Abstract
Backgrounds/Aims
Liver hemangioma, the most common benign liver tumor, can be safely managed by clinical observation. However, surgical treatment should be considered in a subset of patients with giant hemangioma with abdominal symptoms. We reviewed the feasibility of total laparoscopic liver resection for giant hemangioma of >6 cm in diameter.
Methods
Nine consecutive patients who underwent total laparoscopic liver resection for giant hemangioma between August 2008 to December 2012 were included in this study. Medical records were retrospectively reviewed for demographic data, laboratory findings, and perioperative results.
Results
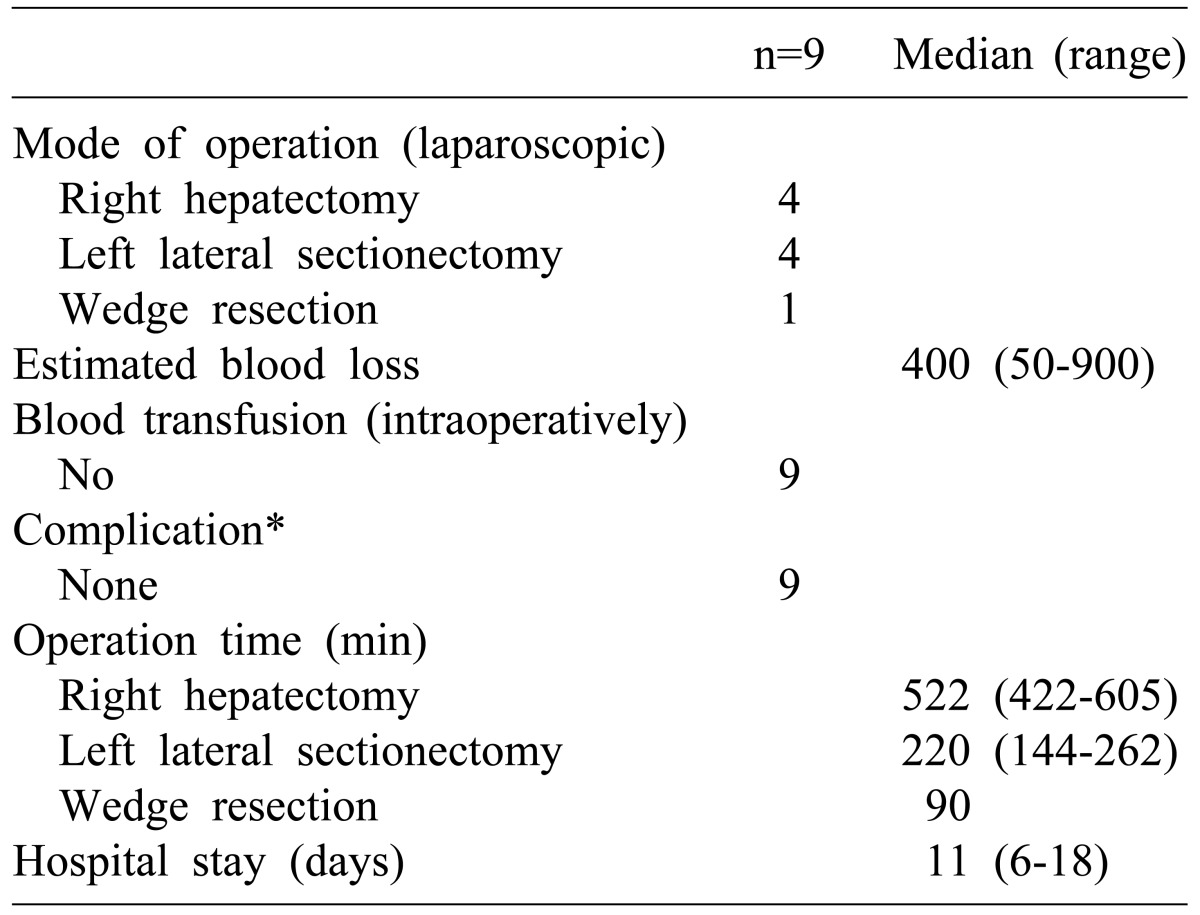
The median age of patients was 36 yrs (range, 31-63). Eight females and 1 male were included in the study. The median size of hemangioma was 11 cm in diameter (range, 6-18) and 5 patients had a hemangioma >10 cm. Indications for surgical treatments were abdominal symptoms in 4 patients, increased size in 5 patients, and uncertain diagnosis in 1 patient. The median operation time was 522 minutes for right hepatectomy, 220 minutes for left lateral sectionectomy, and 90 minutes for wedge resection. The median estimated blood loss was 400 ml (range, 50-900). There was no postoperative morbidity, including Clanvien-Dindo grade I.
Conclusions
The resection of giant hemangioma demands meticulous surgical technique due to high vascularity and the concomitant risk of intraoperative hemorrhage. Laparoscopic liver resection is feasible with minimal operative complication. Therefore, laparoscopic liver resection can be considered as an option for surgical treatment for giant hemangioma.
Liver hemangioma, the most common benign liver tumor, can usually be managed safely by clinical observation.1,2 However, in a subset of patients with giant hemangioma of diameter >4 or 5 cm,3 surgical treatment is justified in high-volume centers if clinical symptoms are present.4,5
The resection of hemangioma demands meticulous surgical technique due to high vascularity and the concomitant risk of intra-operative hemorrhage. Compared to open surgical resection, laparoscopic resection offers many advantages, such as decreased blood loss, shorter hospital stay, improved cosmetic results, and early return to normal life.6 The currently acceptable indications of laparoscopic liver resection are patients with solitary lesions of ≤5 cm diameter located in liver segments 2 to 6. According to The Louisville Statement, giant liver hemangioma (>5 cm diameter) is relatively contraindicated for laparoscopic liver resection.7
Laparoscopic resection of giant hemangioma has been reported previously. However, it has only been reported anecdotally.8 Hemangiomas are more frequent in female patients as benign tumors. Patients requiring surgical treatment would benefit greatly from laparoscopic resection of giant hemangioma if feasible. The aim of this study was to evaluate the feasibility of laparoscopic liver resection for giant hemangioma >6 cm in diameter.
Nine patients (8 females and 1 male) with giant liver hemangioma were referred for liver resection between August 2008 and December 2012. Medical records of patients were retrospectively reviewed for demographic data, laboratory findings, hemangioma size, operation type, operation time, estimated blood loss and perioperative transfusion, complications, and hospitalization duration. Perioperative complications and mortality were assessed over a postoperative period of 6 months.
All but 1 patient (wedge resection) underwent anatomically oriented liver resection. Inflow control of the 'to be resected section' was performed (except for the wedge resection) to reduce the size of the tumor and prevent massive bleeding in case of accidental tearing of the hemangioma. Routine Pringle maneuver was not performed. Such a maneuver was only needed to minimize intraoperative blood loss and ease the operative procedures. Decompression of the hemangioma after resection and prior to retrieval was performed in the last 2 cases to reduce the size of the incision and ease the retrieval of the mass. Total laparoscopic method was the approach in every operation.
The preoperative characteristics of the patients were summarized in Table 1. The median size of hemangioma was 11 cm in diameter (range, 6 to 18 cm) and included hemangioma >10 cm in 5 patients. Indications for surgical treatment in patients were abdominal symptoms in 4 (44.4%), which included dyspepsia, abdominal discomfort, epigastric pain, nausea, and vomiting. Surgical treatment was indicated in 5 (55.5%) patients due to the increasing size of the hemangioma. Diagnosis was uncertain in 1 (11.1%) patient. Hemangiomas with increasing size were 11-18 cm, with a mean increment of 1.67 cm per year.
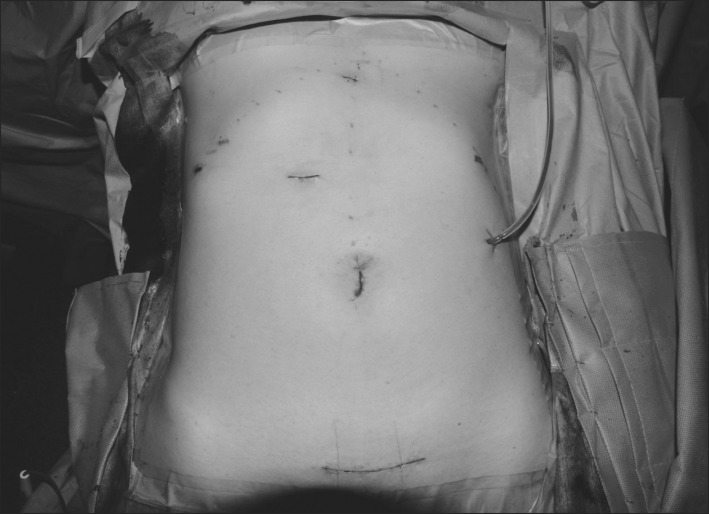
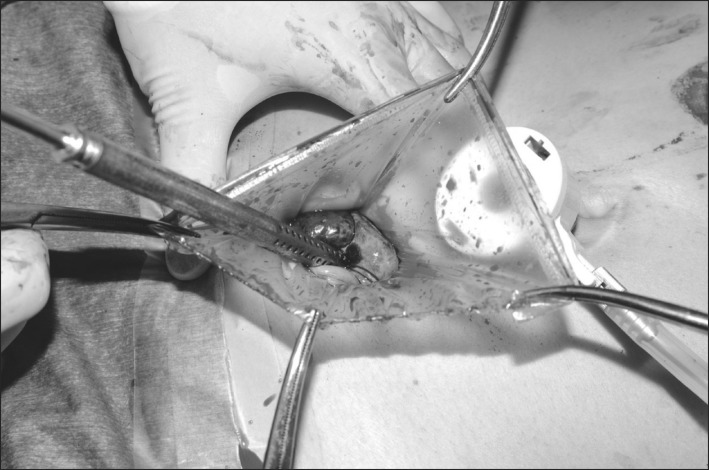
Laparoscopic right hepatectomy was performed in 4 patients. Four patients received left lateral sectionectomy. One patient underwent wedge resection. The median operation time was 522 minutes (range, 422 to 605 minutes) for right hepatectomy, 220 minutes (range, 144 to 271 minutes) for left lateral sectionectomy, and 90 minutes for wedge resection. The operative and postoperative results were described in Table 2. The median estimated blood loss was 400 ml (range, 50 to 900 ml). No patient required blood transfusion. Incision type for specimen retrieval was individually determined based on the previous operation scar and hemangioma size. Pfannenstiel incision, umbilical camera port incision extension, and previous cesarean-section incision were performed on 4, 3, and 2 patients, respectively (Fig. 1). Decompression of hemangiomas during retrieval was performed to decrease the size of incision (Fig. 2). The last 2 cases were performed with decompression. An incision of 8 cm was made on a 13 cm sized giant hemangioma. The incision size was 10 cm for an 18 cm hemangioma. There was no postoperative complication or perioperative mortality, including a Clavien-Dindo classification of surgical complication grade I. The median hospitalization duration was 11 days (range, 6-18 days). There was no correlation between hospitalization duration and the type of operation.
Over the last 2 decades, laparoscopic surgery has evolved to become the preferred approach for many abdominal procedures. Compared to open surgical resection, laparoscopic surgery has several advantages, such as decreased blood loss, shorter hospital stay, improved cosmetic results, and early return to normal life.6,8 Multiple series have reported on the safety and efficacy of laparoscopic liver surgery. Small and medium sized procedures have become commonplace in many centers. Major laparoscopic liver resections have been performed in highly specialized centers with the same efficacy and safety as open surgery.8
Liver hemangioma is a benign tumor. Many studies have demonstrated that clinical observation of patients with giant hemangioma is the standard treatment option in most patients.2 Nevertheless, surgical resection is indicated for patients who have acceptable surgical risk, who have lesions for which a diagnosis is equivocal despite appropriate preoperative evaluation, and who have rapidly increasing sized lesions that cause Kasabach-Merritt syndrome.9 Open enucleation is preferred as a curative treatment by most surgeons, because in open enucleation, maximum amount of normal liver parenchyma is preserved, blood loss is limited, and the risk of bile leak is decreased.10 However, massive blood loss remains a problem for large hemangiomas of >10 cm diameter and for centrally located liver hemangiomas.11
Laparoscopic resection of hemangioma was not recommended as a surgical treatment due to high vascularity and the concomitant risk of intra-operative hemorrhage. Therefore, anatomic liver resection was the chosen method of liver resection in our series with the exception of 1 case in which wedge resection could be easily performed. Safety and efficacy were well demonstrated by median estimated blood loss of 400 ml, no requirement of perioperative blood transfusion and no postoperative complication. Minor surgical complications such as wound infection of grade I or II are documented in a series of resection. However, we had no such minor complications, supporting the minimally invasive nature of the laparoscopic approach.
Two essential operative techniques enhance the feasibility and the outcome. First, it is essential to control the inflow to the section of the liver that has the hemangioma, in the early period of the operation. This step, not only decreases the potential for massive bleeding from the hemangioma, but also increases surgical visibility by decreasing the giant hemangioma, thus making the surgical procedure much easier. The Pringle maneuver should also be performed in a flexible manner to further decrease the amount of bleeding. The second technique is the decompression of hemangioma during retrieval. Hemangioma is a benign disease. Its size can be greatly reduced by extraction of blood inside the tumor and the size of incision was also reduced.
In conclusion, the resection of giant hemangioma demands meticulous surgical technique due to their high vascularity and the concomitant risk of intra-operative hemorrhage. Although laparoscopic approach for tumors >5 cm has not been previously recommended, our results suggested that laparoscopic liver resection may be considered as an option for surgical treatment for giant hemangioma contingent on some surgical precautions and the experience of the surgeon.
References
1. Choi BY, Nguyen MH. The diagnosis and management of benign hepatic tumors. J Clin Gastroenterol. 2005; 39:401–412. PMID: 15815209.

2. Schnelldorfer T, Ware AL, Smoot R, Schleck CD, Harmsen WS, Nagorney DM. Management of giant hemangioma of the liver: resection versus observation. J Am Coll Surg. 2010; 211:724–730. PMID: 20980175.

3. Lise M, Feltrin G, Da Pian PP, Miotto D, Pilati PL, Rubaltelli L, et al. Giant cavernous hemangiomas: diagnosis and surgical strategies. World J Surg. 1992; 16:516–520. PMID: 1589990.

4. Yedibela S, Alibek S, Müller V, Aydin U, Langheinrich M, Lohmüller C, et al. Management of hemangioma of the liver: surgical therapy or observation? World J Surg. 2013; 37:1303–1312. PMID: 23354918.

5. Duxbury MS, Garden OJ. Giant haemangioma of the liver: observation or resection? Dig Surg. 2010; 27:7–11. PMID: 20357445.

6. Katkhouda N, Mason RJ, Towfigh S, Gevorgyan A, Essani R. Laparoscopic versus open appendectomy: a prospective randomized double-blind study. Ann Surg. 2005; 242:439–448. PMID: 16135930.

7. Buell JF, Cherqui D, Geller DA, O'Rourke N, Iannitti D, Dagher I, et al. World Consensus Conference on Laparoscopic Surgery. The international position on laparoscopic liver surgery: the Louisville Statement, 2008. Ann Surg. 2009; 250:825–830. PMID: 19916210.
8. Acharya M, Panagiotopoulos N, Bhaskaran P, Kyriakides C, Pai M, Habib N. Laparoscopic resection of a giant exophytic liver haemangioma with the laparoscopic Habib 4× radiofrequency device. World J Gastrointest Surg. 2012; 4:199–202. PMID: 23293733.

9. Erdogan D, Busch OR, van Delden OM, Bennink RJ, ten Kate FJ, Gouma DJ, et al. Management of liver hemangiomas according to size and symptoms. J Gastroenterol Hepatol. 2007; 22:1953–1958. PMID: 17914976.

10. Lerner SM, Hiatt JR, Salamandra J, Chen PW, Farmer DG, Ghobrial RM, et al. Giant cavernous liver hemangiomas: effect of operative approach on outcome. Arch Surg. 2004; 139:818–821. PMID: 15302689.
11. Hamaloglu E, Altun H, Ozdemir A, Ozenc A. Giant liver hemangioma: therapy by enucleation or liver resection. World J Surg. 2005; 29:890–893. PMID: 15951941.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download