Abstract
Germinoma is the most common type of intracranial germ cell tumors (GCTs). Pineal gland and suprasellar region are the most frequent sites of central nervous system (CNS) involvement. Intracranial masses caused by Langerhans cell histiocytosis (LCH) mimics features of CNS GCTs. LCH frequently involve spine and is the most common cause of vertebra plana in children. A 15-year-old boy presented with progressing symptoms of polydipsia, polyuria, general headache, nausea and severe back pain. Brain MRI showed brain tumor with simultaneous involvement of suprasellar region and pineal gland. An excisional biopsy of suprasellar mass was done. The pathologic assessment confirmed the diagnosis of germinoma. Patient's treatment continued accordingly. A spine MRI, done due to persistent backache, showed a vertebra plana. We reevaluated the primary diagnosis suspecting LCH. Germinoma of CNS was confirmed and a biopsy of vertebral lesion resulted in hemangioma. Thus we report a case of CNS germinoma with co-occurrence of vertebra plana. We emphasized the importance of histopathologic diagnosis of pineal/suprasellar masses and primary investigation of other CNS regions including spine for possible metastasis or comorbidities.
Germinoma is the most common type of intracranial germ cell tumors (GCTs) [1]. The peak incidence is in children and adolescents (age<20), more common in males than females [12]. Asian countries specifically Japan were reported to have the highest rate of incidence [1]. The presentation is associated to tumor's size and location. endocrine changes, visual disturbances and increased intracranial pressure are the most common clinical features [3]. Pineal gland and suprasellar region are the most frequent sites of central nervous system (CNS) involvement and in some cases (6–13%) simultaneous involvement were reported [4].
Pineal and suprasellar masses differential diagnosis include other non-germinoma GCTs (NGGCTs), pituitary adenoma, meningiomas, gliomas, granulomatosis and Langerhans cell histiocytosis (LCH) [567]. LCH is a rare proliferative disorder. Isolated involvement of CNS in LCH is not common [8]. Intracranial masses caused by LCH mimics features of CNS GCTs, e.g., causing diabetes insipidus, therefore a pathologic assessment of lesion prior to treatment is necessary [7]. In addition, LCH frequently involve spine and is the most common cause of vertebra plana (eosinophilic granulomatosis) in children [8].
In this article, we present a case of pineal/suprasellar bifocal germinoma with co-occurrence of vertebra plana.
A 15-year-old boy with a 2-year history of progressing polydipsia, polyuria and long standing neurologic symptoms; general headache with nausea and severe back pain, was admitted to outpatient department of Ghaem Hospital for further evaluations. The back pain was severe and vague mostly placed at thoracic region, causing movement restriction with no radiation to limbs. He denied any disturbances in visual perception, history of seizure or syncope. Neurologic and general examination yielded no further findings.
As the patient was under 18 years old we obtained the written informed consent from patient's parent.
Complete blood count and metabolic tests were unremarkable. Endocrine tests showed decreased insulin-like growth factor 1 (71.79 ng/mL), AM cortisol (0.23 mcg/dL), and adrenocorticotropic hormone (3.92 pg/mL).
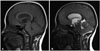
A brain MRI revealed two complex solid-cystic masses, a 17 mm mass located in pineal region and a 15 mm mass in suprasellar region involving the floor of 3rd ventricle. They were irregular, lobulated with solid parts which were enhanced with injection of contrast. A moderate hydrocephalus in 3rd and lateral ventricles were seen. GCT was suggested (Fig. 1, 2).
An excisional biopsy of suprasellar mass by subfrontal transcranial approach was done, pathologic assessment showed atypical cells with large round hyperchromatic nuclei, large nucleoli and clear cytoplasm forming nests surrounded by thin fibrous septa with lymphocytic infiltration consistent with germinoma. Thirty sessions of radiotherapy (RT) with dose of 50 Gy at primary site of tumor was administered. Patient also received medical therapy due to pituitary gland dysfunction.
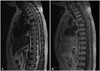
In follow ups the patient complained of persistent back pain. In accordance a thoracic MRI was done; a complete collapse of T5 vertebral body (vertebra plana) with preservation of disk space, moderate spinal cord compression and no associated soft tissue mass was evident (Fig. 3). His RT was stopped and reevaluation of the diagnosis was undertaken with LCH as an important differential diagnosis. Skeletal survey and chest CT scan revealed no lesion. The re-examination of suprasellar biopsy specimens approved primary diagnosis of germinoma. To investigate the origin of vertebra plana (either isolated LCH or metastatic lesion) a biopsy was done. Pathologic assessment showed capillary proliferation of vessels between trabeculae of bone, immunohistochemistry test was positive for CD31 and negative for CD1a and SALL4 which were consistent with diagnosis of hemangioma and both LCH and metastasis from GCT were excluded. Thus the diagnosis was considered bifocal CNS germinoma with co-occurrence of vertebra plana.
GCTs are classified into undifferentiated and differentiated GCTs based on histopathology [9]. Geographical and racial factors had been associated with incidence of CNS GCTs, with higher incidence in Asian countries like Japan, yet findings from recent large studies are inconsistent with prior reports [10]. The peak incidence of germinoma is in the second decade of life and it is more prevalent in males [11].
Extragonadal GCTs are found at midline structures, this include CNS GCTs as well. The most common places are near third ventricle, at pineal gland and suprasellar region [11]. Simultaneous occurrence of germinoma at pineal gland and suprasellar region is reported to comprise 8% of CNS germinoma cases [1]. The clinical manifestation of disease is connected to the age at presentation, size and location of tumor. Suprasellar masses tend to affect anterior and posterior pituitary functions causing growth failure, puberty delay and diabetes insipidus; endocrine deficiencies due to suprasellar masses might be overlooked until neurologic symptoms develop [11]. Signs and symptoms of pineal masses are caused by increased intracranial pressure in regard to hydrocephalous of third ventricle [11]. In the case presented here, the progress of disease and clinical manifestations were highly concordant with suprasellar/pineal bifocal germinoma [411].
Neuroimaging, computed tomography or magnetic resonance, is the first diagnostic step in evaluating a patient with explained presentation [11]. Although germinoma and NGGCTs may often show a difference in enhancement pattern, they cannot be distinguished based on radiographic findings. Elevated serum/cerebrospinal fluid levels of tumor markers beta human chorionic gonadotropin (BhCG) and alpha-feto-protein (AFP) in suspected GCT of suprasellar/pineal region is indicative of secreting NGGCT and as Cuccia and Alderete [4] and Robertson [11] have discussed no further tissue biopsy for histopathologic confirmation is required. Yet in absence of evidence of secreting NGGCT it is necessary to obtain a biopsy because differential diagnosis of a lesion at pineal/suprasellar include variety of neoplasms. In comparison to traditional craniotomy, advances in neuroendoscopy resulted in less aggressive procedure, indirect visualization of the tumor and endoscopic third ventriculostomy in case of significant hydrocephalus [12]. We think in our case, using neuroendoscopy would have been more advantageous with regard to reaching more definitive diagnosis and symptoms relief.
A rare differential diagnosis of pineal/suprasellar mass is LCH. A proliferative disease that may affect different body organs. The most common presentation in CNS involvement is central diabetes insipidus which may be accompanied with headaches and disturbances in vision. Yoon et al. [7] reported a case of 29-year-old woman with pituitary dysfunction and two masses placed at pineal gland and suprasellar region in whom radiographic assessment were in favor of GCT and measured tumor markers were in normal range. Chemo/radiotherapy were administered without tissue diagnosis due to patient's demur; despite initial response to treatment follow ups showed an increase in mass size, an excisional biopsy result showed LCH, no bony and extra-cranial lesion were found [7].
CNS germinoma responds well to RT alone. Substantial late effects of irradiation especially in children and recent findings that reduced dosage of RT to primary site without prophylactic use of craniospinal RT (for localized tumors) can be effectively administered had led to attempts to reach an optimal reduced dosage for treating CNS germinoma [111314]. Some clinical trials investigated the role of neoadjuvant chemotherapy in effectively reducing RT dose and volume, the results showed excellent progression-free survival [111314].
In the case we presented, spinal MRI showed a vertebra plana in T5. Vertebra plana can occur in a variety of conditions, yet LCH is the most common cause of vertebra plana in children [8] with common symptoms of neck or back pain, restricted motion and neurologic symptoms [15]. Therefore, despite histopathologic evidence we reevaluated our diagnosis which as explained in previous section reapproved the primary diagnosis of germinoma for suprasellar mass. Also the biopsy of vertebral lesion showed vertebral hemangioma and not LCH.
Vertebral hemangiomas are the most common benign neoplasms of spinal axis. They are mostly asymptomatic and incidentally found. The diagnosis is usually based on typical radiologic findings, e.g., ‘jail bar’ in plain radiograph, ‘salt and pepper’ in CT and increased intensity on both T1 and T2 of MRI (in contrast to decreased intensity on T1 for metastatic lesions) [1617]. In the case presented here complete collapse of the body (vertebra plana) necessitated the performing of core biopsy to distinguish between metastatic lesion, LCH and other causes of vertebra plana. The management of hemangioma majorly depends on current and expected complications of the lesion (e.g., compression fractures that may result in cord compression). Non-surgical methods such as embolization, vertebroplasty or sclerotherapy and surgical resection should be selected based on each patient's condition [18].
Although there has been reports of gonadal GCTs metastasis to bones [19], to the best of authors' knowledge, there is no report of GCT metastasis causing vertebra plana or a co-occurrence of them. Thus we think we are reporting the first case of co-occurrence of CNS GCT and vertebra plana.
In conclusion, we should emphasize the importance of histopathologic diagnosis of pineal/suprasellar masses and primary investigation of other CNS regions including spine for possible metastasis or comorbidities.
Figures and Tables
Fig. 1
Sagittal T1-weighted (A) and T2-weighted (B) images show two complex solid-cystic masses, a 17 mm mass located in pineal region and a 15 mm mass in suprasellar region.
References
1. Jennings MT, Gelman R, Hochberg F. Intracranial germ-cell tumors: natural history and pathogenesis. J Neurosurg. 1985; 63:155–167.

2. Cuccia V, Galarza M. Pure pineal germinomas: analysis of gender incidence. Acta Neurochir (Wien). 2006; 148:865–871.

3. Echevarría ME, Fangusaro J, Goldman S. Pediatric central nervous system germ cell tumors: a review. Oncologist. 2008; 13:690–699.

4. Cuccia V, Alderete D. Suprasellar/pineal bifocal germ cell tumors. Childs Nerv Syst. 2010; 26:1043–1049.

5. Freda PU, Post KD. Differential diagnosis of sellar masses. Endocrinol Metab Clin North Am. 1999; 28:81–117.

6. Smirniotopoulos JG, Rushing EJ, Mena H. Pineal region masses: differential diagnosis. Radiographics. 1992; 12:577–596.

7. Yoon JY, Park BK, Yoo H, et al. A case of langerhans cell histiocytosis manifested as a suprasellar mass. Brain Tumor Res Treat. 2016; 4:26–29.

8. Chaudhary V, Bano S, Aggarwal R, et al. Neuroimaging of Langerhans cell histiocytosis: a radiological review. Jpn J Radiol. 2013; 31:786–796.

10. McCarthy BJ, Shibui S, Kayama T, et al. Primary CNS germ cell tumors in Japan and the United States: an analysis of 4 tumor registries. Neuro Oncol. 2012; 14:1194–1200.

11. Robertson PL. CNS germ cell tumors: a clinical review and future directions. Future Neurology. 2016; 11:47–62.

12. Morgenstern PF, Souweidane MM. Pineal region tumors: simultaneous endoscopic third ventriculostomy and tumor biopsy. World Neurosurg. 2013; 79:2 Suppl. S18.e9–S18.e13.

13. Bowzyk Al-Naeeb A, Murray M, Horan G, et al. Current management of intracranial germ cell tumours. Clin Oncol (R Coll Radiol). 2018; 30:204–214.

14. Shibamoto Y, Takemoto S. Central nervous system germinoma. In : Mahajan A, Paulino A, editors. Radiation oncology for pediatric CNS tumors. Cham, Switzerland: Springer;2018. p. 263–274.
15. Huang WD, Yang XH, Wu ZP, et al. Langerhans cell histiocytosis of spine: a comparative study of clinical, imaging features, and diagnosis in children, adolescents, and adults. Spine J. 2013; 13:1108–1117.

16. Quinn SF. Vertebral Hemangioma. MRI Web Clinic;2006. at http://radsource.us/vertebral-hemangioma/.
17. Grossman R, Yousem D. Nondegenerative diseases of the spine. Neuroradiology. 3d ed. Philadelphia: Mosby;2003. p. 827–828.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download