INTRODUCTION
Arthrocentesis is a minimally invasive procedure that is used to alleviate the symptoms of temporomandibular joint (TMJ) disorders. It is usually the first method of treatment when there is no response to the more conservative treatment options. In the arthrocentesis procedure described by Nitzan [
1], lavage is performed by entering into the upper joint cavity of the TMJ with cannula tips to remove the inflammatory mediators, release the intra-articular adhesions, and free the articular disc [
1234].
Although arthrocentesis is considered a reliable and minimally invasive procedure, complications may occur during and/or after the procedure due to the operation site's proximity to important anatomical structures. These complications include facial paralysis, hematoma, vertigo, tinnitus, dizziness, arterial injury, and cranial injury [
567]. Ocular and ear structures, found on the anterior and posterior regions of the TMJ, respectively, are frequently affected. The majority of complications in these regions are in fact caused by the anesthetic solution applied before the arthrocentesis procedure [
58].
Anesthetic solutions can spread to the surrounding tissues and cause complications. Complications such as diplopia and mydriasis have been reported in the ophthalmic region as a result of dental anesthetics [
9]. In local anesthetic solutions, epinephrine is often added as a vasoconstrictive agent, with the aim of providing more effective anesthesia through less anesthetic reagents, thus preventing systemic toxicity which can be caused by excessive anesthetic agents. The addition of epinephrine also increases the duration and strength of the anesthesia. Furthermore, epinephrine reduces blood flow through its vasoconstrictive effects, thus facilitating easier control of the tissue during surgical procedures [
10].
The choroidal layer is one of the most important structures for nourishing and supplying the retinal structures with blood. The thickness of the choroidal layer is measured by optical coherence tomography (CT), which is a non-radioactive, non-invasive, reliable, and high-resolution imaging method [
1112]. In the CT measurements performed using this method, a decrease in choroidal layer thickness suggests a decrease in the blood supply to the retinal region, whereas an increase in thickness indicates an increase in retinal blood volume [
1314].
In a study by Dogan et al., it was determined that local anesthetics applied to the nasal area resulted in decreased blood supply in the retinal region through measurement of the choroidal layer [
13]. In another study, Berrones et al. evaluated changes in retinal blood flow after the use of sildenafil by measuring choroidal layer thickness [
15].
In this study, we aimed to evaluate the thickness of the choroidal layer, which is important for blood supply in the retinal structures, with respect to the arthrocentesis procedure.
MATERIALS AND METHODS
Twenty patients who underwent arthrocentesis in the Department of Oral and Maxillofacial Surgery of the Faculty of Dentistry at Adiyaman University between April 1st and June 1st, 2018, were included in the study. The study protocol was approved by the Adiyaman University Ethics Committee (Project No: 2018/2-32). In the study, written informed consent was obtained from all patients. CT measurements were performed using optical coherence tomography (Spectralis™ OCT, Version 6.0, Heidelberg Engineering, Germany) in the Department of Ophthalmology, Faculty of Medicine, Adiyaman University. Four different comparisons were made:
- Before arthrocentesis, between the ipsilateral and contralateral regions
- Immediately after arthrocentesis, between the ipsilateral and contralateral regions
- Before and immediately after arthrocentesis (during the period in which the anesthetic effect continues) in the ipsilateral regions
- Before and immediately after arthrocentesis (during the period in which the anesthetic effect continues) in the contralateral regions
Arthrocentesis Procedure and CT Measurements:
Arthrocentesis was performed using a double needle as defined by Nitzan [
1]. At the beginning of the arthrocentesis procedure, 2 cc of 4% articaine hydrochloride with 1/200,000 epinephrine was injected into the upper joint cavity of the TMJ region with dental anesthesia cannulas. Following anesthesia, 2 cannulas (no: 21) were inserted into the upper joint space, and the region was irrigated with ringer lactate (150–200 cc). Finally, sodium hyaluronate was injected into the area, and the procedure was then completed.
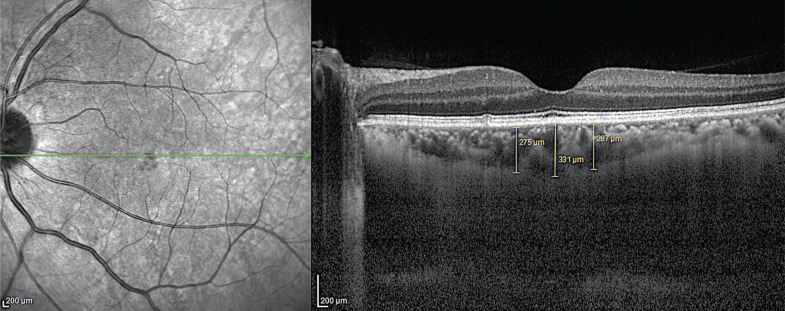
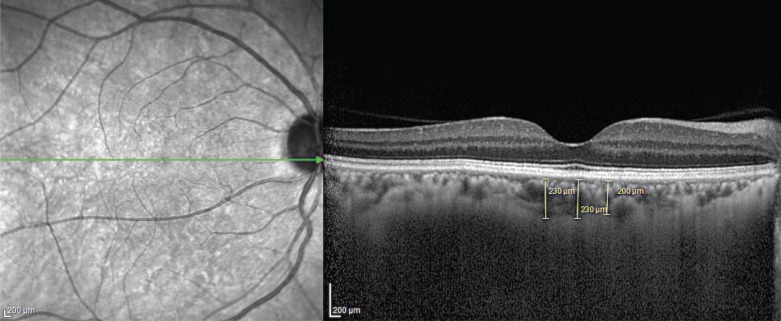
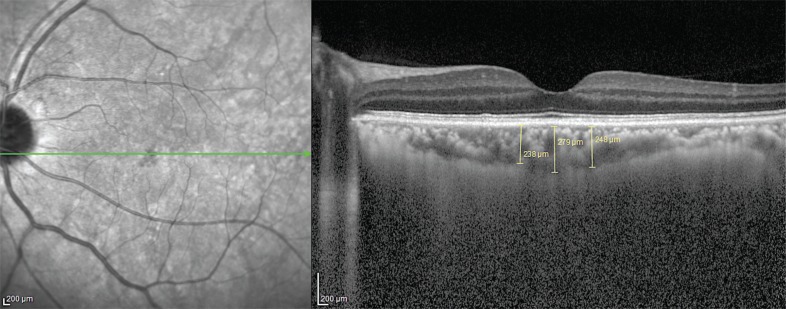
Optical coherence tomography was used to measure the choroidal layer at 3 regions, and the mean values of these 3 regions were used to determine CT values. This procedure was performed before and immediately after arthrocentesis. All measurements are shown in
Figures 1,
2,
3,
4.
1. Statistical analysis
The data obtained in this study were analyzed with the IBM SPSS Statistics Version 22 package program. Because of the number of units, Shapiro Wilk's test was used for analyzing whether the variables had a normal distribution. When interpreting the results, 0.05 was used as the level of significance, with P values greater than 0.05 assumed to display a normal distribution and P values less than 0.05 assumed to display a non-normal distribution.
As the groups were interdependent, the Paired Samples t-test was used for examining the differences between groups when the variables displayed a normal distribution.
When analyzing the relationships and differences between groups, 0.05 was used as the level of significance. P values less than 0.05 were understood to indicate a significant relationship or difference, and P values greater than 0.05 were understood to indicate no significant relationship or difference.
RESULTS
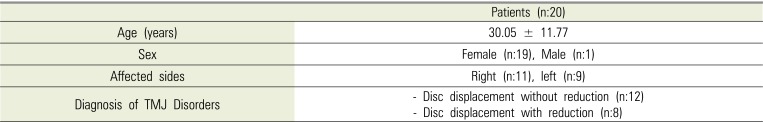
The mean age of the 20 patients who underwent arthrocentesis was 30.05 ± 11.77 years. Of these twenty, 19 patients were female, and 1 patient was male. Eleven of these patients were affected on their right side, while 9 were affected on their left side. Twelve of these patients, who had not responded to conservative treatment, experienced severe pain as well as complete restriction in opening of their mouths (disc displacement without reduction). The other 8 of these patients experienced severe pain, but mouth opening could be achieved by manipulation (disc displacement with reduction). Demographic characteristics of these patients are shown in
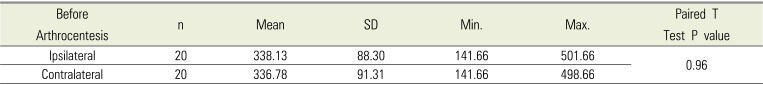
Table 1. There were no systemic or local factors that would prevent carrying out arthrocentesis in these patients. No complications was observed in any patient during as well as after arthrocentesis. In addition, it was observed that patients had less pain and increased mouth opening upon follow-up. In these patients, when CT values were compared between the ipsilateral and contralateral sides before arthrocentesis, the mean CT value for the ipsilateral side was 338.13 ± 88.30, while the mean CT value for the contralateral side was 336.78 ± 91.31. This difference was not statistically significant (
Table 2).
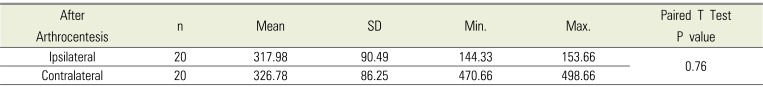
When CT values were compared between the ipsilateral and contralateral sides after arthrocentesis, the mean CT value for the ipsilateral side was 317.98 ± 90.49, while the mean CT value for the contralateral side was 326.78 ± 86.25. This difference was not statistically significant (
Table 3).
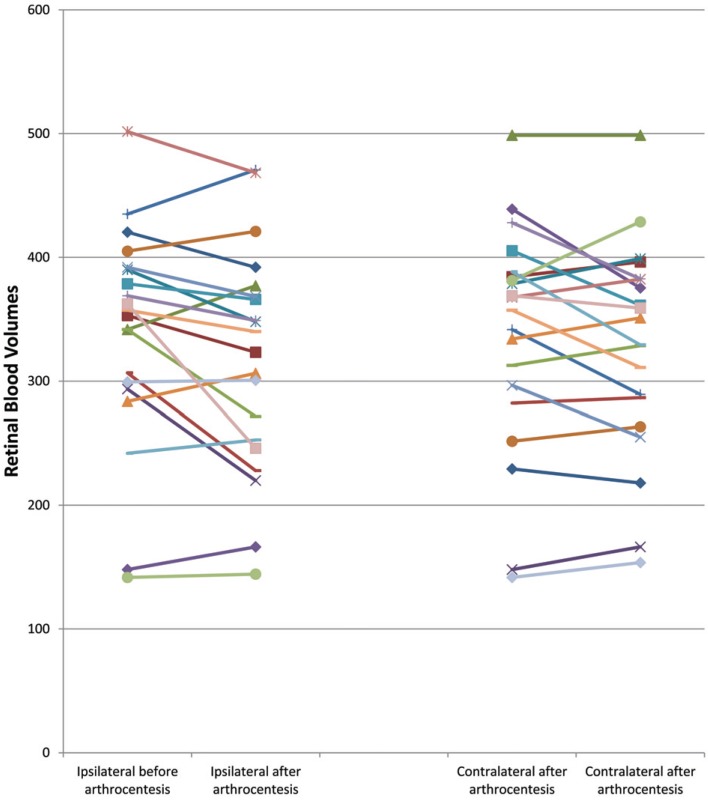
When the retinal blood volume on the ipsilateral side was compared before and after arthrocentesis, CT values were found to decrease from 338.13 ± 88.30 to 317.98 ± 90.49 after the arthrocentesis process. This decrease was statistically significant (
Table 4).
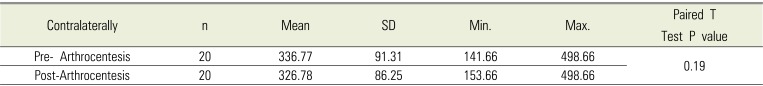
In addition, when CT values were evaluated on the contralateral side before and after the arthrocentesis procedure, CT values were found to decrease from 336.77 ± 91.31 to 326.78 ± 86.25, which was also not statistically significant (
Table 5). These results are shown in the graph in
Fig. 5.
DISCUSSION
TMJ related problems are common in the population [
1617]. When the conservative methods are found to be inadequate in treating these problems, arthrocentesis is usually performed [
34]. Although arthrocentesis is considered to be a minimally invasive surgical procedure, compared to open joint surgery, this procedure can also cause various complications. The TMJ region is adjacent to several anatomical structures, such as the cranial bones, mid-ear equilibrium organs, the facial nerve, the temporal artery, and the parotid gland [
5678]. Complications from arthrocentesis usually stem from two factors, one being the mechanical damage caused by the cannula during arthrocentesis. This damage can include facial nerve injuries, periauricular hematoma, superficial temporal artery bleeding, arteriovenous fistula formation, hemorrhage, or perforation in the intracranial structures and breaking of the cannula in the joint. The second factor is the local anesthesia-induced complications in the arthrocentesis procedure, which include allergic reactions, facial paralysis, vertigo, dizziness, and hearing problems when the middle ear is affected [
581819]. Anesthesia-induced complications usually occur when the anesthetic solution spreads to the surrounding tissues, and these complications were found to be mostly temporary. Therefore, in this study, the effect of local anesthesia performed during arthrocentesis on retinal regions was investigated.
There are few studies looking at the complications caused by local anesthetics in arthrocentesis. Viara et al. reported that 65.1% of patients who underwent arthrocentesis procedures displayed temporary frontal and orbicular oris paresthesia due to anesthesia (433 total arthrocentesis procedures), while 23.5% of these patients had external ear canal problems which lasted less than 1 week [
5]. Senturk et al. observed temporary facial paralysis due to anesthesia in 22.1% of 22 patients who underwent arthrocentesis [
20]. In the study by Yapici, Yavuz et al, 18 complications were observed in 102 arthrocentesis procedures, and 4 of these complications were identified as temporal paresthesia of the facial (n: 2), lingual (n: 1), and inferior alveolar nerves (n: 1) as a result of anesthesia [
8]. In a case report, Vaira et al. reported that vertigo was observed temporarily after arthrocentesis, and it was thought that vertigo could have been caused by the anesthetic effects [
21]. Our study demonstrated that anesthesia decreased blood supply to the retinal structures during the arthrocentesis procedure. CT measurements were performed by optical coherence tomography to measure this retinal blood volume. In the present study, a decrease in CT levels was observed after local anesthesia in the regions where arthrocentesis was performed, and this decrease was statistically significant. In addition, after unilateral procedures, CT levels in the retinal regions were lower in both eyes, but this decrease was not statistically significant. In a study on local anesthetics by Dogan et al., it was shown that anesthetics had bilateral effects on the retina [
13]. This is thought to be due to the abundance of arteries in the cranium. In this study, the vasoconstrictor effects of local anesthetics result in decreased blood supply to the retinal structures, so it is thought that this decrease in retinal blood volume is a temporary effect. In previous studies, it was thought that the complications caused by the anesthetic solution during arthrocentesis were due to the effects of the anesthetic solution spreading to the surrounding tissues. However, in the present study, we report that these complications are due to the vasoconstrictor effects of the anesthetics.
In a study on the ophthalmological complications caused by intraorally applied anesthetics, Von Arx et al. examined the complications (diplopia, enophthalmos, mydriasis, ptosis) on 108 eyes in 65 patients, noting that it is common for anesthetic solutions in maxillofacial regions to affect the eye [
9]. In our study, no complications similar to the ones observed by Von et al. were observed. In one study, Dogan et al. reported that the presence of epinephrine in local anesthetics applied to the nasal area reduced CT, consequently reducing retinal blood supply [
13]. In our case, a temporary decrease in retinal blood supply due to the anesthesia was detected. Epinephrine is usually added to anesthetic agents as a vasoconstrictor agent, as it minimizes systemic toxicity by using less articaine. Thus, more effective anesthesia can be achieved with less articaine [
10]. Verlinde et al. reported that, based on its vasoconstrictor effects, excessive amounts of epinephrine cause ischemic damage by reducing blood flow [
22]. With this knowledge, it was concluded that the decrease in retinal blood volume seen in our study was due to the use of epinephrine together with articaine. Therefore, excessive use of epinephrine should be avoided. In our study, an anesthetic with one of the lowest epinephrine ratios was preferred.
Among anesthetics used in the maxillofacial region, epinephrine is used in different proportions. In the present study, an anesthetic with a low epinephrine ratio was used, with the aim of preventing both the ischemic effects of epinephrine and its systemic damages. One of the limitations of this study was the lack of comparison with anesthetics that do not include epinephrine, which would have enabled us to better understand the effects of epinephrine. However, caution should be taken when using epinephrine-free anesthetics for an operation such as arthrocentesis, where hemorrhaging may increase due to the high cranial blood supply. In addition to the anesthetic agent, ringer lactate and hyaluronic acid were applied in the arthrocentesis procedure. As the decrease in retinal blood supply was temporary, the anesthetic agent was thought to be the most probable cause of this change; however, further studies should be performed to also evaluate the effects of ringer lactate and hyaluronic acid on retinal blood supply. In line with these limitations, it is suggested that further studies be performed on the effects of anesthetics in the arthrocentesis process.
In conclusion, the local anesthesia applied in the arthrocentesis procedure reduces the retinal blood supply in the operated region. The reason for this is thought to be the epinephrine mixed with the local anesthetic solution. Although this effect is temporary, excessive use of local anesthetics containing epinephrine agents should be avoided. In addition, the present study is the first to investigate the change in blood supply in the retinal structures during arthrocentesis.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download