Abstract
Backgrounds/Aims
Although laparoscopic cholecystectomy is a common and widely accepted technique, the use of prophylactic antibiotics in elective laparoscopic cholecystectomy still remains controversial. The aim of this study is to determine whether prophylactic antibiotics could prevent surgical site infection after elective laparoscopic cholecystectomy and to identify any risk factors for surgical site infection.
Methods
This study included 471 patients undergoing laparoscopic cholecystectomy between January 2009 and May 2012. Period 1 patients (279) received second generation cephalosporin 1 g intravenously after induction of anesthesia, and Period 2 patients (192) were not given prophylactic antibiotics. The characteristics and surgical site infections of the patients were compared and analyzed.
Results
The overall rate of surgical site infection was 1.69% for the total of 471 patients. The incidence of surgical site infection was similar for the two Periods: 5 of 279 patients (1.79%) in Period 1, 3 of 192 patients (1.56%) in Period 2 (p=0.973). All of the patients with surgical site infections were well treated under conservative treatments without any sequelae. The preoperative albumin level (p=0.023) contributed to surgical site infection.
Laparoscopic cholecystectomy (LC) has been the gold standard treatment for symptomatic gallstone disease since 1990.12 The main advantages of LC include less postoperative pain, shorter hospital stays, lower morbidity and mortality, and a lower rate of postoperative infection. Out of the several advantages over open cholecystectomy, an important benefit is the low rate of infective complications (0.4% to 1.1%), mostly occurring at the umbilical port site.3 Because of the low risk of infection, there have been many debates on whether prophylactic antibiotics are necessary.
Currently, many randomized controlled trials (RCTs) have not been able to show any benefit of prophylactic antibiotics in low risk LC.456 However, the statistical power in RCTs has been questioned in some reports, many meta-analysis results do not recommend prophylactic antibiotics in low risk LC as well.37891011 Therefore, more recent guidelines on surgical site infection (SSI) from the Scottish Intercollegiate Guidelines Network (SIGN) and American Society of Health-System Pharmacists (ASHP) do not recommend prophylactic antibiotics in low risk elective LC.1213 But prophylactic antibiotics are still recommended for the high-risk group.
On the other hand, Matsui et al.14 have claimed that underreporting of SSIs may have occurred in previous trials and prophylactic antibiotics should be recommended for LC to reduce SSIs. Recent updates by Centers for Disease Control (CDC) have reported SSIs are now the most common healthcare-associated infection (HAI), accounting for 31% of all HAIs among hospitalized patients.15 With increased awareness of SSIs, criteria for SSI by CDC have been updated to minimize subjective evaluation of the wound and more detailed classifications are now in place.15 With a new guideline by CDC on the way, the role of prophylactic antibiotics should be carefully analyzed with well-gathered data.
The aim of this study was to determine whether prophylactic antibiotics could prevent surgical site infection after elective LC and to identify the high-risk group for SSI.
We retrospectively reviewed medical records of 534 consecutive patients who received elective laparoscopic cholecystectomy at Severance Hospital of the Yonsei University Health System in Seoul, Korea between January 2009 and May 2012 by a single surgeon. Those patients diagnosed with gallbladder empyema or acute cholecystitis were excluded from the study, in total, 63 patients. Diagnoses of patients included gallstones, chronic cholecystitis, gallbladder polyp, and adenomyomatosis. Thus, a total of 471 patients were evaluated and they were divided into two periods. Period 1 was from January 2009 to March 2011. During this period, patients received a routine administration of 1 g of second-generation cephalosporin intravenously after the induction of anesthesia. Prophylactic antibiotic was given only once for each operation. During period 2, from April 2011 to May 2012, patients did not receive any prophylactic antibiotics. There were 279 patients in period 1 and 192 patients in period 2. Data were analyzed between the periods.
Demographic data were collected for all patients, including age, gender, body mass index (BMI), American Society of Anesthesiologists score (ASA score), information on diabetes status, length of hospital stay, operative time, and gallbladder perforation during the operation. The length of hospital stay was defined as the number of days in the hospital from admission to discharge. Clinical characteristics and perioperative results were compared between the two periods.
Preoperative laboratory results were gathered for all patients within 1 month from the operation. The gathered information included white blood cell count (WBC), hemoglobin, creatinine, cholesterol, albumin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), and bilirubin.
All patients underwent operation by a single surgeon. LC was performed using 3-port placements in all cases. A transverse supraumbilical incision was made and a 12 mm camera port was introduced using a Veress needle. Two additional 5 mm working ports were placed under direct vision in the right subcostal and subxiphoid areas.
Examination for SSI was made until hospital discharge and again at the first postoperative visit. All patients were followed up within 7 days from the discharge in the outpatient department and again in 2 months. Postoperative SSIs were defined according to the CDC guidelines.16 Superficial incisional SSI was defined to be an infection involving only skin and subcutaneous tissue of an incision within 30 days of the operation. Additionally, the patient needs to have at least one of the following: purulent discharge from the superficial incision, positive culture result, incision that is deliberately opened by an attending physician with positive culture result, or in cases of cultures not taken, showing signs of inflammation. Diagnosis of superficial incision SSI by the attending physician is also included in the definition.15 Deep incisional SSI was defined to be an infection involving deep soft tissues of the incision; and organ/space SSI was defined to be an infection involving any part of body deeper than the fascial/muscle layers, that is manipulated during the operation.15 According to the definition of the CDC guidelines, a stitch abscess alone with minimal inflammation and discharge confined to the points of suture penetration was not considered a SSI. In a case of SSI, the standard management of wound care was provided: including antibiotics, dressing, or intervention drainage.
Analysis was performed with the Statistical Package for Social Sciences version 20 (SPSS, Chicago, IL, USA). A Shapiro-Wilk test was used to test normality for each quantitative variable. Comparisons between the groups were performed using the Fisher's exact test, or chi-square, as appropriate.
Binary logistic regression was performed to assess risk factors for SSI. The following independent variables were used: antibiotic use, age, sex, BMI, ASA score, WBC, hemoglobin, albumin, AST, ALT, bilirubin, and history of diabetes. SSI was used as the dependent variable. The level of statistical significance was set to be 0.05.
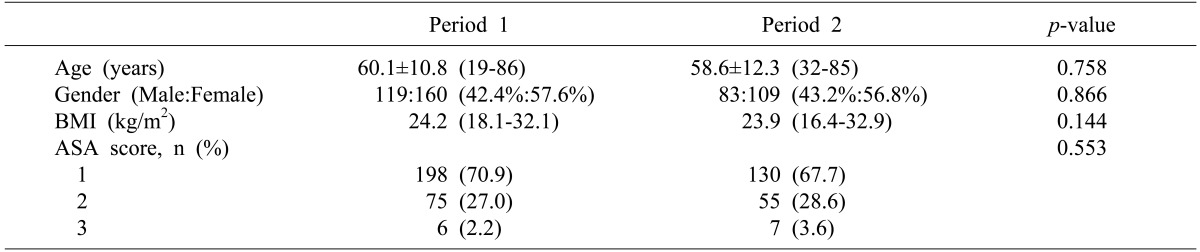
The mean ages of the patients were 60.1±10.8 years for period 1 and 58.6±12.3 years for period 2 (p=0.758). The gender ratio between the two periods showed similar characteristics with male to female ratios of 42.4%: 57.6% in period 1 and 43.2%: 56.8% in period 2. The median body mass indices were 24.2 kg/m2 (range, 18.1-32.1 kg/m2) for period 1 and 23.9 kg/m2 (range, 16.4-32.9 kg/m2) for period 2 (p=0.866). Most patients in the study were of normal weight, in terms of the body mass index. To assess the severity of underlying conditions, the ASA score was used. In period 1, 198 patients (70.9%) had a score of 1 and in period 2, 130 patients (67.7%) had a score of 1. Most patients were in the normal healthy patient category. Only 2.2% in period 1 and 3.6% in period 2 had an ASA score of 3 and no patients had a higher ASA score. A comparison of the baseline characteristics between the two periods showed no significant differences regarding age, sex, body mass index, and ASA score. The clinical characteristics between the two periods are summarized in Table 1.
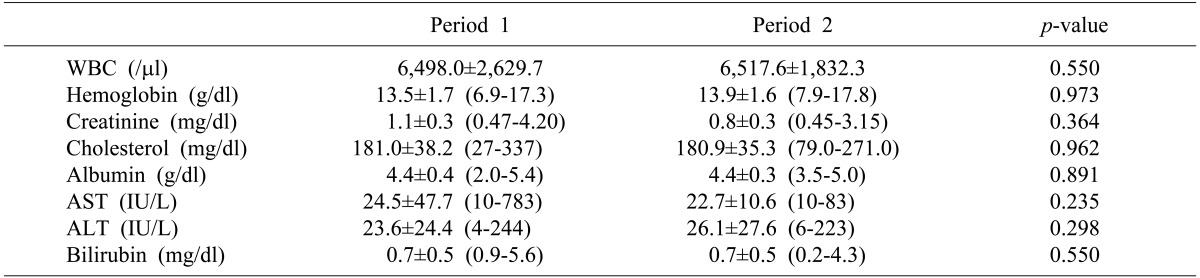
WBC was used to evaluate the presence of an inflammatory condition prior to operation. The results showed a mean WBC of 6498.0±2629.7/ul in period 1, and 6517.6±1832.3/ul in period 2 (p=0.550). No obvious inflammation was present in both groups prior to operation. The mean values of preoperative laboratory results showed that patients were in normal healthy condition without anemia and renal insufficiency. The mean values for albumin and cholesterol also suggested that the patients in both group were in a good nutritional state. The results of AST and ALT values showed normal liver functions prior to operation and mean bilirubin level in both periods were within normal range. Preoperative laboratory results were compared between the periods and the results also showed no significant difference (Table 2).
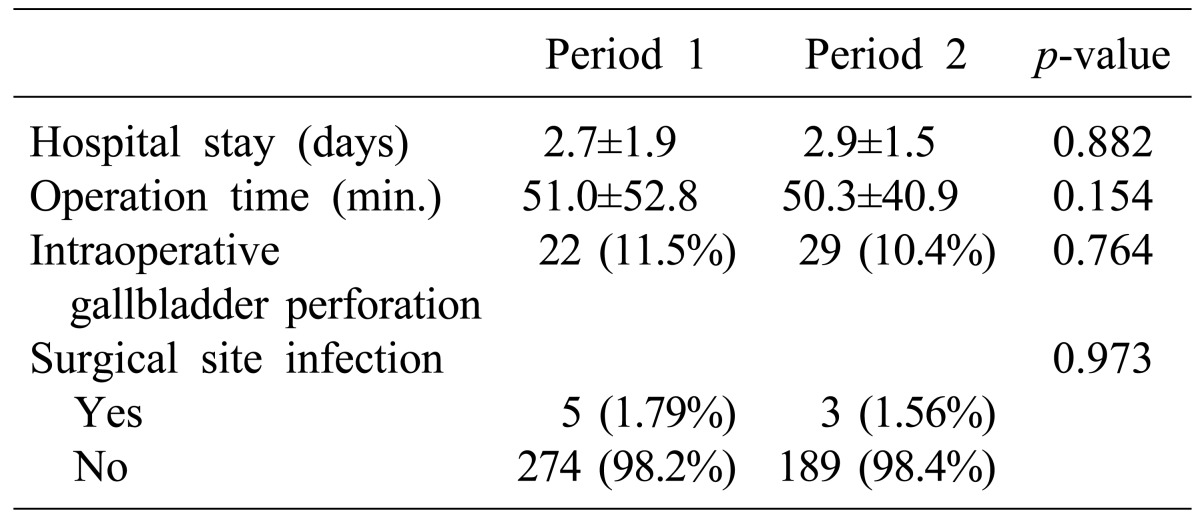
The mean length of hospital stay during period 1 was 2.7±1.9 days and 2.9±1.5 days for period 2 (p=0.882). The total operation time during the two periods was similar with 51.0±52.9 minutes for period 1 and 50.3±40.9 minutes for period 2 (p=0.154). Intraoperative gallbladder perforation also occurred at a similar rate in both periods (11.5% in period 1 and 10.4% in period 2, p=0.764) Postoperative results did not show significant results between the two periods, including mean length of hospital stay, operation time and intraoperative gallbladder perforation (Table 3).
The incidences of SSIs are shown in Table 3. Five (1.79%) patients developed SSIs during period 1 and three (1.56%) in period 2. There was no statistically significant difference in the development of SSI between the periods (p=0.973). SSIs presented during both periods were superficial incisional. All patients, who developed SSIs, were well treated with conservative treatments without any sequelae.
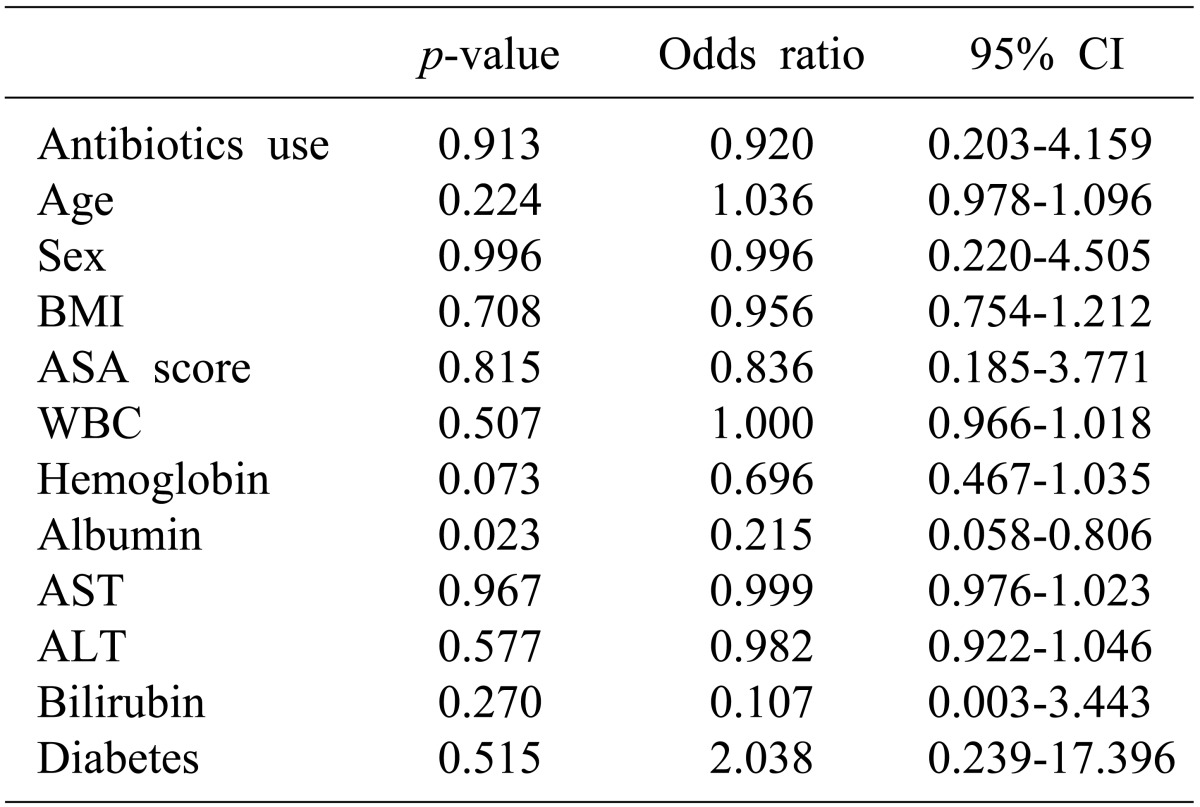
In a further search for risk factors associated with the development of surgical site infection, binary logistic regression analysis was also carried out. With surgical site infection as a dependent variable, only the albumin level showed a significant impact on surgical site infection (p=0.023). Nutritional state may play an important role in SSI. Antibiotic use was shown not to have a significant influence on SSI (p=0.913). The results are summarized in Table 4.
Since the introduction of LC, role of prophylactic antibiotics have been questioned because of low infection rates. Most of the recent randomized trials and their meta-analysis have concluded that low risk elective LC does not require prophylactic antibiotics.34567891011 Our study results concur with these previous trials, thus no benefit of prophylactic antibiotics was found. Despite much evidence on the unnecessity of prophylactic antibiotics in LC, a more recent RCT by Matsui et al.14 has recommended three doses of perioperative antibiotics to reduce SSI in elective low-risk LC. That study emphasized a possibility of overlooked SSIs and inadequate statistical power as the reasons for its discrepancy with previous trials.14 The underreporting of SSIs during follow-up should be carefully addressed in order to obtain a reliable data. Our data was collected from a single surgeon experience and the reporting of SSI properly followed the CDC guidelines to minimize underreporting. SSIs are defined to be infections occurring within 30 days of an operation for LC. However, in this study the follow-up of the patients was not done at 30 days from the surgery. The follow-up was scheduled in the outpatient department at postoperative 7 days and 2 months. In a case of complicated SSI, the patient would return to the outpatient department prior to the scheduled appointment and will be accounted for in the analysis. However, in a minor SSI, the case may have been underreported. This limitation may have influenced the incidences of SSI. To minimize the underreporting of the SSIs for future studies, it is essential to have a more systemic and specific web-based data collection system.
Despite the controversy, current guidelines by SIGN and ASHP do not recommend use of prophylactic antibiotics in low risk LC, as based on the evidence from many RCTs. Nevertheless, prophylactic antibiotics are recommended for the high-risk group. In defining the high-risk group, both guidelines acknowledge bile spillage (intraoperative gallbladder rupture), conversion to laparotomy, acute cholecystitis, jaundice, pregnancy, immunosuppression, and insertion of a prosthetic device.1213 But, intraoperative cholangiogram is considered to be a high-risk only in the SIGN guideline. In the therapeutic guideline by ASHP, the high-risk factors for SSI are considered to be: emergency procedures, diabetes, long procedure duration, age >70 years, ASA score of 3 or higher, and an episode of colic within 30 days before the procedure. These discrepancies in the definition of a high-risk group should be addressed in future studies. Furthermore, our data have also shown nutritional state, in terms of albumin level, as a risk factor for SSI. The preoperative albumin level was similar between the groups, but patients with a higher preoperative albumin level were at a lower risk of SSIs.
Although our data could not confirm the high-risk variables from these guidelines, it is noteworthy to consider nutritional state as a possible risk factor in SSI for LC; thus further evaluation is warranted.
The main limitation of this study includes the lack of statistical power to overcome the type II error. With the incidences of reported SSIs at less than 2%, to have a significance power of 80% and lower limit of a 2-sided 95% confidence interval, more than 4,000 patients are necessary. Our study was based on a single surgeon experience with the intention of properly assessing SSIs to reduce underreporting and compensate for this limitation. Nevertheless, results of low SSI rates in both groups suggest that further study with a sufficiently powered sample size may have a limited value.
When the Center for Disease Control (CDC) first introduced its guideline on SSI in 1999, SSI was reported to be third most common nosocomial infection, accounting for 14 to 16%.16 Since then, many advances have been made in infection control practices. However, the most current definition of SSI by CDC states that SSI is now the most common HAIs, which accounts for 31%.15 Surveillance of SSI has been emphasized in the reduction of SSI risk. With the new CDC guideline on SSI expected soon, definition and surveillance protocol for SSI are being updated. With recent modifications in surveillance of SSI and more awareness, a more refined classification is recommended in the effort to reduce SSIs.
In conclusion, we could not find a benefit of prophylactic antibiotics on surgical site infection in laparoscopic cholecystectomy. SSIs were not associated with an increase in length of hospital stay and patients were well treated with conservative care in the outpatient department. Prophylactic antibiotics are not necessary for elective LC, but patients in poor nutritional state with low albumin level should consider prophylactic antibiotics.
References
1. McMahon AJ, Fischbacher CM, Frame SH, MacLeod MC. Impact of laparoscopic cholecystectomy: a population-based study. Lancet. 2000; 356:1632–1637. PMID: 11089821.

2. Shea JA, Berlin JA, Bachwich DR, Staroscik RN, Malet PF, McGuckin M, et al. Indications for and outcomes of cholecystectomy: a comparison of the pre and postlaparoscopic eras. Ann Surg. 1998; 227:343–350. PMID: 9527056.
3. Choudhary A, Bechtold ML, Puli SR, Othman MO, Roy PK. Role of prophylactic antibiotics in laparoscopic cholecystectomy: a meta-analysis. J Gastrointest Surg. 2008; 12:1847–1853. PMID: 18780131.

4. Harling R, Moorjani N, Perry C, MacGowan AP, Thompson MH. A prospective, randomised trial of prophylactic antibiotics versus bag extraction in the prophylaxis of wound infection in laparoscopic cholecystectomy. Ann R Coll Surg Engl. 2000; 82:408–410. PMID: 11103159.
5. Koc M, Zulfikaroglu B, Kece C, Ozalp N. A prospective randomized study of prophylactic antibiotics in elective laparoscopic cholecystectomy. Surg Endosc. 2003; 17:1716–1718. PMID: 12802644.

6. Kuthe SA, Kaman L, Verma GR, Singh R. Evaluation of the role of prophylactic antibiotics in elective laparoscopic cholecystectomy: a prospective randomized trial. Trop Gastroenterol. 2006; 27:54–57. PMID: 16910066.
7. Al-Ghnaniem R, Benjamin IS, Patel AG. Meta-analysis suggests antibiotic prophylaxis is not warranted in low-risk patients undergoing laparoscopic cholecystectomy. Br J Surg. 2003; 90:365–366. PMID: 12594674.

8. Catarci M, Mancini S, Gentileschi P, Camplone C, Sileri P, Grassi GB. Antibiotic prophylaxis in elective laparoscopic cholecystectomy. Lack of need or lack of evidence. Surg Endosc. 2004; 18:638–641. PMID: 14752639.

9. Sanabria A, Dominguez LC, Valdivieso E, Gomez G. Antibiotic prophylaxis for patients undergoing elective laparoscopic cholecystectomy. Cochrane Database Syst Rev. 2010; (12):CD005265. PMID: 21154360.

10. Yan RC, Shen SQ, Chen ZB, Lin FS, Riley J. The role of prophylactic antibiotics in laparoscopic cholecystectomy in preventing postoperative infection: a meta-analysis. J Laparoendosc Adv Surg Tech A. 2011; 21:301–306. PMID: 21443433.

11. Zhou H, Zhang J, Wang Q, Hu Z. Meta-analysis: Antibiotic prophylaxis in elective laparoscopic cholecystectomy. Aliment Pharmacol Ther. 2009; 29:1086–1095. PMID: 19236313.

12. Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 2013; 70:195–283. PMID: 23327981.

13. SIGN. Antibiotic prophylaxis in surgery. Scottish Intercollegiate Guidelines Network (SIGN) Guidelines 104. Edinburgh, UK: SIGN;2008.
14. Matsui Y, Satoi S, Kaibori M, Toyokawa H, Yanagimoto H, Matsui K, et al. Antibiotic prophylaxis in laparoscopic cholecystectomy: a randomized controlled trial. PLoS One. 2014; 9:e106702. PMID: 25192389.

15. CDC. Surgical site infection event. Atlanta, GA: Centers for Disease Control and Prevention;2015.
16. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for Prevention of Surgical Site Infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999; 27:97–132. PMID: 10196487.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download