Abstract
Purpose
To evaluate long-term visual outcome of arteriovenous adventitial sheathotomy in BRVO-induced macular edema.
Methods
The visual outcomes of 8 patients following vitrectomy with arteriovenous adventitial sheathotomy for BVO-induced macular edema (surgery group) were retrospectively evaluated. The three year post-operative visual acuity of the surgery group was compared with that of the conservatively managed controls.
Results
All patients were followed for a minimum of 36 months. Mean BCVA (logMAR) in the surgery group changed from 1.10± 0.34 to 1.19±0.70 and to 0.80±0.36 at 12 and 36 months, respectively (p=0.959 at 12 months, p=0.018 at 36 months). In the control group, visual acuity improved from 1.15±0.43 to 0.43±0.44 and to 0.43±0.39 at 12 and 36 months, respectively (p=0.015 at 12 months, at p=0.003 at 36 months). A strong trend toward better visual acuity at 12 months and final examination was observed for controls. (surgery vs. control group, p=0.052 at 12 months, p=0.066 at 36 months).
Branch retinal vein occlusion (BRVO) is the second most common retinal vascular disease. BRVO can lead to visual loss from retinal hemorrhage, macular edema, and macular ischemia. Although BRVO has a relatively favorable visual prognosis, with approximately 50% of patients achieving 20/50 and reasonable final visual acuity, some patients' acuities worsen. Previous reports suggest that poor initial acuity, macular ischemia, and foveal avascular zone breakdown predict poor outcome.1,2 However, there is controversy regarding the etiology of poor outcome.
The branch vein occlusion study showed that argon laser macular photocoagulation benefits those with macular edema lasting longer than 3 months prior to treatment, foveal avascular zone preservation, and no macular hemorrhage.3 However, most patients had initial acuities between 20/40 and 20/100, and very few patients with severe visual loss were enrolled. Therefore, alternative treatments for BRVO patients with poor initial acuity are needed.
BRVO is thought to be caused by vein compression at an arteriovenous crossing site. Arteries share a common arteriovenous sheath with the vein; an overlying hypertensive and atherosclerotic affected artery leads to compression, downstream venous turbulence, endothelial damage, and secondary thrombosis. Arteriovenous adventitial sheathotomy has been proposed as a direct approach to release compressive vein force and to restore venous flow. To date, surgical results show resolution of macular edema and subsequent visual improvement.4-7 However, there is some controversy regarding surgical efficacy and long-term outcome.
This study, therefore, retrospectively reviewed visual outcomes of arteriovenous adventitial sheathotomy at 3 year follow-up in patients with BRVO-induced macular edema and poor visual acuity.
A consecutive series of patients with BRVO associated decreased visual acuity from September 2002 to December 2003 were enrolled. All patients with retinal disease other than BRVO were excluded. Patients with 20/100 or worse best-corrected visual acuity (BCVA) were eligible and were followed for at least 3 years. Patients were not excluded based on fluorescein angiographic evidence of capillary nonperfusion or extensive hemorrhage involving the fovea. In addition, patients were not excluded by symptom duration or BRVO location.
All patients initially underwent complete ophthalmologic examination including BCVA, fundus photographs, and fluorescein angiography. The macular Photocoagulation Study disc areas were used to quantify ischemia size from fluorescein angiograms. Best-corrected visual acuity was measured and recorded with a decimal notation.
One surgeon performed surgical procedures. After standard pars plana vitrectomy, surgical separation of the posterior cortical vitreous from optic nerve and posterior retina was performed. The responsible arteriovenous (AV) crossing site was identified. A modified microvitreoretinal blade, bent at the tip, was used to separate the overlying artery from vein. An inner retinal incision was started between 100 and 500 µm proximal to the AV crossing. The incision was continued parallel to, and under the retinal arteriole, with gentle lifting motion, until it reached the common AV crossing sheath. Both sides of the blade were used in a side-to-side manner to incise through the arteriovenous sheath and to separate the arteriole from underlying venule. The end point was elevation of the arteriole from the underlying venule.
Patients were examined postoperatively at 1 day, 1 week, and at monthly intervals for 6 months, followed by quarterly examinations thereafter. Postoperative examinations included best corrected visual acuity, slit-lamp examination, tonometry, and fundus examination.
Patients who had 20/100 or worse initial visual acuity and did not have surgical intervention were enrolled as controls, and observed for at least 36 months. The control group was examined at monthly intervals for 6 months after diagnosis, then at intervals of 2 to 3 months.
Decimal visual acuity was converted to a logarithm of minimal angle of resolution for statistical analysis. Improvement or worsening of visual acuity in surgery group was analyzed with Wilcoxon-signed rank test. Pearson correlation coefficient was used to analyze whether visual prognosis was associated with degree of foveal ischemia, timing of surgical intervention, initial visual acuity or macular thickness. Comparisons of baseline variables, visual acuity and vision change between two groups were performed using Mann-Whitney test and Fisher's exact test. A value of p<0.05 was considered statistically significant.
Eight eyes from 8 patients with macular edema secondary to BRVO and with decreased visual acuity to 20/100 underwent vitrectomy with arteriovenous adventitial sheathotomy. All patients completed 36 months of follow-up examinations. Eight control eyes completed 36 month follow-up. Baseline variables were compared between surgery and control groups including age, gender, initial visual acuity, hypertension, BRVO location (superior or inferior), and fluorescein angiographic findings of severity of foveal ischemia. Table 1 summarizes baseline characteristics. The surgery and control group were statistically similar with respect to baseline variables.
The duration of BRVO before arteriovenous sheathotomy was between 1 and 13 months (mean±std, 3.95±3.8 Mo) in the surgery group. The arteriole was found to overlay the venule in all patients. The intraoperative surgical decompression of the arteriovenous crossing site (as defined by successful separation of the overlying arteriole from venule) was achieved in all surgical patients. Removal of internal limiting membrane was performed in all patients.
In the surgery group, vision changed from 1.10±0.34 to 1.19±0.70 at 12 months and to 0.80±0.36 at 36 months. The mean visual acuity change in logMAR between the initial and final examination was 0.30±0.28, and the final BCVA was significantly better than preoperative BCVA (p=0.018).
Timing of surgical intervention and degree of foveal ischemia were not statistically significant with respect to vision improvement (p=0.865 and p=0.686). Patients with better preoperative visual acuity had a strong trend toward better final acuity (p=0.063). In postoperative OCT at a mean of 34 months, the mean thickness of the foveal center (±SD) was 204.7±46.9 µm. However, this decrease was not accompanied with visual acuity improvement and there was no correlation between final visual acuity and foveal thickness (p=0.618).
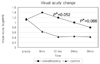
In the control group, visual acuity improved from 1.15±0.43 to 0.43±0.44 and to 0.43±0.39 at 12 and 36 months, respectively (vs. initial vision, p=0.015 at 12 months, p=0.003 at 36 months). Comparison of the surgery and control groups was performed using the mean BCVA at initial, 12 month, and final examination, and visual acuity of 20/40 or better (Table 2). Both groups were statistically similar with respect to initial visual acuity (p=0.814). However, a strong trend toward better visual acuity with the control group at 12 month and final examination was observed (surgery vs. control group, p=0.052 at 12 months, p=0.066 at 36 months) (Fig. 1). Changes in visual acuity between the initial and 36 month examination was also greater in the control group, but was not statistically significant. (surgery vs. control group, 0.30±0.28 vs. 0.72±0.47, p=0.053). At final examination, 62.5% of controls had 20/40 or better, compared with 12.5% in the surgery group (p=0.018).
Cataract developed in 7 of 8 eyes in the surgery group, and phacoemulsification with intraocular lens implantation was performed approximately 20.1 (±14.4) months after surgery.
Arteriovenous adventitial sheathotomy involving pars plana vitrectomy and AV crossing decompression is a direct approach to reopen involved venule. Osterloh and Charles.8 first performed the procedure in a patient who obtained visual improvement from 20/200 to 20/25, with progressive intraretinal hemorrhage and macular edema resolution 8 months post-operation. Since then, several studies have reported arteriovenous adventitial sheathotomy outcomes. However, there has been controversy regarding its efficacy. The primary goal of sheathotomy is to reestablish compressed venule perfusion. However, it is unclear if reperfusion decreases macular edema. Yamamoto et al.9 performed arteriovenous adventitial sheathotomy in 20 eyes and obtained reperfusion in 10 eyes. However, correlation between reperfusion and macular edema or visual acuity improvement was not established. In addition, surgical separation of the posterior vitreous cortex alone showed similar outcomes. Charbonnel et al.4 also reported that postoperative improvement in visual acuity was due to macular edema decrease and not from better blood flow.
On the other hand, a correlation between postoperative macular thickness and visual acuity was consistently reported in many studies. Garcia-Arumi et al.5 reported a significant correlation between decreased macular edema and visual acuity improvement (p<0.001, r=-0.725). Cahill et al.10 also reported that improved acuity was achieved only in eyes with resolved macular edema. In addition, it was demonstrated that intravitreal injection of triamcinolone acetonide leads to both decreased macular thickness and improved visual acuity, regardless of nonischemic or ischemic type.11 It appears that improvement in vision occurs with macular edema resolution. However, resolution does not always lead to vision improvement. In the present study, postoperative central foveal thickness at a mean of 34 months was 195.6±58.6 µm (range from 94 to 258 µm) and macular edema almost disappeared in all cases. However, this decrease was not accompanied with visual acuity improvement and OCT foveal structure was disorganized in most of the surgery group.
In a 15-patient study following arteriovenous adventitial sheathotomy, Opremcak and Bruce.12 reported that 80% had stable vision or visual improvement. Mester and Dillinger.7 performed sheathotomy on 43 patients with BRVO and used 25 patients as controls. Visual acuity improved from 0.16 to 0.35 (decimal notation), and 60% of patients achieved more than 2 lines of improvement. Yamamoto et al.9 reported that visual acuity improved from 0.53±0.35 to 0.25±0.28 (logMAR, vision improvement 0.29±0.35). Kumagai et al.13 also showed significant improvement at 31 months after sheathotomy (logMAR, improvement from 0.52±0.45 to 0.08±0.18). In the present study, visual acuity changed from 1.10±0.34 to 0.80±0.36 (at 36 month, p=0.018) and visual acuity improvement was 0.30±0.28. The final visual acuity in the present study was worse than those of other studies. However, this may be due to worse initial visual acuity. Vision improvement in our study, with an average of 0.30 logMAR of vision gained, was similar to that of study by Yamamoto et al. and in 6 of 8 eyes in the surgery group had improved vision after surgery.
With regard to surgical timing, an association between early intervention and better visual outcomes has previously been described. Mason et al.6 showed a strong trend toward improved visual outcomes with early intervention and Mester and Dillingers.7 reported that best functional improvement was observed in eyes with a shorter duration of symptoms. In the present study, timing of surgical intervention were not statistically significant with respect to vision improvement (p=0.865). However, 2 patients with symptom duration of 1 month had a tendency toward better visual outcome than patients with longer duration (vision improvement, 0.59±0.01 vs. 0.11±0.05, p=0.071). These results show that early sheathotomy may be more effective than delayed intervention. The fact that symptom duration was longer in our patients may also be another explanation for worse visual acuity than other studies. (15.8 weeks in the present study vs. 6.0 weeks in other studies).
There is conflicting evidence of an association between preoperative fluorescein angiographic findings of foveal ischemia and visual acuity outcomes. Mason et al.6 reported that foveal capillary nonperfusion and foveal ischemia severity had a statistically significant association with worsening of visual acuity. In contrast, Charbonnel et al.4 reported that eyes with preoperative retinal ischemia had more favorable outcomes than those without. In the present study, there was no significant association between the degree of macular ischemia and vision improvement.
Compared with patients in the surgery group, controls had a tendency toward better visual outcome at each time point. Cataract progressed in 7 of 8 eyes in the surgery group and cataract surgery was performed at a mean of 20 months after the operation. However, even after cataract surgery, vision remained poor in the surgery group. Although patients were not randomly assigned to treatment groups, and precise comparison between surgical intervention and natural course may not be possible, the difference in visual outcome between two groups was considerable.
Given the uncertainty of the reperfusion effect on visual improvement, the frequent complications, such as cataract progression, and the favorable natural course of BRVO, arteriovenous adventitial sheathotomy may be not a better treatment modality than conservative management in all cases. However, arteriovenous adventitial sheathotomy may be promising in selective cases. In the present study, one patient who had experienced gradual deterioration in visual acuity over 12 months before surgery achieved vision improvement from 1.16 to 0.82 (logMAR, change of 0.33) after surgery. Since the mean vision improvement of other patients in our study was 0.22±0.31, this patient's improvement was noteworthy.
This study had several limitations including a small sample size and nonrandomized treatment allocation. However, positive aspects of this study included more than three years of follow-up study, the presence of a control group, and consistent surgical technique by single surgeon.
The favorable natural course of BRVO and the unproven reperfusion effect on macular edema have created doubt regarding arteriovenous adventitial sheathotomy efficacy. Prospective randomized clinical trials are needed to determine efficacy and to evaluate indications for good surgical results.
Figures and Tables
Fig. 1
Change in visual acuity since the initial visit.
*p-value: Comparison between two groups, p=0.052 at 12 months, p=0.066 at 36 months.
References
1. Kang SJ, Chin HS, Moon YS. Visual prognosis of macular edema associated with macular ischemia in branch retinal vein occlusion. J Korean Ophthalmol Soc. 2002. 43:1621–1628.
2. Chang YH, Kim SH, Kwon OW. Risk factors and prognostic factors for branch retinal vein occlusion. J Korean Ophthalmol Soc. 2002. 41:418–426.
3. Branch Vein Occlusion Study Group. Argon laser photocoagulation for macular edema in branch vein occlusion. The Branch Vein Occlusion Study Group. Am J Ophthalmol. 1984. 98:271–282.
4. Charbonnel J, Glacet-Bernard A, Korobelnik JF, et al. Management of branch retinal vein occlusion with vitrectomy and arteriovenous adventitial sheathotomy, the possible role of surgical posterior vitreous detachment. Graefes Arch Clin Exp Ophthalmol. 2004. 242:223–228.
5. Garcia Arumi J, Martinez Castillo V, Boixadera A, et al. Management of macular edema in branch retinal vein occlusion with sheathotomy and recombinant tissue plasminogen activator. Retina. 2004. 24:530–540.
6. Mason J, Feist R, White M, et al. Sheathotomy to decompress branch retinal vein occlusion: a matched control study. Ophthalmology. 2004. 111:540–545.
7. Mester U, Dillinger P. Vitrectomy with arteriovenous decompression and internal limiting membrane dissection in branch retinal vein occlusion. Retina. 2002. 22:740–746.
8. Osterloh MD, Charles S. Surgical decompression of branch retinal vein occlusions. Arch Ophthalmol. 1988. 106:1469–1471.
9. Yamamoto S, Saito W, Yagi F, et al. Vitrectomy with or without arteriovenous adventitial sheathotomy for macular edema associated with branch retinal vein occlusion. Am J Ophthalmol. 2004. 138:907–914.
10. Cahill MT, Kaiser PK, Sears JE, Fekrat S. The effect of arteriovenous sheathotomy on cystoid macular oedema secondary to branch retinal vein occlusion. Br J Ophthalmol. 2003. 87:1329–1332.
11. Chen SD, Sundaram V, Lochhead J, Patel CK. Intravitreal triamcinolone for the treatment of ischemic macular edema associated with branch retinal vein occlusion. Am J Ophthalmol. 2006. 141:876–883.
12. Opremcak EM, Bruce RA. Surgical decompression of branch retinal vein occlusion via arteriovenous crossing sheathotomy: a prospective review of 15 cases. Retina. 1999. 19:1–5.
13. Kumagai K, Furukawa M, Ogino N, et al. Long-term outcomes of vitrectomy with or without arteriovenous sheathotomy in branch retinal vein occlusion. Retina. 2007. 27:49–54.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download