Abstract
Percutaneous transhepatic biliary drainage (PTBD) is safe treatment for biliary decompression given certain indications. However, this is temporary until definitive drainage is established. We report on a 76-year-old lady with recurrent pyogenic cholangitis and PTBD catheter fracture. She had hepatitis B virus-related Child-Pugh class A liver cirrhosis, hypothyroidism, hyperlipidaemia, and previous atrial fibrillation with a background of mild mitral, tricuspid and aortic valvular regurgitation. She had history of laparoscopic cholecystectomy in the past. She was deemed to be a high operative risk and declined hepatic resection. She had undergone multiple endoscopic and percutaneous biliary interventions to control sepsis and stone burden. A bilateral PTBD catheter was left in situ with plans for 3-monthly change. However, she defaulted follow-up and presented 11 months later with complaints of pain over the drain site and inability to flush the right catheter. Abdominal X-ray and computed tomography scans detected right catheter fracture at two places, making three fragments. She underwent percutaneous removal of the proximal fragment by an interventional radiology team. A temporary 4 Fr catheter was inserted to maintain biliary access. Endoscopic removal of the intra-biliary fragments was done the next day. Complete removal was confirmed on fluoroscopy. Finally, the 4 Fr catheter was replaced by a new 12 Fr catheter. The patient was discharged well.
Percutaneous transhepatic biliary drainage (PTBD) is safe treatment for biliary decompression. It is usually done to control acute hepatobiliary sepsis or as a palliation for malignant jaundice. In most instances, PTBD is a temporary procedure prior to definitive intervention. However, PTBD can be left life-long in patients with predicted short life expectancy or prohibitive operative risk. We report on an elderly female patient with multiple comorbidities and recurrent pyogenic cholangitis (RPC) where bilateral PTBD catheters were inserted for sepsis. Thereafter the patient elected to have this left in situ until the catheter fracture warranted admission.
A 76-year-old lady with a history of RPC was admitted with hepatobiliary sepsis. She was deemed to be a high operative risk because of hepatitis B virus-induced Child A liver cirrhosis, hypothyroidism, hyperlipidaemia, and previous atrial fibrillation with a background of mild mitral, tricuspid, and aortic valve regurgitation. She had undergone laparoscopic cholecystectomy previously. She had also undergone multiple prior endoscopic and percutaneous biliary interventions to control sepsis and stone burden. The brushings and cytology from the intrahepatic ducts did not find malignancy. She was offered hepatic resection, but declined because of the high operative risk. She opted for indwelling percutaneous internal-external biliary drains with 3-monthly changes. In the last visit prior to this admission, she was discharged with a 12 Fr internal-external biliary drain (Navarre®; Bard Biopsy Systems, Tempe, AZ, USA) in the right hepatic duct and a 16 Fr drainage catheter (Cook Medical, Bloomington, IN, USA) in the left hepatic duct. The catheters were spigotted on discharge and the patient was taught to flush the catheters once a day with normal saline. However, she defaulted the follow up and was readmitted after 11 months with complaints of pain over the drain site and inability to flush the right catheter. The left drain site was normal. A plain abdominal x-ray revealed fractures of the right PTBD catheter with a normal left PTBD catheter (Fig. 1).
This result was further confirmed by a computed tomography (CT) scan, which showed a break in the right PTBD catheter near the liver capsule, with a 4 cm gap between the ends (Fig. 2), as well as a break at the distal segment. The left PTBD catheter was intact.
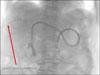
The catheter was fractured at two places with three fragments needing removal. The management of the catheter fracture was performed in stages. Firstly, radiologically guided percutaneous removal of the proximal fragment was performed. Further percutaneous attempt at removal of the middle and distal fragments was unsuccessful, because the strings of the catheter could not be pulled. A temporary 4 Fr Cobra angiographic catheter (Cook Medical, Bloomington, IN, USA) was inserted over the strings of the fractured catheter into the duodenum to drain the right hepatic duct and retain right biliary access. Second, endoscopic retrieval of the remaining fractured fragments (Fig. 3) was done the next day. The intra-biliary catheter fragments were still tied to the duodenal components by the interlocking suture. Thus, all the catheter fragments could be successfully removed by the forceps. At this point, two catheters remained in place: the 4 Fr temporary right biliary access catheter and the 16Fr left biliary access catheter. Last, interventional radiology-guided exchange of the 4 Fr catheter to a 12F internal-external biliary drain (Navarre®; Bard Biopsy Systems, Tempe, AZ, USA) was then done the following day. The successful removal and insertion was confirmed by fluoroscopy (Fig. 4).
RPC is a triad of stones, sepsis, and stricture.1 RPC patients have either definitive surgery performed or permanent metallic biliary endoprosthesis inserted depending on the clinical state. Placement of a PTBD catheter intended to be permanent is a rare clinical need, and for the catheter to fracture is even rarer. Clinical presentation depends on the site of fracture. If left in situ, the retained catheter fragments in the duodenum behave like migrated endoscopically placed biliary stents, and can migrate further into the small bowel, leading to intestinal obstruction. Besides intestinal obstruction, other reported complications of the migrated biliary stents include intestinal perforation, intra-abdominal abscess, and fistula formation.2
We performed a literature search on PubMed with search terms “(percutaneous transhepatic biliary drainage OR biliary catheter OR biliary drainage catheter OR biliary endoprosthesis OR biliary drainage tube) AND (breakage OR catheter fracture OR tube fracture OR fragment OR segment) AND (liver OR bile duct OR biliary system OR bile)” from January 01, 1980 to December 14, 2017. No restriction on language was applied, an ad reference list of all the articles was screened to include additional case reports. A total of 132 reports was generated. Title and abstracts of the reports were screened by first author Kwan JR, and any doubt was clarified by senior author Shelat VG. The findings are presented in Table 1.345678910
In our patient, the fracture was at two sites: (a) at the liver capsule and (b) at the intra-biliary portion. Our patient presented with mild right upper quadrant pain and inability to flush the catheter. It is likely that, because of the prolonged duration, a fistulous track had already matured, and she hence did not develop biliary peritonitis.
We believe that the fracture could have been caused by the catheter becoming brittle over time, leading to spontaneous fracture. In our experience, if there is no catheter fracture, blockage is almost certain after 3 months; so we advocate changing the catheter every 3 months. To prevent early blockage, we advocate daily flushing of the catheter. Plain abdominal radiography is adequate to diagnose catheter migration or fracture, as in our patient. However, a CT scan is warranted to evaluate the underlying pathology, disease progression, or secondary complications that result from the fracture. In our patient, an abdominal film showed a large gap between the two fragments of the catheter.
Management of fractured PTBD includes both preventive and corrective measures for fractured segments and management of the underlying pathology for which the PTBD is inserted. As with our patient, a multidisciplinary approach involving the surgical, medical, and radiological teams is integral to achieving good outcomes. Removal of catheter fragments percutaneously via radiological guidance or via endoscopic retrograde cholangiography should first be considered. Surgical intervention should be the last option if all else fails or if the patient develops biliary peritonitis. In patients requiring a long-term catheter, options of metallic biliary endoprosthesis should be explored. Biodegradable biliary stents are also reportedly used in benign biliary strictures.11 In patients wishing to leave the PTBD for the long term, they should be instructed about the possibility of fracture and to reinforce the need to change the PTBD catheter every 3 months.
In conclusion, this case highlights the importance of close follow-up. Catheters and plastic stents are not designed for long-term use. Therefore it is our institutional recommendation to change catheters every 3 months. Close follow-up of patients who are on PTBD and patient education on regular flushing and catheter care is important to prevent catheter malfunction.
Figures and Tables
Fig. 1
Abdominal X-ray showing intrabiliary fracture of a right percutaneous transhepatic biliary drainage (PTBD) catheter (arrow A) and normal left-side PTBD catheter.

Fig. 2
Computed tomography scan showing fractured right biliary drainage catheter at liver capsule with gap between fragments (arrow B).
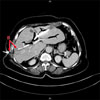
Fig. 3
Endoscopic view of distal fracture fragment (arrow A), intact left PTBD catheter (Arrow B), and temporarily inserted 4 Fr right biliary catheter (arrow C).

References
1. Kwan KEL, Shelat VG, Tan CH. Recurrent pyogenic cholangitis: a review of imaging findings and clinical management. Abdom Radiol (NY). 2017; 42:46–56.

2. Strode MA, Bandera BC, Deveaux P, Rice RD. Migrated biliary stent complicated by small bowel obstruction. Am Surg. 2013; 79:E253–E254.

3. Hsien-Tzu L, Hsiuo Shan T, Nai Chi C, Yi Yang L, Yi You C, Chien An L. Percutaneous transhepatic techniques for retrieving fractured and intrahepatically dislodged percutaneous transhepatic biliary drainage catheters. Diagn Interv Radiol. 2017; 23:461–464.

4. Nghiem DD. Bile leakage after fracture of a percutaneous transhepatic biliary drainage catheter. JAMA. 1984; 251:892.

5. Arai M, Furuya M, Shimizu Y, Okino T, Yokomuro S, Arima Y, et al. A piece of catheter for liver abscess drainage was left in a liver due to fracture: report a case. Tando. 2010; 24:209–212.
6. Luska G, Elgeti H, Lux M. Repeated breaks of polyurethane catheters as a complication of internal bile duct drainage. Rofo. 1981; 135:731–733.
7. Takamatsu S, Nagano H, Ootsukasa S, Kawachi Y, Maruyama H. Ampullary carcinoma associated with removing fractured percutaneous transhepatic biliary drainage catheter for hilar cholangiocarcinoma. HPB. 2016; 18:e472.

8. Jensen LE, Collins Z, Lemons S, Johnson PL. Fracture of Navilyst Exodus biliary catheters. J Vasc Interv Radiol. 2011; 22:261–262.

9. Nennstiel S, Weber A, Frick G, Haller B, Meining A, Schmid RM, et al. Drainage-related complications in percutaneous transhepatic biliary drainage: an analysis over 10 years. J Clin Gastroenterol. 2015; 49:764–770.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download