Abstract
Endotracheal tube damage is a well-known complication of maxillary surgery. We report a case of failure to ventilate due to superficial damage to the tubing between the cuff and pilot balloon in the nasal portion of a north facing Ring, Adair and Elwyn pre-formed endotracheal tube during Surgically Assisted Rapid Palatal Expansion surgery. The endotracheal tube was replaced uneventfully and surgery completed successfully. On reflection, we feel that that the vulnerable position of the cuff-pilot tubing significantly contributed to this critical incident and suggest that increased recognition of this is vital for the prevention of such cases in the future.
Endotracheal tube damage resulting in a failure to ventilate has been previously reported as a complication of maxillary surgery [1234567]. Several strategies have been suggested to manage such damage, but there is a dearth of literature suggesting methods for preventing such clinically significant events. We describe a case of a failure to ventilate due to endotracheal tube damage during Surgically Assisted Rapid Palatal Expansion (SARPE) surgery and suggest how an awareness of the vulnerability of cuff pilot balloon tubing could prevent such events in the future.
A 20-year-old female with transverse maxillary deficiency presented for SARPE surgery. Our preoperative airway examination did not predict an increased risk of difficult laryngoscopy and the patient was of average female height and weight. A size 6 north-facing Ring, Adair and Elwyn (RAE) endotracheal tube (Polar™ Preformed Tracheal Tube, Smiths Medical International LTD, Hythe, UK) was checked preoperatively for cuff leaks. Anaesthesia was induced and the trachea was intubated uneventfully. The patient was ventilated with a fresh gas flow of 1 L/min via a circle system, and the peak inspiratory pressure was approximately 20 cmH2O.
After about 20 minutes of operating, and during the palatal osteotomy, there was a sudden loss of minute ventilation and a complete collapse of the ventilator bellows. The fresh gas flow was increased to 15 L/min and manual ventilation was attempted unsuccessfully. Examination of the anaesthetic circuit revealed deflation of the pilot balloon, but reinflation was not possible. The damaged tube was withdrawn under direct laryngoscopy visualisation and replaced with an identical endotracheal tube uneventfully. The integrity of the circle system was confirmed by manually ventilating the patient whilst assessing the adequacy of ventilation and auscultating for leaks.
Visual inspection of the endotracheal tube revealed an approximately 9 mm incomplete incision in the nasal portion of the endotracheal tube (Fig. 1). We confirmed that damage to the tubing between the cuff and the pilot balloon was the cause for the failure to ventilate by placing a small bead of water over the cut whilst attempting to inflate the pilot balloon, which produced bubbles. Inspection of the inside of the endotracheal tube revealed a negligible internal defect.
To our knowledge, this is the first report of endotracheal tube damage during a SARPE procedure. SARPE involves surgical liberation of sites resisting palatal expansion in skeletally mature patients [8]. The sites of resistance are the piriform aperture pillars, zygomatic buttresses, pterygoid junctions and the midpalatal suture. The osteotomies required to mobilise the areas of resistance are in close proximity to the nasal cavity, and so the risk of nasal endotracheal tube damage is perhaps not surprising. Several reports of endotracheal tube damage during a closely related procedure, the LeFort 1 osteotomy, highlight this issue and also possible management strategies [1234567]. Our case demonstrates the vulnerability of the cuff-pilot tubing, and an awareness of this could help prevent cases of failure to ventilate in the future.
The vulnerability of the cuff-pilot tubing was highlighted by the fact the endotracheal tube damage was superficial and did not seem to involve the lumen, yet caused a circuit leak sufficient to impair adequate ventilation. There have been several similar cases of superficial endotracheal tube damage causing pilot balloon deflation [345]. The only case report we identified where there was clinically significant endotracheal tube damage without cuff involvement was caused by a greater than 50% transection of the lumen [1]. Conversely, a clinically insignificant 12 mm cut through the side of an endotracheal tube and into the lumen went unnoticed until extubation [7]. As such, an assertion could be made that the cuff-pilot balloon tubing is the most vulnerable part of the endotracheal tube during maxillary surgery.
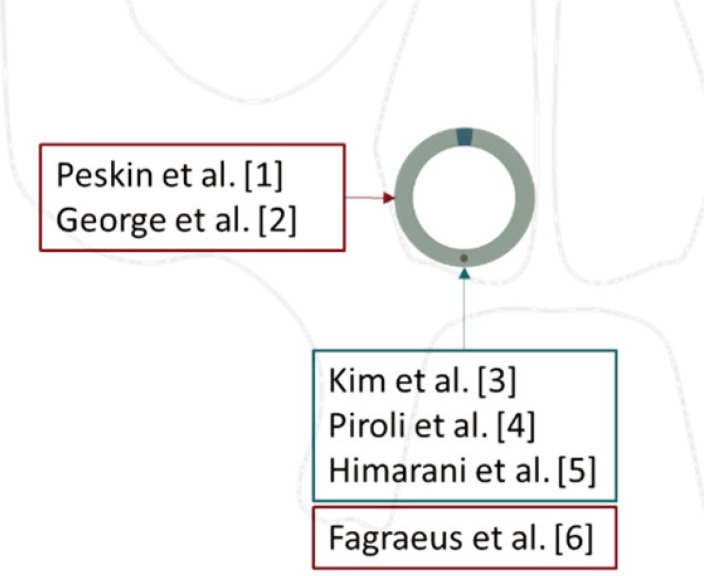
Another factor which increases the vulnerability of the cuff-pilot tubing is its location in relation to the site of surgery. The cuff-pilot tubing conventionally runs close to the palate in the inferior wall of the pre-formed endotracheal tube. Given the position of the osteotomies and that all of the case reports we identified involve either damage to the lateral or inferior aspect of the endotracheal tube, the location of the cuff-pilot tubing would appear to increase its vulnerability (Fig. 2). However, simply re-orienting the cuff-pilot tubing to the superior or medial wall of the endotracheal tube would result in a loss of the anatomical curvature. The vulnerability of the cuff-pilot balloon tubing would therefore need to be considered in the design of preformed endotracheal tubes.
In conclusion, endotracheal tube damage is a possible complication of Surgically Assisted Rapid Palatal Expansion surgery. The position of the cuff-pilot balloon puts it at a higher risk of damage, and even superficial damage can result in a failure to ventilate. We believe that both clinicians and endotracheal tube manufacturers should be aware of the vulnerability of cuff-pilot balloon tubing in order to prevent such clinically significant events in the future.
References
1. Peskin RM, Sachs SA. Intraoperative management of a partially severed endotracheal tube during orthognathic surgery. Anesth Prog. 1986; 33:247–251. PMID: 3465262.
2. George P, Fiadjoe JE, Simpao AF. An unusual lacerated tracheal tube during Le Fort surgery: literature review and case report. Case Rep Anesthesiol. 2016; 2016:6298687. PMID: 27895942.

3. Kim EJ, Yoon JY, Woo MN, Kim CH, Yoon JU, Jeon DN. Damage to the pilot balloon of the nasotracheal tube during orthognathic double-jaw surgery: A case report. J Dent Anesth Pain Med. 2015; 15:101–103. PMID: 28879266.

4. Piroli A, Cutilli T, Lupi E, Marinangeli F, Varrassi G, Paladini A. Different solutions for damaged nasotracheal tube during maxillofacial surgery: a case series. Adv Ther. 2019; 36:1812–1816. PMID: 31065994.

5. Himarani J, Nancy SM, Krishna Kumar Raja VB, Shanmuga Sundaram S. Management of an intraoperatively damaged endotracheal tube in a case of difficult airway using fibre-optic bronchoscope with minimal apnoea period. Indian J Anaesth. 2017; 61:347–349. PMID: 28515525.

6. Fagraeus L, Angelillo JC, Dolan EA. A serious anesthetic hazard during orthognathic surgery. Anesth Analg. 1980; 59:150–153. PMID: 6989286.

7. Adke M, Mendonca C. Concealed airway complication during LeFort I osteotomy. Anaesthesia. 2003; 58:294–295.

8. Bell RA. A review of maxillary expansion in relation to rate of expansion and patient's age. Am J Orthod. 1982; 81:32–37. PMID: 6758589.

Fig. 2
Location and extent of endotracheal tube damage. The grey outline represents a coronal section of the face. The circle is a transverse section of a pre-formed endotracheal tube in situ with the cuff to pilot balloon tubing within the lower border (black circle). The blue box represents studies where superficial damage to the endotracheal tube has been clinically significant due to cuff deflation. The red boxes represent the location of clinically significant damage as a result of > 50% transection.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download