Abstract
Purpose
To investigate the effect of lens density on liquefaction time by using liquefaction device (AquaLase®, Alcon Laboratories, TX, U.S.A.).
Methods
Cataract surgery using AquaLase® was performed on 47 eyes. With a Scheimpflug camera, the density and thickness of lens were measured in eye of each patient preoperatively. During surgery, liquefaction time and total number of pulses were recorded. The correlation of both density and thickness of lens with liquefaction time and total number of pulses was analyzed.
Results
The mean density of anterior cortex, nucleus, and posterior cortex was 112.45±42.1 computer compatible tapes (CCT), 76.5±22.7 CCT, and 70.9±52.2 CCT, respectively. The mean thickness was 0.97±0.30 mm, 2.76±0.54 mm, and 0.81±0.24 mm, respectively. The mean liquefaction time was 174.8±108.2 seconds. The mean total number of pulses was 4799±3007. There was no significant difference between the density of each area of lens (anterior cortex, nucleus, posterior cortex, and total lens) and liquefaction time (p>0.05), and between the thickness of each area of lens and liquefaction time (p>0.05). There was no significant difference between the density of each area of lens and total number of pulses (p>0.05), and between the thickness of each area of lens and total number of pulses (p>0.05).
After the development of ultrasonic phacoemulsification, its technology allows for the marked improvement of cataract surgery and the reduction of side effects that accompany conventional cataract opeartion. The improvement of visual acuity, the reduction of corneal astigmatism, and rapid visual acuity rehabilitation can be possible. However, in ultrasonic phacoemulsification, there are significant correlations between phacoemulsification time and endothelial cell loss.1 The higher is the density of the lens nucleus, the longer is phacoemulsification time, thus it has the shortcoming of increased risk of corneal endothelial cell injury when the extraction of dense cataractous lens is performed.1,2
The Scheimpflug camera which measured the density of lens is a devise imaging the anterior segment applying the Scheimpflug principle. Its imaging procedure is simple. Its objectivity and reproducibility are excellent. With Scheimpflug camera, the thickness and the density of lens could be presented as objective value. Various tests could be performed simultaneously as well.3 Then the opaque density and the thickness of each area of lens could be recorded and compared.
The AquaLase®, recently introduced surgical device, is one of the options available for lens extraction on Infiniti Vision System (Alcon Laboratories, TX, U.S.A.). During cataract surgery, the lens was emulsified via a stream of warmed balanced salt solution that ejected at the tip. This unique working method that uses the force of the water is very different from that of conventional ultrasonic phacoemulsification.
In our study, to examine the effect of lens density on the duration of liquefaction using AquaLase®, the density of each area of the lens of cataract patient was measured by a computer using a Scheimpflug camera, and it was compared with liquefaction time that was recorded at each cataract operation.
Among patients diagnosed as cataract at St. Mary's Hospital, Catholic Universicy Medical College, from September 2005 to January 2006, 43 patients (47 eyes) whose Lens Opacities Classification System (NOCS) nuclear grade was lower than 3 were examined prospectively. The cases with the past history of glaucoma, endophthalmitis, other ocular diseases, and ocular trauma were excluded from the study.
The lens tomography was taken by using a Scheimpflug camera (EAS-1000, Nidek, Japan) before surgery. At the time of imaging, the axis was 0 degree, the slit length was 14.0 mm, flash time was 200 ws, and flash intensity was 1109, thus the imaging condition was identical. After the imaging of the lens, the images were converted to digital images, directly analysed using computerised linear scanning densitometry. Thus, the lens density of cataract using a Scheimpflug camera provided an objective value.
The regional density unit of the lens such as anterior cortex, nucleus, and posterior cortex, was presented as computer compatible tapes (CCT) in our study. On the other hand, the lens thickness was defined as the distance from the anterior surface of the lens to the posterior surface, and the thickness of the lens nucleus was defined as the distance from the anterior side of the nucleus to the posterior side (Fig. 1).
The surgery was performed by a single surgeon (C.K. Chung). All patients received topical anesthesia before surgery. A 3.0 mm clear corneal temporal incision was made and Healon® was injected. Continuous curvilinear capsulorhexis approximately 5.5 mm in diameter was created. Healon® was used to reform surgical space and protect corneal endothelium. After hydrodissection and hydrodelineation by using balanced salt solution (BSS®), cataract extraction was performed using the AquaLase®.
The pulse during surgery was 50 pulses per second (pps), vacuum was 250 mmHg, and the aspiration flow rate was 30 cc/minute. Cases that surgery was initiated by AquaLase® but switched to conventional ultrasound phacoemulsification were excluded from the study. Under such condition, the duration of liquefaction was recorded as well as the total number of pulse. The correlation of measured liquefaction time and total number of pulse to the density and thickness of each area of the lens was investigated. Statistical analysis was performed by the SPSS 13.0 for Window. By applying Pearson's correlation coefficient, the correlation of the density and thickness of each area of the lens to liquefaction time and the total pulse was compared.
According to total lens density level, all patients were divided into three groups. The first group (Group 1) consisted of 12 eyes that had lower density level (lower than total 220 CCT). Second group (Group 2) consisted of 23 eyes that had intermediate lens density (between 220 and 300 CCT). The last group (Group 3) consisted of 12 eyes that had higher lens density (higher than total 300 CCT). We also compared the mean liquefaction time among the three groups.
47 eyes in 43 patients were included in this study. The mean age of patients was 62.8±9.7 years (29-78 years). The male was 12 patients (13 eyes), and the female was 31 patients (34 eyes).
Regarding the mean density of each area of the lens measured by a Scheimpflug camera preoperatively, anterior cortex (D1), nucleus (D2), and posterior cortex (D3) were 112.45±42.1 CCT, 76.5±22.7 CCT and 70.9±52.2 CCT, respectively. The mean thicknesses of anterior cortex (T1), nucleus (T2), and posterior cortex (T3) were 0.97±0.30 mm, 2.76±0.54 mm, and 0.81±0.24 mm, respectively. The mean liquefaction time was 174.8±108.2 seconds and the mean total number of AquaLase® pulses was 4799±3007 pps.
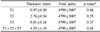
There was no statistically significant difference between the density of each area of the lens (D1, D2, D3, and total lens density) and liquefaction time (p=0.09, p=0.39, p=0.26, and p=0.35) (Table 1). There was no statistically significant difference between the thickness of each area of the lens (T1, T2, T3, and total lens thickness) and liquefaction time (p=0.25, p=0.08, p=0.38, and p=0.31) (Table 2). There was no statistically significant difference between the density of each area of the lens (D1, D2, D3, and total lens density) and total number of AquaLase® pulses (p=0.54, p=0.55, p=0.74, and p=0.51) (Table 3). There was no statistically significant difference between the thickness of each area of the lens (T1, T2, T3, and total lens thickness) and total number of AquaLase® pulses (p=0.68, p=0.55, p=0.37, and p=0.45) (Table 4).
The liquefaction times of Group 1, Group 2 and Group 3, which were created according to lens density level, were 171.5±113.8 second, 188.1±117.6 second, and 169.8±71.7 second, respectively. The total number of AquaLase® pulses was 4605±2820 pps, 5082±3255 pps, and 4363±2379 pps, respectively. There was no statistically significant difference of liquefaction time and total number of pulses among the three groups (p=0.54 and p=0.55) (Table 5).
AquaLase® is a new surgical method of nuclear removal by the utilization of the water force during cataract surgery. In comparison with ultrasonic phacoemulsification which has been used widely, AquaLase® has some proposed advantages, including reduced posterior capsule rupture and thermal injury to corneal endothelium and corneal Incision site.4
AquaLase® warms balanced salt solution to 57℃ and works by propelling short pulses of heated balanced salt solution, maximum rate of 50 Hz, which liquefies lens material. The effect of AquaLase® is two parts: far-field and near field. In case of near field effect, sufficient fluid pulse energy inside aspiration port is delivered to liquefy the lens nucleus. Far-field effect is distal to the tip and creates delamination of nuclear material.
As shown in our study, AquaLase® was very effective for removal of soft to moderate density cataract in which Lens Opacities Classification System (LOCS) nuclear grade was lower than 3. Mackool RJ and Brint SF4 reported their experience for dense nucleus removal using AquaLase®. In their case, it was not as effective as conventional ultrasound phacoemulsification. We also experienced that cataract surgery was switched from AquaLase® to conventional ultrasound phacoemulsification in 4 patients, who were excluded in our study. The mean density of the lens nucleus for 4 eyes was 149.7±25.5 CCT, which was much higher than the mean density of all participants in our study, 76.5±22.7 CCT. Although this is very subjective, 4 cases with higher nucleosclerosis were felt to be more difficult with AquaLase® than they would be with ultrasound phacoemulsification.
During cataract surgery using conventional ultrasound phacoemulsification, higher is the density of nuclues, longer is phacoemulsification time. Then, more corneal endothelial cell loss occurs.2 Therefore it is always recommended that short duration of ultrasound phacoemulsification should be applied as much as possible.5 However, our study found that the density of the lens nucleus did not have an effect on the duration of liquefaction using AquaLase® in soft to moderate cataract whose LOCS nuclear grade was lower than 3 and the total lens density also did not cause the increase of liquefaction time. Moreover, even if the density level of the lens was elevated, the amount of total AquaLase® pulse was not increased. We propose possible reasons that liquefaction time does not correlate to lens density in soft to moderate cataract. One is that AquaLase® uses a fundamentally different technology from the action of conventional ultrasound phacoemulsification. AquaLase® liquefies lens material through the action of fluid pulses. Another is that AquaLase® easily extracts cataract of soft and moderate density. Our study consists of cataract patients with soft and moderate density. The last one is that cataract with soft and moderate lens density may not be associated with the liquefaction time and AquaLase® pulse.
When extractions of cataract were performed with AquaLase® on 47 eyes, no posterior capsule rupture occurred in our study, as suggested in other report that AquaLase® less likely causes posterior capsule rupture than conventional ultrasound phaco-emulsification tip.4 The smooth polymer tip of AquaLase® is capable of reducing the rate of rupturing of the capsule when the vacuum causes occlusion of the tip by capsule. Thermal injury of corneal incision site was not shown on all 47 eyes.
Other serious complications were not developed and good surgery outcome was obtained without special complications in most case. After surgery, in 2 eyes, the temporary elevation of ocular pressure was detected, and in 1 eye, severe inflammatory reaction in the anterior chamber was shown but it was recovered immediately at the next follow-up. In 4 eyes that were not included in our study, the liquefaction of the lens nucleus could not performed readily, and thus the surgery was continued by switching to phacoemulsification using ultrasound, and special complications did not occur during surgery. In one case, zonulolysis was developed. That case was well managed after converting liquefaction to ultracound phacoemulsification. At 2 months after surgery, severe posterior capsule opacification was detected in that case.
When the extraction of soft to moderate density cataract was performed with liquefaction device on 47 eyes in our study, the lens density and lens thickness didn't increase the liquefaction time and total number of AquaLase® pulses. More extensive study may demonstrate the relationship between AquaLase® cataract extraction and lens density. In the future, the development in liquefaction technology will allow more efficient removal of denser lens. For the present, AquaLase® plays a major role in soft to moderate density cataract extraction. However, this instrument seems especially stable and safe. It is certain that it is likely to become one of indispensable surgical tools.
Figures and Tables
Fig. 1
Schematic view of lens. D1=the density of anterior portion of lens cortex; D2=the density of lens nucleus; D3=the density of posterior portion of lens cortex; T1=the thickness of anterior portion of lens cortex; T2=the thickness of lens nucleus; T3=the thickness of posterior portion of lens cortex.

Table 1
Correlation between the density of each area of the lens and liquefaction time using AquaLase® (Mean±S.D.)

Table 2
Correlation between the thickness of each area of the lens and liquefaction time using AquaLase® (Mean±S.D.)
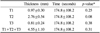
Table 3
Correlation between the density of each area of the lens and total number of AquaLase® pulses (Mean±S.D.)
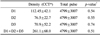
Table 4
Correlation between the thickness of each area of the lens and total number of AquaLase® pulses (Mean±S.D.)
References
1. Dick HB, Kohnen T, Jacobi FK, Jacobi KW. Long-term endothelial cell loss following phacoemulsification through a temporal clear corneal incision. J Cataract Refract Surg. 1996. 22:63–71.
2. Hayashi K, Hayashi H, Nakao F, Hayashi F. Risk factors for corneal endothelial injury during phacoemulsification. J Cataract Refract Surg. 1996. 20:1079–1084.
3. Qian W, Sodenberg P, Chen E, Philipson B. Universal opacity standard for Scheimpflug photography. Ophthalmic Res. 2000. 32:292–298.
4. Mackool RJ, Brint SF. AquaLase : a new technology for cataract extraction. Curr Opin Ophthalmol. 2004. 15:40–43.
5. Ogino K, Koda F, Miyaki K. Damage to cultured corneal endothelium caused by ultrasound during phacoemulsification. Nippon Ganka Gakkai Zasshi. 1993. 97:1286–1291.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download