz DL. Retained nuclear fragment in the anterior segment. Arch Ophthalmol. 1998. 116:1532–1533.
10. Hoffman RS, Fine IH, Packer M. Retained IOL fragment and corneal decompensation after pseudophakic IOL exchange. J Cataract Refract Surg. 2004. 30:1362–1365.
11. Olsen TW, Hardten DR, Meiusi RS, Holland EJ. Linear endotheliitis. Am J Ophthalmol. 1994. 117:468–474.
12. Goodfellow JF, Whitefield LA. Retained lens fragments. Ophthalmology. 2008. 115:414–415.
13. Majima K. Lens epithelial cells in postoperative aqueous humor. Jpn J Ophthalmol. 1997. 41:55–58.
14. Bagga A, Soukiasian SH, Cotran PR, Speert PK. Delayed appearance and consequences of retained nuclear fragments after uneventful phacoemulsification. Invest Ophthalmol Vis Sci. 2004. 45:E-Abstract 290. 290-B263.
15. Teo L, Chee SP. Retained lens fragment in the anterior segment as a cause of recurrent anterioruveitis. Int Ophthalmol. 2010. 30:89–91.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download