Abstract
Purpose
To report the results of secondary posterior chamber intraocular lens (PC-IOL) implantation in pediatric cataract eyes with microcornea and/or microphthalmos.
Methods
Retrospective studies were conducted by reviewing the charts of 26 eyes of 15 patients with secondary PC-IOL implantations for microcornea and/or microphthalmos associated with cataract in children between 1999 and 2002. The corneal diameter was 9.5 mm or less at the time of secondary PC-IOL implantation. Preoperative examinations were conducted for bilaterality, corneal diameter, eye abnormalities and systemic abnormalities. Postoperative results were evaluated in terms of visual developments, refractive changes, axial length measurements and the occurrence of complications. The follow-up period was at least one year after secondary PC-IOL implantation.
Results
Age at the first diagnosis for cataract with microcornea and/or microphthalmos was 2.7 months on average. Among 15 patients, 8 (53.3%) had a family history. All patients received an initial irrigation and aspiration, posterior capsulectomy, and anterior vitrectomy at 0.8 years (0.1-3.3 years) of age and a secondary PC-IOL implantation surgery at 6.7 years (1.6-17.2 years) of age on average. The postoperative follow-up period was 2.1 years (1.1-4.3 years) on average. The average power of the implanted PC-IOL was +21.2D. Postoperative complications were secondary glaucoma in two eyes, secondary pupillary membrane formation in two eyes. Best corrected visual acuities in 20 eyes in children capable of the vision test at the last follow-up were 20/60 or better in 11 eyes, 20/80 to 20/150 in eight eyes, and 20/200 or worse in one eye.
Surgical management of eyes with abnormally small corneal diameter and cataract is often complex. Intraoperative and postoperative complications are more likely to occur with cataract removal in the presence of microcornea and/or microphthalmos.1 Yu et al2 reported upon the complications of cataract surgery in severe microphthalmos with a corneal diameter of less than 9 mm, which included corneal opacity for the limbal approach and secondary membrane formation for the pars plana approach.
Posterior chamber intraocular lens (PC-IOL) implantation in pediatric cataract surgery is routinely performed.3-5 Intraoperative and postoperative complications can be reduced by microsurgical techniques and postoperative refractive changes from ocular growth can be anticipated by adjusting the target refractive power.6,7 Only a small number of studies, have reported on the application of PC-IOLs in patients with microphthalmos.8-11 Sinskey et al8 reported surgical results after primary or secondary PC-IOL implantation in 11 microphthalmic eyes with 22 months of follow-up on average. Five patients were younger than nine years and six were older than 15 years. This is not an appropriate sample of the surgical results of congenital cataract with microphthalmos, because the patients were too old. Such patients may have been diagnosed earlier during the postnatal period due to a positive family history or appearance problems. Early management is very important to ensure normal visual development in early childhood.
PC-IOL implantation in congenital cataract with microcornea and/or microphthalmos has a several drawbacks compared to that in cataractous eyes of normal size. Extremely shallow anterior chamber depth can cause an incomplete surgical manipulation and an increased incidence of complications. Moreover, there are no well-accepted guidelines for estimating intraocular lens power and no data on refractive changes on aging in these small eyeballs. This study shows the results of secondary PC-IOL implantation in congenital cataract with microcornea and/or microphthalmos with a corneal diameter of or less than 9.5 mm in children younger than 18 years.
Retrospective review was conducted on records of patients who underwent secondary PC-IOL implantation for aphakia with a corneal diameter of 9.5 mm or less between 1999 and 2002 at Seoul National University Children's Hospital. The cataract surgery was conducted by a single doctor (YS Yu) on a total of 26 eyes in 15 patients after obtaining informed consent from their parents. Patients with microphthalmos with a corneal diameter of greater than 9.5 mm, microphthalmos with anterior segment dysgenesis syndrome and posterior or combined types of persistent hyperplastic primary vitreous were excluded from this study. All patients had bilateral disease but four eyes of four patients were excluded from this study. Three of these patients underwent secondary PC-IOL implantation on both eyes but a corneal diameter of one eye was greater than 9.5 mm. One underwent secondary PC-IOL implantation surgery only on her left eye, because the contralateral eye developed a corneal opacity after bilateral primary lens surgery.
Preoperative examinations were conducted for bilaterality, corneal diameters, axial lengths, eye abnormalities and systemic abnormalities.
Corneal diameters of each eye were measured by using a caliper from white to white horizontally during lens surgery.
Primary lens surgeries were conducted using the two limbal incisions: one for an irrigation cannula and the other one for an aspiration/cutting hand piece. In every case, an anterior capsulectomy, aspiration of the lens material, posterior capsulectomy and anterior vitrectomy were conducted at one time. Following surgery, all patients' visions were corrected with glasses and amblyopia was treated with occlusion therapy, if necessary. When patients became 2 years or older, secondary PC-IOL implantations with a sulcus fixation were conducted. However, some patients who had a late cataract onset, asymmetric lens opacities, or delayed parental consent underwent late cataract surgery.
Secondary PC-IOL implantations were conducted using scleral tunnel incision superiorly. Posterior synechia of the iris were carefully separated and proliferated lens materials were completely removed. PC-IOLs were implanted into the sulcus and the scleral wound was closed with interrupt 8-0 Vicryl sutures. Polymethylmethacrylate (PMMA) one piece PC-IOLs were implanted in all eyes. Most patients received Ceeon 811B lenses (Pharmacia, USA) with 6 mm optic diameter and 12 mm total length, but some eyes with severe microcornea received Ceeon 812B lenses (Pharmacia, USA) with 5.5 mm optic diameter and 12 mm total length. Calculations to determine PC-IOL power were performed using SRK II formula.
All patients were followed up for at least one year after secondary PC-IOL implantation surgery. Postoperative results and complications were determined by measuring refraction, axial length, intraocular pressure with a noncontact tonometer, and by using a handheld slit lamp and by indirect ophthalmoscopic examinations. Vision assessment was made using a fixation pattern in nonverbal children and a Snellen acuity chart in the verbal group.
Patient demographic data is shown in the Table 1. The age at first diagnosis of cataract with microcornea and/or microphthalmos ranged from 0.2 to 11 months (mean: 2.7 months). Among 15 patients, eight (53.3%) had a family history of least one patient among siblings, parents, or grandparents. Corneal diameters ranged from 8 mm to 9.5 mm (mean: 9 mm) at the time of secondary PC-IOL implantation surgery.
Twenty-six eyes of 15 patients underwent an initial irrigation and aspiration, posterior capsulectomy, and anterior vitrectomy at an average 0.8 years (range 0.1-3.3 years) and a secondary PC-IOL implantation surgery at 6.7 years (range 1.6-17.2 years). Primary cataract surgeries were performed binocularly under the same general anesthesia with separate drapes after obtaining informed consent. The average power of the implanted PC-IOL was +21.2D. Among these, three eyes (cases nos. 8 & 15) having a small corneal diameter of 8.0 mm and 8.5 mm underwent PC-IOL implantation with small optic (5.5 mm), and five eyes of three patients (cases nos. 11, 14 & 15) having a large axial length of more than 25 mm, underwent surgery with a +9.0 or +10.0 diopters PC-IOL.
The postoperative follow-up period was 2.1 years on average (range 1.1-4.3 years). Postoperative complications included secondary glaucoma in two eyes, and secondary pupillary membrane formation in two eyes. Axial length at the last follow-up was 22 mm on average. Best corrected visual acuity in 20 eyes of children capable of vision testing at the last follow-up was 20/60 or better in 11 eyes, 20/80 to 20/150 in eight eyes, and 20/200 or worse in one eye.
Recent improvements in the methods of surgery for congenital cataracts have considerably reduced postoperative complications and improved visual outcome. Of the optical correction modalities, the implantation of a PC-IOL has recently become more common in the surgical management of cataracts in one or both eyes in patients older than two years, although significant long-term data on PC-IOL implantation in children is lacking.3-5,9
Microcornea and/or microphthalmos is not an uncommon congenital eye abnormality and is commonly accompanied by congenital cataracts.1,12,13 Microcornea is diagnosed when the corneal diameter is less than 11 mm, and can occur independently or by accompanied by microphthalmos.1 Microphthalmos is characterized by an axial length of less than 20 mm and can occur independently or be accompanied by microcornea. All cases presented in this study demonstrated microcornea with a corneal diameter ranging from 8 mm to 9.5 mm, but their axial lengths ranged from less than 20 mm to more than 24 mm. Among these, five eyes of three patients had large axial lengths, exceeding 25 mm. According to the report by Auffarth et al,14 these eyes may be defined as showing complex dysgenesis. They were implanted with PC-IOLs of +10 diopters and the final refractive results ranged from -0.5D to -4.0D. The final best corrected visions ranged from 20/40 to 20/100. In the present study, eyes with an axial length ranging from 21 mm to 23 mm had relative anterior microphthalmos. Auffarth et al14 defined the inclusion criteria for relative anterior microphthalmos as follows: horizontal corneal diameter ≤11 mm, axial length >20 mm, no visible malformation.
When microphthalmos is not too severe, the surgical method of PC-IOL implantation can be applied. Reports on PC-IOL implantation in cases of microphthalmos in an early childhood are uncommon. Specific anatomical features of microphthalmos, such as a small cornea and a very shallow anterior chamber, make PC-IOL insertion technically difficult. Moreover, it is difficult to determine the exact power of a lens.15-17 Gimbel et al.9 reported inserting PC-IOLs in microphthalmos patients with a corneal diameter of 9.43 mm and 9.61 mm and an axial length of 19.29 mm and 19.23 mm to obtain a postoperative vision of 20/20. Dahan et al17 reported that a pediatric PC-IOL may be inserted in the capsular bag in unilateral congenital and developmental cataracts except when the corneal diameter is less than 9.5 mm. And, Sinskey et al.8 reported inserting PC-IOLs secondarily in both aphakic eyes of a 2.5-year-old patient. The patient, whose record showed a family history of the condition, demonstrated microphthalmos with a 9 mm corneal diameter. They reported that the patient showed a late secondary membrane after surgery and required re-operation. According to these workers, there were no major difficulties in inserting PC-IOLs of optic diameters 6.0 mm or 6.5 mm and total lengths 13.5 mm or 14.0 mm in microphthalmos patients ranging in age from three to 15 years. In the present study, all cases except three underwent surgery, involving the insertion of PC-IOLs of optic diameter 6 mm and total length 12 mm, without major difficulty. Three eyes of corneal diameter 8.0 mm, 8.5 mm, 8.5 mm, underwent surgery PC-IOL insertion of 5.5 mm optic diameter and 12 mm total length.
A method for implanting high-power intraocular lenses into microphthalmic eyes with extremely high hyperopia has been reported. Gayton et al18 reported that a 31-year-old male with bilateral microphthalmos and cataract underwent implantations of two lenses in each eye. His calculated intraocular lens power was +46.0 diopters, and such a high-power lens could not be made by manufacturer. A +25.0 diopter lens was implanted posteriorly and a +30.0 diopter lens anteriorly. Oshika et al19 reported the implantation of two piggyback foldable acrylic intraocular lenses in 5 microphthalmic eyes with an axial length shorter than 17.0 mm. The mean power of the implanted lenses was +43.0 diopters. However, their system of lens power calculation markedly underestimated the required lens power, resulting in a hyperopic refractive error after surgery. Moreover, the benefits of in-the-bag placement of 2 foldable lenses were questionable. In the present study, no cases demonstrated a calculated intraocular lens power of greater than +30.0 diopters or an axial length of less than 17.0 mm. And the last refractive results ranged from +4.50 to -4.0 diopters, which could be managed by wearing glasses. No case presented in this study required the implantation of two lenses in one eye.
Postoperative complications of congenital cataract include, the formation of a secondary membrane, glaucoma, and retinal detachment.20-22 It is believed that the possibility of such complications is heightened in cases of congenital cataracts accompanied by microphthalmos or microcornea.23,24 In the present study, two eyes postoperatively showed secondary pupillary membrane formation, which needed YAG laser and surgical pupilloplasty. Two eyes developed secondary angle-closure glaucoma. Retinal detachment did not occur during the follow-up period.
Postoperative improvement of vision in cases involving congenital cataracts is influenced by the age at surgery.25,26 In the present study, primary lens surgery took place at 0.8 years of age and the secondary PC-IOL implantation at 6.7 years of age. This result demonstrates the poor recognition of microphthalmos with cataract in children, a problem that has yet to be resolved. Yu et al2 reported upon the surgical management of 20 eyes of bilateral congenital cataracts and severe microphthalmos of less than 9 mm in corneal diameter with either a limbal or a pars plicata incision, and demonstrated an encouraging result. Surgery was performed between 2 and 16 months of age. The degree of visual improvement in their study was much greater than in this study, presumably due to younger age at the time of intervention.
Dahan et al6 reported the younger the child at time of implantation, the greater the myopic shift. These eyes should be undercorrected, and the residual refractive error corrected by spectacles that are adjusted throughout life according to refractive development. However, IOL power calculations in pediatric cataract with microphthalmos have not been fully studied. Inatomi et al15 reported the best predicted refraction was calculated using the SRK/T formula for microphthalmos with axial lengths less than 19.0 mm. Bartke et al27 used a modified biometric formulas for cataract with microphthalmos in adulthood. They showed 94.7% had not more than 3 diopters of difference between the target and achieved refraction and produced reliable IOL power calculations. Oshika et al18 presented four formulas, which could be used to predict IOL power, but markedly underestimated the power required to achieve emmetropia by implanting two piggyback IOLs. In the present study, IOL power was calculated using the SRK II formula. The last refractions measured were in the range of ±3.0 diopters in 88% of the patients. Mean age of the patients at secondary IOL implantation surgery was 6.7 years, and their refractions continued to change with age, which contrasts with Bartke's result in patients aged 75.6 years.
This study has a number of limitations, although the data from secondary PC-IOL implantation in microcornea and/or microphthalmos with cataract, especially in children, are worth noting. The study design was retrospective and the ages of subjects at primary lens surgery and at last follow-up were not identical. Moreover, no control patients were included who had undergone lens surgery without PC-IOL implantation at the same age. These limitations, however, may not be easily solved. A statistical review was not possible in this study due to the small number of cases and to the different ages at surgery. Although postoperative complications developed in this study they were not significant. It might be expected that glaucoma and retinal detachment are more likely to develop in microphthalmic eyes than in the normal-sized eyes of children after PC-IOL implantation.21,23,24 For a clearer insight into these problems, we need more cases and longer follow-ups.
This retrospective study was undertaken to evaluate anatomical and functional outcomes in the eyes of children who underwent secondary PC-IOL implantation for cataract with microcornea and/or microphthalmos. It is hoped that our results add value to the literature upon PC-IOL implantation in children with microcornea and/or microphthalmos, which we recommend as a way of improving vision, but stress that the surgery must be conducted carefully to avoid possible complications.
Figures and Tables
Table 1
Patient demographic data
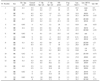
RE: right eye, LE: left eye, 1° Op: aspiration & irrigation, posterior capsulectomy, and anterior vitrectomy, 2° Op: Secondary PC-IOL implantation, 12 mm total length, BCVA: best-corrected visual acuity, csm: central, steady, maintained fixation, csum: central, steady, unmaintained fixation, cus: central, unsteady fixation.
References
1. Bateman JB. Microphthalmos. Int Ophthalmol Clin. 1984. 24:87–107.
2. Yu YS, Lee JH, Chang BL. Surgical management of congenital cataract associated with severe microphthalmos. J Cataract Refract Surg. 2000. 26:1219–1224.
3. Wilson ME. Intraocular lens implantation: has it become the standard of care for children? Ophthalmology. 1996. 103:1719–1720.
4. Hiles DA. Intraocular lens implantation in children with monocular cataracts. 1974-1983. Ophthalmology. 1984. 91:1231–1237.
5. DeVaro JM, Buckley EG, Awner S, et al. Secondary posterior chamber intraocular lens implantation in pediatric patients. Am J Ophthalmol. 1997. 123:24–30.
6. Dahan E, Drusedau MU. Choice of lens and dioptric power in pediatric pseudophakia. J Cataract Refract Surg. 1997. 23:618–623.
7. Dahan E, Salmenson BD. Pseudophakia in children; precautions, technique, and feasibility. J Cataract Refract Surg. 1990. 16:75–82.
8. Sinskey RM, Amin P, Stoppel J. Intraocualr lens implantation in microphthalmic patients. J Cataract Refract Surg. 1992. 18:480–484.
9. Gimbel HV, Basti S, Ferensowicz M, et al. Results of bilateral cataract extraction with posterior chamber intraocular lens implantation in children. Ophthalmology. 1997. 104:1737–1743.
10. Dahan E. Lens implatation in microphthalmic eyes of infants. Eur J Implant Ref Surg. 1989. 1:9–11.
11. Wilson ME, Bartholomew LR, Trivedi RH. Pediatric cataract surgery and intraocular lens implantation. Practice styles and preferences of the 2001 ASCRS and AAPOS memberships. J Cataract Refract Surg. 2003. 29:1811–1820.
12. Zeiter HJ. Congenital microphthalmos; a pedigree of four affected siblings and an additional report of forty-four sporadic cases. Am J Ophthalmol. 1963. 55:910–922.
13. Bermejo E, Martinez-Frias ML. Congenital eye malformations: clinical-epidemiological analysis of 1,124,654 consecutive births in Spain. Am J Med Genet. 1998. 75:497–504.
14. Auffarth GU, Blum M, Faller U, et al. Relative anterior microphthalmos. Morphometric analysis and its implications for cataract surgery. Ophthalmology. 2000. 107:1555–1560.
15. Gayton JL, Sanders VN. Implanting two posterior chamber intraocular lenses in a case of microphthalmos. J Cataract Refract Surg. 1993. 19:776–777.
16. Inatomi M, Ishii K, Koide R, et al. Intraocular lens power calculation for microphthalmos. J Cataract Refract Surg. 1997. 23:1208–1212.
17. Dahan E, Welsh NH, Salmenson BD. Posterior chamber implants in unilateral congenital and developmental cataracts. Eur J Implant Ref Surg. 1990. 2:295–302.
18. Gayton JL, Sanders VN. Implanting two posterior chamber intraocular lenses in a case of microphthalmos. J Cataract Refract Surg. 1993. 19:776–777.
19. Oshika T, Imamura A, Amano S, et al. Piggyback foldable intraocular lens implantation in patients with microphthalmos. J Cataract Refract Surg. 2001. 27:841–844.
20. Egbert JE, Wright MM, Dahlhauser KF, et al. A prospective study of ocular hypertension and glaucoma after pediatric cataract surgery. Ophthalmology. 1995. 102:1098–1101.
21. Desai P. Cataract surgery and retinal detachment: cause and effect? Br J Ophthalmol. 1996. 80:683–684.
22. Keech RV, Tongue AC, Scott WE. Complications after surgery for congenital and infantile cataracts. Am J Ophthalmol. 1998. 108:136–141.
23. de Sa LCF. Lens implantation in microphthalmic eyes. J Cataract Refract Surg. 1993. 19:323.
24. Parks MM, Johnson DA, Reed GW. Long-term visual results and complications in children with aphakia. A function of cataract type. Ophthalmology. 1993. 100:826–841.
25. Lambert SR, Drack AV. Infantile cataracts. Surv Ophthalmol. 1996. 40:427–458.
26. Lloyd IC, Goss-Sampson M, Jeffrey BG, et al. Neonatal cataract: aetiology, pathogenesis and management. Eye. 1992. 6:184–196.
27. Bartke TU, Auffarth GU, Uhl JC, et al. Reliability of intraocular lens power calculation after cataract surgery in patients with relative anterior microphthalmos. Graefe's Arch Clin Exp Ophthalmol. 2000. 238:138–142.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download