Abstract
Purpose
To compare the surgical outcomes between bilateral lateral rectus muscles (BLR) re-recession and bilateral medial rectus muscles (BMR) resection in recurrent exotropia.
Methods
The medical records of patients with recurrent exotropia who underwent surgery for intermittent exotropia during the 6 years from January 2001 to December 2006 and followed up for more than 6 months were reviewed retrospectively.
Results
In group A, BLR recessions was performed at the first surgery and BLR re-recession was performed at the second surgery. In group B, BLR recession was performed at the first surgery and BMR resection at the second surgery. Success rates at the last follow-up after the second operation were 81.9% in Group A and 83.3% in Group B, showing no statical difference between the two groups. In group A, no significant underaction of the BLR was noted. Success rates were not statistically different between the 2 mm re-recessed subgroup and 3 mm re-recessed subgroup.
The purpose of strabismus surgery is to realign the deviated eyeball. However, regardless of the application of the best surgical technique, strabismus always has a possibility to require resurgery.1 After surgery, in cases with recurrent exotropia with time, if diplopia were developed, for the cases whose binocular vision could not be maintained or the deviation were severe to the level that strabismus were shown in appearance, resurgery is required.2
For exotropia surgery, bilateral lateral rectus muscles recession or unilateral recession and resection has been generally used.3 Upon recurrence of exotropia, surgical procedure of resurgery is determined depending on the first surgery procedure.4 The patients who had bilateral lateral rectus muscles recession for the first surgery, primarily, medial rectus muscle resection is applied for the second surgery, and although rare, lateral rectus muscles re-recession may be performed.4 Lateral rectus muscles re-recession has the advantage that unoperated muscles could be conserved maximally. Nevertheless, reports on the re-recession amount is rare, therefore, after excessive lateral rectus muscles re-recession, abduction impairment of the rectus muscles may be induced.
We compared the surgical outcome of patients who had bilateral lateral rectus muscles re-recession with patients who had bilateral medial rectus muscles resection for exotropia recurred after the first bilateral lateral rectus muscles recession surgery, and assessed the successful re-recession amount for procedure.
The medical records of patients with recurrent exotropia who underwent surgery for intermittent exotropia from January 2001 to December 2006 and followed up for more than 6 months were examined retrospectively. Patients with congenital exotropia, sensory exotropia or paralytic strabismus, patients with systemic diseases that may cause the impairment of the extraocular muscle, and other ophthalmic anomalies were excluded from the study.
A total of 23, patients received the second surgery for recurrent exotropia after the first surgery for intermittent exotropia during this research period. All 23 patients had received previous bilateral lateral rectus muscles recession. The subjects were divided into patients who received bilateral lateral rectus muscles re-recession (A group, 11 patients) (Table 1) and patients who received bilateral medial rectus muscles resection (B group, 12 patients) (Table 2) as the second surgery, and their surgical outcome was compared.
The angle of deviation was measured after the correction of refractive error by the alternate prism cover test at 6 m and at 33 cm distance. The recurrence was defined as that after surgery, at the test performed at the outpatient clinic, orthophoria or the deviation less than 8 prism diopter (PD) at distance and near was shown, and subsequently, the exotropic deviation angle increased and became exotropia greater than 8PD. All surgeries were performed by one surgeon. At the resurgery, the surgery amount was determined considering the bilateral lateral rectus muscles recession amount of the first surgery at the A group, and according to the Parks' table at the B group.5 Regarding resurgery techniques, patients whose primary recession amount was greater than 7.0 mm received bilateral medial rectus muscles resection because re-recession may cause limitation of abduction. Among the group who received bilateral lateral rectus muscles re-recession, if the amount of recession for the first surgery was 7.0 mm, for example for about 20 PD exotropia patients, 2.0 mm re-recession was performed, and if the recession amount was less than 7.0 mm in the first surgery, 3.0 mm re-recession was performed.
The follow up observation was performed at one day, 1 week, 1 month, and 6 months after surgery, and afterward, at 1 year intervals. At 1 day and at 1 week after surgery, the limitation of eyeball movement was examined. Orthophoria at distance and near and the deviation less than 8PD at the last visit was defined as successful surgery.
The statistical significance of surgery outcome was analyzed by the SPSS 12.0 statistics program. Between the two groups, the age prior to surgery, the deviation angle prior to surgery, the follow up observation period, etc. were analyzed by Mann-Whitney U test, and the final success rate after the second surgery and the success rate according to the re-recession amount were analyzed by Fisher's exact test.
Twenty-three patients received the second surgery for recurrent exotropia after bilateral lateral rectus muscles recession. Twelve were male (52.2%), and 11 were female patients (47.8%), and the ratio of male to female was comparable.
At the time of the first surgery, the average age of the A group was 7.7±3.5 years, the B group was 6.9±3.0 years, and a significant difference was not detected (p=0.775). The average deviation angle at the distal distance of the A group was 25±4.4PD (18-32PD) and the B group was 29±6.8PD (20-40PD), and at the proximal distance, the A group was 29±6.5PD (18-35PD) and the B group was 35±7.0PD (25-45PD), and a significant difference between the two groups was not detected both at distance and near (p=0.058, p=0.057). The interval from the first surgery to the time the second surgery was performed for recurrent exotropia of the A group was average 25.8±11.9 months (6-72 months) and the B group was 18.1±10.1 months (6-38 months), and the difference was not statistically significant (p=0.643). At the time of the second surgery, the average deviation angle at the distal distance of the A group was 20±3.5PD (18-24PD) and the B group was 21±3.7PD (18-25PD), and at the proximal distance of the A group was 23±2.0PD (18-25PD) and the B group was 24±3.1PD (20-30PD), and a significant difference between the two groups was not detected (p=0.165, p=0.138). The follow up period after the second surgery of the A group was 11.5±6.4 months (6-24 months) and the B group was 9.0±4.8 months (6-20 months), a difference between the two groups was not detected (p=0.260).
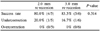
At the last visit after the second surgery, the success rate of the A group was 81.9%, the B group was 83.3%, and the surgery success rate of the two groups was not different (p=0.671)(Table 3). In all cases of the A group, limitation of abduction was not detected.
Among the 11 cases of the A group, between the patient group with 2.0 mm re-recession amount and the patient group with 3.0 mm re-recession amount, a difference of the surgery success rate was not detected (p=0.314) (Table 4).
The success rate and recurrence rate of exotropia surgery have been reported diversely in each study because the standard of surgery success and the follow up period were different. Choi and Kim5 have reported 22.4% under-correction or the recurrence of exotropia after the average 16.6 months follow up observation, Kim and Cho6 have reported 36% recurrence rate in the average 21 months follow up observation of 180 patients. Stoller et al.7 have reported 31.6% undercorrection or recurrence in a study on 57 patients, Richard and Parks8 have reported 38% undercorrection or recurrence after 2-8 years follow up observation.
Because strabismus is not simply a mechanical problem, but a problem developed by the combination of the nervous system and the sensory system, even in intermittent exotropia cases, regardless of the choice of surgery techniques, a tendency of the deviation becoming exotropia, in other words, recurrence has been reported with the increase of the follow up period after surgery.9
Therefore, at the time of the first surgery, the possibility of the second surgery is considered simultaneously, and upon its recurrence, the second surgery technique is chosen depending on the surgical technique of the first surgery. If unilateral lateral rectus muscle recession and medial rectus muscle resection were performed as the first surgery, as the second surgery, the identical procedures are performed on the opposite eye, and for the cases which underwent bilateral lateral rectus muscles recession as the first surgery, as the second surgery, bilateral medial rectus muscles resection is performed in many cases.2
Among those patients whose exotropia recurred after the surgical treatment of intermittent exotropia, and who underwent the second surgery and were available for longer than 6 months follow ups, we compared the surgery success rate at the last follow up of 11 patients of the A group who underwent bilateral lateral rectus muscles recession as the first surgery and bilateral lateral rectus muscles re-recession as the second surgery with 12 patients of the B group who underwent bilateral lateral rectus muscles recession as the first surgery and bilateral medial rectus muscles resection as the second surgery. The success rate after the second surgery was 81.9% and 83.3%, respectively, similar to the result of 81% reported by Hardesty et al.10 and 82% reported by Richard and Parks8, and thus it could be confirmed that regardless of surgical techniques, the surgery success rate of recurrent exotropia was good. Nevertheless, the follow up observation period of our study was shorter than the two studies, and if long term observations were performed, the surgery success rate may be lowered.
Reports on lateral rectus muscle re-recession performed on recurrent exotropia patients are very rare. Yazdian and Ghiassi11 have reported that in recurrent exotropia patients, average 2.0-4.0 mm bilateral lateral rectus muscles re-recession was performed less than 17.0 mm from the limbus and the surgery was successful in 100%. In our study, based on the exodeviation about 20 prism diopter, for the case which had 7.0 mm recession at the first surgery, 2.0 mm re-recession was performed, and for the cases with the recession amount less than 7.0 mm, 3.0 mm re-recession was performed, and the total recession amount of all 11 patients in the A group was within 16.0 mm from the limbus area. Lateral rectus muscle re-recession showed a success rate comparable with medial rectus muscle resection without limitation of abduction, and regarding the success rate according to the re-recession amount, a significant difference between the group performed 2.0 mm re-recession and the group performed 3.0 mm re-recession was not detected. Thus, in re-recessions performed considering the recession amount of the first surgery a good surgery outcome without the limitation of abduction of lateral rectus muscle may be anticipated. Our study is meaningful in that we were able to provide the information on the re-recession amount without limitation of abduction, and the advantage of re-recession which could conserve unoperated muscles maximally.
However, our recurrent exodeviation range is localized from 18PD to 28PD and the number of subject patients was small. Also, although the follow up observation period from the first surgery to the second surgery was long, the follow up period after the second surgery was relatively short, which could be considered to be a shortcoming of our study. To overcome such limitations, studies on a larger number of patients and long term follow ups are required.
Figures and Tables
Table 3
Final success rate after the second surgery

Success: deviation less than 8PD esodeviation or 8PD exodeviation; Undercorrection: exodeviation ≧8PD; Over-correction: esodeviation ≧8PD.
Group A: Bilateral lateral rectus muscles recession at first operation and bilateral lateral rectus muscles re-recession at second surgery, Group B: Bilateral lateral rectus muscles recession at first operation and bilateral medial rectus muscles resection at second surgery.
References
1. Howard ME, Philip K. Management of reoperations in strabismus surgery. Ann Ophthalmol. 1986. 18:70–73.
2. Park HY, Yoo MH, Choi DG. Comparision of surgical results between unilateral recession-resection and bilateral resections in recurrent exotropia. J Korean Ophthalmol Soc. 2006. 47:148–153.
3. Burian HM, Spivey BE. The surgical management of exodeviations. Am J Ophthalmol. 1965. 59:603–620.
4. Kim SJ, Choi DG. The clinical analysis after reoperation for recurrent intermittent exotropia. J Korean Ophthalmol Soc. 2007. 48:321–327.
5. Choi DG, Kim PS. The surgical outcome of intermittent exotropia and the prognostic factors. J Korean Ophthalmol Soc. 1998. 39:1255–1263.
6. Kim MM, Cho ST. Long-term surgical results of intermittent exotropia. J Korean Ophthalmol Soc. 1994. 35:1321–1326.
7. Stoller HS, Simon JW, Lininger LL. Bilateral lateral rectus recession for exotropia; A survival analysis. J Pediatr Ophthalmol Strabismus. 1994. 31:89–92.
8. Richard JM, Parks MM. Intermittent exotropia-surgical results in different age groups. Ophthalmology. 1983. 90:1172–1177.
9. Chang BL. Operative results in exotropia. J Korean Ophthalmol Soc. 1983. 24:729–734.
10. Hardesty HH, Boynton JR, Keenan JP. Treatment of intermittent exotropia. Arch Ophthalmol. 1978. 96:268–274.
11. Yazdian Z, Ghiassi G. Re-recession of the lateral rectus muscles in patients with recurrent exotropia. J AAPOS. 2006. 10:164–167.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download