Abstract
Purpose
Several articles have been published on the successful elimination of iridolenticular synechiae after cataract extraction with a neodymium YAG laser (Nd:YAG laser) and surgical synechiolysis during cataract surgery, but the indications recommending which method is proper to use for specific kinds of adhesions have not yet been established.
Methods
We retrospectively reviewed the medical records of 106 patients who had undergone Nd:YAG laser or surgical synechiolysis between January 2002 and December 2007 in our clinic. Laser synechiolysis was performed in the synechiae not exceeding the extent of one clock hour and reaching only to the iris sphincter, whereas surgical synechiolysis was performed in other diffuse and/or thick synechiae.
Results
Surgical synechiolysis was performed in 93 eyes, and YAG laser synechiolysis was done in 21 eyes. Increases in best-corrected visual acuity (BCVA) were observed in 61 eyes (53.51%). Intraocular pressure spikes after the procedure were present in only 4 eyes, and all of them were transient except for 1 eye, which needed additional glaucoma eyedrops.
Iridocapsular adhesion after cataract surgery can cause pupil contour change associated with functionally significant glare for the patient, decreased focal depth, some decreased visual acuity, and the release of potential inflammatory mediators, which are the suspected source of cystoid macular edema.
Some articles have been published on the successful elimination of such synechiae with neodymium YAG laser (Nd:YAG laser)1-3 or neodymium YLF laser (Nd:YLF laser)4 and surgical synechiolysis during cataract surgery,5-7 but the indications recommending which method is proper to use in specific kinds of iridocapsular adhesions after cataract surgery have not been established yet.
With a new guideline, we successfully achieved the elimination of iridocapsular adhesion with minimal complications.
We retrospectively reviewed the medical records of 106 patients who had undergone Nd:YAG laser or surgical synechiolysis after cataract extraction between January 2002 and December 2007 in our clinic. Synechiolysis was done in eyes in which pharmacological dilation or miosis was not effective to destruct the adhesions and also in eyes with synechiae causing a dragged or distorted pupil resulting in an impaired normal light reflex, photophobia, diplopia, and in those with cystoid macular edema. Patients who had undergone phacoemulsification and intraocular lens implantation, a triple operation (combined cataract surgery and trabeculectomy), or a combined procedure with pars plana vitrectomy and cataract surgery with or without intraocular gas or oil injection, with or without Ahmed valve implantation were eligible. Excluded were those who had undergone surgery due to penetrating ocular trauma or endophthalmitis, combined surgery with extraocular buckling, and those without an intraocular lens. Patients who had undergone any kind of procedure like posterior subtenon injection, intravitreal triamcinolone injection done simultaneously with the synechiolysis or within one month of it were not included in this study (Table 1). Synechiolysis was delayed in the eyes with intraocular gas tamponade to minimize re-adhesion until the gas completely disappeared.
We defined focal synechiae as iridocapsular adhesions not exceeding one clock hour. Thin synechiae are the iridocapsular adhesions that reach only to the iris sphincter and are stretched with pupillary dilation. The pupil was dilatated with 1% tropicamide and 2.5% phenylephrine before the synechiolysis. The Nd:YAG laser was applied to the focal and thin synechiae using between 0.6 and 1.5 millijoules. The laser beam was targeted adjacent to the lens capsule to minimize iris pigment dispersion and hemorrhaging from the iris. Diffuse synechiae were determined to be the adhesions exceeding one clock hour, and thick synechiae were the iridocapsular adhesions including the iris stroma. Surgical synechiolysis was done in such diffuse and/or thick synechiae with a synechiolysis spatula through a small paracentesis wound placed at the limbus under the surgical microscope and under topical anesthesia (Fig. 1). Irrigation of the anterior chamber with balanced salt solution (BSS®) was followed through the wound in all cases to wash out dispersed iris pigments and possible microhemorrhages and to set proper intraocular pressure. Pharmacologic miosis with 1% miochol was performed as needed on a case-by-case basis to prevent re-adhesion. In cases of poor pupil dilation with or without large capsulorrhexis, 2% pilocarpine eyedrops were prescribed four times a day, whereas in small capsulorrhexis, 1% tropicamide eyedrops were recommended twice a day. Miotic or mydriatic eyedrops were used for up to two weeks postoperatively.
After the procedure, intraocular pressure was measured in one hour with a Goldmann applanation tonometer. One drop of 0.15% brimonidine (Alphagan®) was instilled when intraocular pressure was less than 25 mmHg, and glaucoma eyedrops were prescribed if the patients had preexisting glaucoma and/or an intraocular pressure of 25 mmHg or more.
Patients were followed-up at three days, one week, two weeks, one month, three months, and six months postoperatively. The best-corrected visual acuity (BCVA) was checked on the day of synechiolysis and one month after the procedure to identify any improvements. In cases with recurrence of adhesion, synechiolysis was repeated, and BCVA was checked one month after the last procedure.
The average age of the 106 patients was 58.25±10.90 years. The age and sex distributions of the patients with known diabetes and hypertension are described in Table 2. Surgical synechiolysis was performed in 93 eyes, and YAG laser synechiolysis was done in 21 eyes (Fig. 2). Uveitis was present in 7 eyes of 7 patients. Among the 114 eyes, pars plana vitrectomy was preceded in 86 eyes with intraocular gas injection in 78 eyes, silicone oil injection in 3 eyes, and Ahmed valve implantation in 1 eye. Cataract surgery was done in 20 eyes, and a triple surgery was performed on 8 eyes (Table 3). The most common cause for the vitrectomy was vitreous hemorrhage and/or tractional retinal detachment associated with proliferative diabetic retinopathy, followed by retinal vein occlusion, rhegmatogenous retinal detachment, diabetic macular edema, and epiretinal membrane and macular holes (Table 4).
One month later, an increase in BCVA was observed in 61 eyes (53.51%). There were recurrences of synechiae in 19 eyes (16.67%), and synechiolysis was performed using the same method twice in 13 eyes, 3 times in 3 eyes, and 4 times in 3 eyes. Among them, synechiolysis was performed with a laser repeatedly in 3 eyes that had received the same procedure before and showed no recurrence after the repeated procedures. Intraocular pressure spikes after the procedure were present in only 4 eyes, and all of them were transient except for one patient who had preexisting open angle glaucoma and needed additional glaucoma eyedrops after the surgical synechiolysis.
There is general agreement that there is some improvement in visual acuity with the destruction of the iridolenticular adhesions after cataract extraction.2-4 Some complications such as microhemorrhaging, pigment dispersal in the anterior chamber, and elevation of intraocular pressure are usually self-limiting.2-4 In order to minimize such problems and to improve the effectiveness of the procedure, we organized the indications of Nd:YAG laser synechiolysis and surgical synechiolysis. We also experienced a rise in visual acuity in more than 50% of the patients, and only 4 eyes had postoperative intraocular pressure spikes.
Focal and thin synechiae have some tensile strength when the pupil is dilated, which helps to provide stronger detachment of the iris from the capsule when the laser beam is emitted and consequently minimizes the total energy delivered. The Nd:YAG laser is successful because pigmentation of the target is not required and forceful rupture of adhesions can be achieved.8 Otherwise, iridolenticular adhesions that contain any portion of synechiae extending to the iris stroma are thick, which demands more laser energy and increases the chance of postoperative complications. Occasionally, entropion uveae (when the iris rolls back to the lens capsule) interferes with the targeting of the beam to focus at the exact area. Although surgical synechiolysis is more effective in such cases, there is more pigment dispersal, bleeding, and postoperative intraocular pressure increase in proportion to the extent of adhesions. However, irrigation of the anterior chamber with a balanced salt solution and setting the intraocular pressure through the preexisting wound helps to eliminate the dispersed pigment, debris, and hemorrhages and lowers the risks of postoperative intraocular pressure spikes.
In determining the presence of any improvement in visual acuity, we chose a time period of one month to minimize the effect of a normal recovery curve after the main operation (cataract or combined operation) and after the washout period of topical miotic and mydriatic eyedrops.
There is an increasing risk of iridocapsular adhesion following phacoemulsification surgery combined with trabeculectomy, or pars plana vitrectomy with intraocular gas tamponade because a shallow chamber can promote the formation of synechiae.
With suitable indications, laser or surgical synechiolysis can be performed safely, and a small rise in visual acuity may also be expected.
Figures and Tables
Fig. 1
Focal and thin synechiae (A) is destructed after Nd: YAG laser synechiolysis (B). Otherwise, diffuse synechiae (C) is destructed surgically (D).
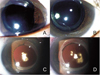
Fig. 2
Method of surgical synechiolysis. (A) A small paracentesis wound was made at the limbus. (B-C) An iridocapsular adhesion was broken by a synechiolysis spatula through the wound. (D) Irrigation of the anterior chamber with a balanced salt solution was done in all cases to wash out the dispersed iris pigment and any possible microhemorrhages and also to set proper intraocular pressure. (E) Pharmacologic miosis with miochol was performed as needed on a case-by-case basis to prevent re-adhesion. (F) Any leakage from the paracentesis wound was checked at the end of the procedure.

Table 3
Number of eyes that underwent synecholysis after each operation
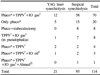
*Phaco=phacoemulsification or lens aspiration with PCL implantation in the bag; †TPPV=trans pars plana vitrectomy; ‡IO gas=intraocular tamponade with expanding gas injection; §IO oil=intraocular silicone oil injection; ‖Ahmed=Ahmed valve implantation with silicone tip insertion through the pars plana.
References
1. Kim TG, Yoo JS, Kim MH, Huh W. Clinical effect of Nd-YAG synechiolysis. J Korean Ophthalmol Soc. 1999. 40:127–132.
2. Fankhauser F, Kwasniewska S, Klapper RM. Neodymium Q-switched YAG laser lysis of iris lens synechiae. Ophthalmology. 1985. 92:790–792.
3. Kumar H, Ahuja S, Garg SP. Neodymium: YAG laser iridolenticular synechiolysis in uveitis. Ophthalmic Surg. 1994. 25:288–291.
4. Geerling G, Roider J, Schmidt-Erfurt U, et al. Initial clinical experience with the picosecond Nd:YLF laser for intraocular therapeutic applications. Br J Ophthalmol. 1998. 82:504–509.
5. Ganesh SK, Padmaja , Babu K, Biswas J. Cataract surgery in patients with Vogt-Koyanagi-Harada syndrome. J Cataract Refract Surg. 2004. 30:95–100.
6. Daus W, Schmidbauer J, Buschendorff P, et al. Results of extracapsular cataract extraction with intraocular lens implantation in eyes with uveitis and Fuchs' heterochromic iridocyclitis. Ger J Ophthalmol. 1992. 1:399–402.
7. Geerards AJ, Langerhorst CT. Pupillary membrane after cataract extraction with posterior chamber lens in glaucoma patients. Doc Ophthalmol. 1990. 75:233–237.
8. Steinert RF, Fine IH, Gimbel HV, et al. Cataract surgery. 2004. 2nd ed. Pennsylvania: Saunders;552.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download