Abstract
Purpose
To compare the effects of performing a single limbal relaxing incision (LRI) combined with a clear corneal incision on a corneal astigmatism with that of paired LRIs in cataract surgery.
Methods
Medical records for 25 eyes in 20 patients who had undergone LRIs during cataract operations for with-the-rule astigmatism of 1.5 diopters (D) or more in topography were retrospectively reviewed. Single or paired LRIs were assigned randomly and were performed on the steepest axis; the degrees of arc were determined using the modified Gills nomogram. A clear corneal wound was made on the steepest vertical axis. Uncorrected visual acuity (UCVA), best corrected visual acuity (BCVA), manifest refraction, and corneal astigmatism on topography were evaluated preoperatively and one month postoperatively. Naeser's polar value analysis was used to assess the efficacy of the LRIs.
Results
The mean depth of the LRIs and degrees of arc were 620±31 µm (87.1% of corneal thickness) and 56.84±19.68°, respectively. The mean postoperative UCVA and BCVA (log MAR) were significantly improved (0.51±0.37 and 0.09±0.12, respectively) (p<0.05). Average refractive and corneal astigmatisms were significantly reduced by 49.4 percent and 32.4 percent, respectively (p<0.05). The single LRI combined with clear corneal incision showed reduced efficacy in refractive astigmatism by 47 percent, which is similar to that of paired LRIs where a 48 percent reduction in efficacy was seen.
Recently, the need to manage pre-existing astigmatism has become a requisite aspect of modern phacosurgery, especially when multifocal presbyopic lenses are supposed to be implanted. Experience with keratorefractive surgery has proved that an astigmatism of as little as 0.75 diopters (D) may leave a patient symptomatic, with visual blur, ghosting, and halos. Introduction of multifocal lenses for presbyopia seems to force the need to perform limbal relaxing incisions (LRIs) for astigmatism reduction.
LRIs have been used to correct pre-existing corneal astigmatism at the time of cataract surgery [1-5]. LRIs are effective in eyes with low to moderate, and even high, astigmatism. These incisions also appear to cause less distortion and irregularity on corneal topographies than corneal relaxing incisions and arcuate keratotomy. They can provide more rapid postoperative vision and carry less risk of inducing glare and discomfort [3].
Generally, paired incisions are preferred to optimize symmetrical corneal flattening in LRIs. However, sometimes, double relaxing incisions may complicate cataract surgery due to leakage from the clear corneal wound, which is made over one of the relaxing incisions. When the corneal incision for cataract surgery is supposed to be made along the same axis, the single relaxing incision with clear corneal wound present in the opposite direction may have a similar effect on astigmatic correction, as compared with the paired relaxing incision. Because with-the-rule (WTR) astigmatism often occurs in elderly cataract patients, we investigated the effects of performing single or paired LRIs on corneal WTR astigmatisms when combined with the clear corneal wound in cataract surgery.
A retrospective study was conducted by reviewing medical records for patients who had cataracts and a WTR astigmatism of 1.5 D or more in preoperative topography, and had undergone phacoemulsification and posterior chamber intraocular lens implantation combined with LRIs between April 2006 and December 2007. A WTR astigmatism was defined when a patient's Sim K was between 45 and 135 degrees in topography.
Exclusion criteria included irregular corneal astigmatism, keratoconus or keratoconus suspect, current uveitis, marked corneal scarring (apart from cataract surgery), pannus, and pterygium. Eventful surgery was also excluded. A complete general ophthalmic examination was performed on all patients including testing uncorrected visual acuity (UCVA), best corrected visual acuity (BCVA), keratometry and autorefractometer readings, slitlamp and retinal evaluation, tonometry, pachymetry, and corneal topography. Pachymetric readings were taken from the central cornea and eight peripheral areas (1.5, 3, 4.5, 6, 7.5, 9, 10.5, and 12 o'clock positions). The degree of arc was determined using the modified Gills nomogram [5]. Single or paired incisions were randomly assigned regardless of the amount of astigmatism. Single LRI was defined as making the main clear corneal incision and the LRI in opposing directions; paired LRI was defined as making an additional LRI in the same direction along with the main corneal incision together with the LRI in opposing direction.
All procedures were performed by one surgeon using topical anesthesia. Patients were instructed to fixate on a microscope light. Prior to surgery, the steep meridian was identified with a surgical marking pen. Based on the procedure described by Langerman [6], a vertical limbal relaxing wound was created with a guarded micrometer diamond blade (MEYCO, Biel, Switzerland) by making a groove concentric to the limbus. The incision depth was equal to approximately 85% of the peripheral corneal thickness at the axis to be cut. After the single or paired incision was made, the penetrating clear corneal incision (CCI) was made along the steepest axis in the upper area for the cataract surgery, along the same axis as the LRI. Uneventful phacoemulsification was then performed, and an intraocular lens was inserted.
Following surgery, Ciprofloxacin (Cravit) and prednisolone acetate eyedrops (Pred Forte) were taken 4 times a day for 2 weeks, and Diclofenac sodium (Diclan) was applied 4 times per day for one month. Patients were examined at one day, one week, and one month postoperatively (Fig. 1, 2).
The changes in corneal and refractive astigmatism were evaluated by corneal topography and retinoscopy. To account for surgically induced changes in the astigmatism axis, the polar value concept described by Naeser et al. [7] was used. The astigmatism correction rate was calculated, as follows: astigmatism correction rate=((preoperative astigmatic polar value (AKP)-postoperative astigmatic polar value (AKP))/preoperative AKP)×100%. The effectiveness of the LRIs was analyzed with respect to the incision depth and the number of incisions performed. Mann-Whitney U tests for intergroup comparison and the Wilcoxon test for intragroup comparison were conducted using Windows SPSS ver. 12.0 (SPSS Inc., Chicago, IL,USA).
The mean age of the patients was 50.3±16.8 years. Five patients were male, and fifteen were female. The preoperative mean spherical equivalents and astigmatism magnitudes in manifest refraction were -4.52±7.98 D and 3.18±1.80 D, respectively. The average preoperative topographic astigmatism and Sim K axis values were 2.71±1.35 D and 90.91±8.87°, respectively. Baseline characteristics are summarized in Table 1. Surgical parameters for the single LRI with clear corneal incision (CCI) and paired LRIs with CCI are listed in Table 2. There was no significant difference in cutting depth, cutting angle, or preoperative corneal thickness between the single LRI with CCI and paired LRIs with CCI groups. Table 3 shows data describing final surgical outcomes for the patients. Significant improvement in UCVA, BCVA, and refractive and corneal astigmatism was seen when compared with the preoperative data. Both average refractive and corneal astigmatism were significantly reduced by 49.4 percent (p=0.002) and 32.4 percent (p=0.029), respectively. Surprisingly, the single LRI with CCI procedure produced reduction effects on the astigmatism, comparable to the paired LRIs with CCI procedure done along the same axis Table 4.
Astigmatism currently has a significant influence on uncorrected visual acuity following cataract surgery. To acquire good postoperative, uncorrected visual acuity, the astigmatism should be minimized preoperatively.
Refractive surgical procedures on eyes with astigmatism include arcuate keratotomy, photorefractive keratectomy (PRK), laser in situ keratomileusis (LASIK), toric phakic intraocular lenses, and a combination of techniques [7-14]. Arcuate keratotomies or corneal relaxing incisions have limited predictability and often result in overcorrection, especially in eyes with low and moderate astigmatism [3]. Currently, LRIs are the preferred technique to reduce pre-existing astigmatism at the time of cataract surgery. LRIs appear to have potential advantages over corneal relaxing incisions or arcuate keratotomy by causing less distortion and irregularity on corneal topographies and less variability in refraction as they are placed at the limbus. They can provide earlier stability in postoperative vision and may carry a lower risk of inducing glare and discomfort. Precise placement on the axis is not as critical as in arcuate keratotomy because the incisions are more peripheral and longer. They are also more forgiving with incision depth than arcuate keratotomy and are easier to perform [3].
Current reports show variable reduction effects on astigmatism by performing LRIs. Budak et al reported an absolute decrease in mean astigmatism of 44 percent [15], Bayramlar et al. [16] 52 percent, Kaufmann et al. [5] 25 percent, and Carvalho el al. [17] 50 percent. Our study showed that LRIs achieve a 49 percent reduction effect for refractive total astigmatism, and 32 percent for corneal astigmatism, which is comparable with other studies. We found the reduction effects of astigmatism in the corneal plane to be less than that in the refractive plane. One possible explanation for this may be that the high astigmatism seen in some patients may originate from not only the cornea but also the lens. Therefore, removal of the lens might have an additional effect on reduction of astigmatism.
Nichasin et al. [4] recommended that the proper incision depth for LRIs is approximately 90 percent of the thinnest corneal depth around the limbus. The cutting depth of an empiric blade is commonly set to 600 µm [4]. Considering that patients have variable corneal thicknesses, a fixed cutting depth of 600 µm does not appear reasonable. We, therefore, adjusted the cutting depth according to the preoperative corneal thickness. Additionally, using a 90 percent cutting depth carries a risk of corneal perforation, although the effect is maximal. Our results showed that a cutting depth of less than 90 percent achieved an acceptable correction effect on the astigmatism.
Interestingly, the single LRI procedure showed a comparable reduction on astigmatism to the paired LRIs when combined with corneal incision for cataract surgery. It appears that the corneal incision can play a coupling role with an opposite vertical keratotomy in correcting astigmatism. Because the corneal incision for cataract surgery is a penetrating wound, it appears to have a compensatory effect that mimics the effect of a second limbal incision on the same side, resulting in similar effects as performing paired LRIs.
Also, asymmetrical incisions (e.g. single LRI) have a higher coupling ratio than symmetrical incisions (e.g. paired LRIs) [18]. However, performing the single LRI with CCI can result in a more symmetrical incision than making a paired LRI with a CCI. Symmetrical incisions can induce a greater steepening effect perpendicular to the incision axis than asymmetrical incisions. Based on the results of our study, we infer that performing the single LRI with CCI appears to produce similar effects to performing the paired LRI with CCI. When you consider that the unstable wound created by performing a vertical cut can make the paired LRI procedure more difficult for the surgeon, performing the single LRI combined with a clear corneal incision appears to be a reasonable alternative that facilitates the surgical procedure.
Budak et al. [15] reported that regression in astigmatic correction mostly occurs in eyes with more than 3.5 D of astigmatism and between the first and third postoperative months. Bayramlar et al. [16] reported that astigmatic correction of LRIs stabilized in a few days and lasted over the long term. There was no such regression in eyes with high astigmatism in the Bayramlar study. Although our study is limited by its small sample size and short term follow-up period, it appears to have been worthwhile to examine the value of performing a single LRI in cataract surgery. Because of the general regression trend for corneal incisions in cataract surgery and of LRIs for lower astigmatism (less than 3 D), long term regression appears less likely to occur.
In conclusion, limbal relaxing incisions showed about a 50 percent reduction effect on the mean refractive astigmatism when combined with phacoemulsification, while performing a single LRI demonstrated comparable reduction effects to performing paired LRIs.
Figures and Tables
Fig. 1
Topography examination of one patient who underwent a single limbal relaxing incision with clear corneal incision, preoperative and postoperative one-month.
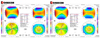
Fig. 2
Topography examination of one patient who underwent double limbal relaxing incisions with clear corneal incision, preoperative and postoperative one-month.

References
1. Budak K, Friedman NJ, Koch DD. Limbal relaxing incisions with cataract surgery. J Cataract Refract Surg. 1998. 24:503–508.
2. Müller-Jensen K, Fischer P, Siepe U. Limbal relaxing incisions to correct astigmatism in clear corneal cataract surgery. J Refract Surg. 1999. 15:586–589.
3. Gills JP, Gayton JL. Gills JP, Fenzl R, Martin RG, editors. Reducing pre-existing astigmatism. Cataract surgery: the state of the art. 1998. Thorofare (NJ): Slack;53–66.
4. Nichamin LD. Astigmatism control. Ophthalmol Clin North Am. 2006. 19:485–493.
5. Kaufmann C, Peter J, Ooi K, et al. Limbal relaxing incisions versus on-axis incisions to reduce corneal astigmatism at the time of cataract surgery. J Cataract Refract Surg. 2005. 31:2261–2265.
6. Langerman DW. Architectural design of a self-sealing corneal tunnel, single-hinge incision. J Cataract Refract Surg. 1994. 20:84–88.
7. Naeser K, Behrens JK, Naeser EV. Quantitative assessment of corneal astigmatic surgery: expanding the polar values concept. J Cataract Refract Surg. 1994. 20:162–168.
8. Argento C, Mendy JF, Cosentino MJ. Laser in situ keratomileusis versus arcuate keratotomy to treat astigmatism. J Cataract Refract Surg. 1999. 25:374–382.
9. Cherry PM. Treatment of astigmatism associated with myopia or hyperopia with the holmium laser: second year follow-up. Ophthalmic Surg Lasers. 1996. 27:S493–S498.
10. Condon PI, Mulhern M, Fulcher T, et al. Laser intrastromal keratomileusis for high myopia and myopic astigmatism. Br J Ophthalmol. 1997. 81:199–206.
11. Kremer FB, Dufek M. Excimer laser in situ keratomileusis. J Refract Surg. 1995. 11:S244–S247.
12. Agapitos PJ, Lindstrom RL, Williams PA, Sanders DR. Analysis of astigmatic keratotomy. J Cataract Refract Surg. 1989. 15:13–18.
13. Güell JL, Vazquez M. Correction of high astigmatism with astigmatic keratotomy combined with laser in situ keratomileusis. J Cataract Refract Surg. 2000. 26:960–966.
14. Ganem S, Sidhoum SB. Surgery in myopic astigmatism: arciform keratotomy and PKR versus PARK. Bull Soc Belge Ophtalmol. 1997. 266:87–90.
15. Budak K, Yılmaz G, Aslan BS, Duman S. Limbal relaxing incisions in congenital astigmatism: 6 month follow-up. J Cataract Refract Surg. 2001. 27:715–719.
16. Bayramlar HH, Dağlioğlu MC, Borazan M. Limbal relaxing incisions for primary mixed astigmatism and mixed astigmatism after cataract surgery. J Cataract Refract Surg. 2003. 29:723–728.
17. Carvalho MJ, Suzuki SH, Freitas LL, et al. Limbal relaxing incisions to correct corneal astigmatism during phacoemulsification. J Refract Surg. 2007. 23:499–504.
18. Gills JP, Rowsey JJ. Managing coupling in secondary astigmatic keratotomy. Int Ophthalmol Clin. 2003. 43:29–41.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download